Fig. 9—
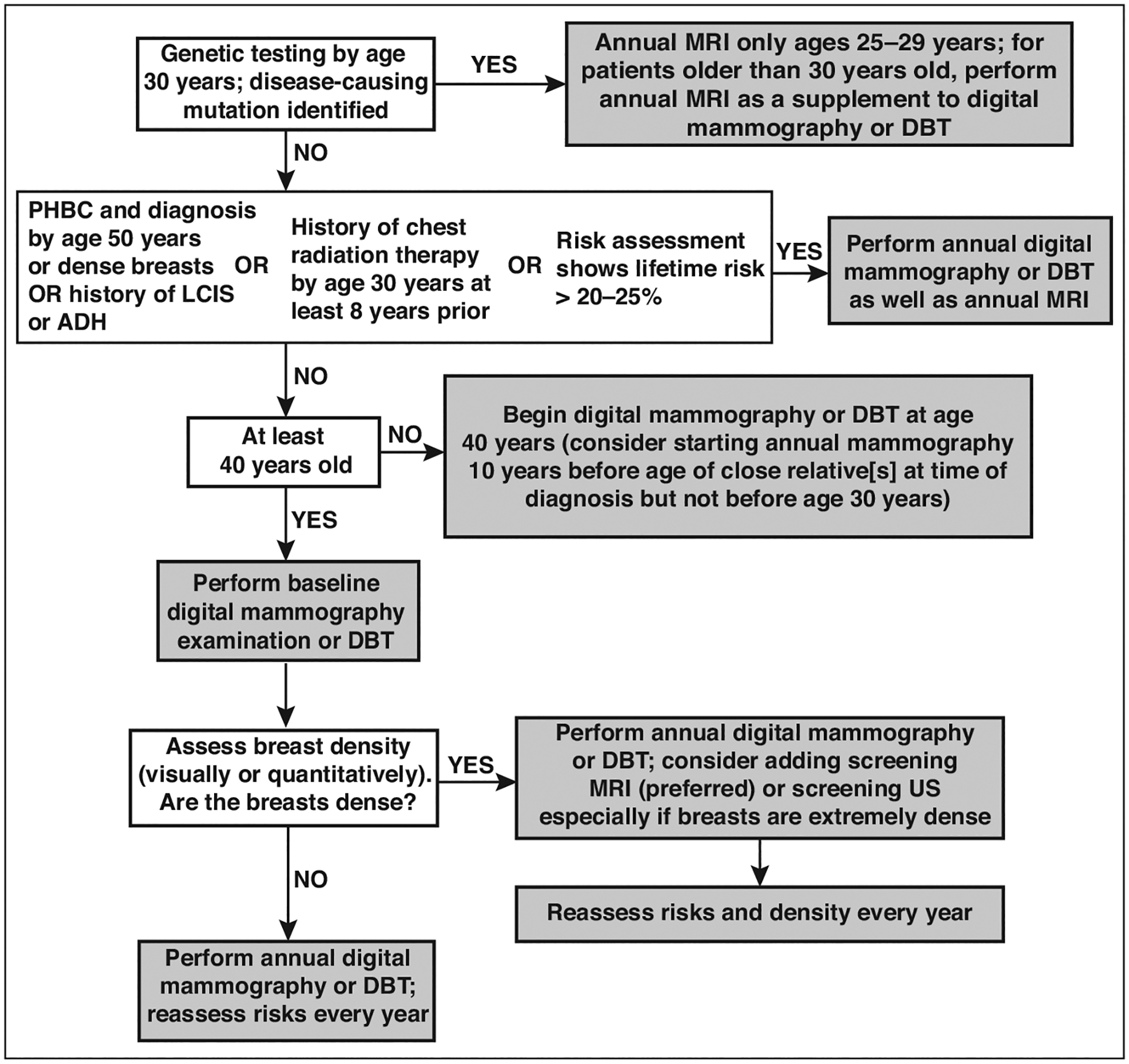
Flowchart illustrates current approaches to supplemental screening in context of risk factors, including breast density. If not performed by age 30 years, genetic testing can be performed at time of diagnosis of breast or ovarian cancer, when appropriate family history is identified, or when family member is found to have pathogenic mutation. Women with high risk for breast cancer who are pregnant or lactating may consider screening ultrasound (US) during that time. Similar performance has been observed for abbreviated MRI and full-protocol diagnostic MRI. For women who cannot tolerate MRI, US is most widely available alternative but produces less gain in cancer detection than MRI. Molecular breast imaging (MBI) or contrast-enhanced mammography (CEM) appear to produce cancer detection similar to that of MRI but are not yet widely available alternatives when MRI is not possible; further validation is needed. If screening MRI is performed, additional supplemental screening with US, MBI, or CEM is not needed. Supplemental screening MRI should stop by age 75 even among high-risk women. PHBC = personal history of breast cancer, LCIS = lobular carcinoma in situ, ADH = atypical ductal hyperplasia, DBT = digital breast tomosynthesis.
