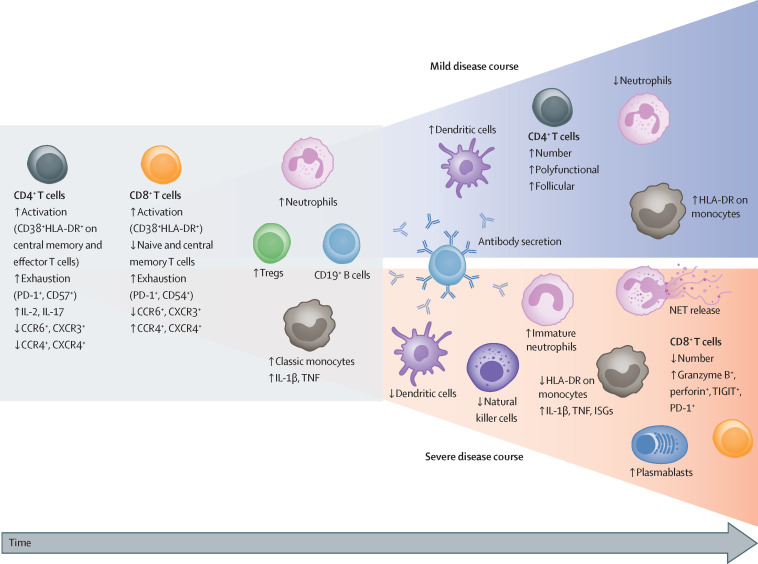
Figure 3.
Severity-dependent changes in peripheral blood immune cells during COVID-19
COVID-19 is associated with a marked decrease in circulating effector CD4+ and CD8+ T lymphocytes, leading to an increase in Tregs. In addition to a numerical loss, the high proportion of exhausted and suppressed T cells expressing CTLA-4, PD-1, or TIGIT suggest compromised T-cell immunity. Both CD4+ and CD8+ T cells show early upregulation of activation markers such as CD38 and HLA-DR concurrent with an altered chemokine receptor pattern (a decrease in CCR6 and CXCR3). Circulating CD4+ T cells are skewed towards an IL-2 and IL-17-positive profile. Early in the course of COVID-19, the numbers of B cells and monocytes remain unchanged, whereas mild neutrophilia is frequently observed. Blue area: patients with favourable outcomes have an increased number of circulating dendritic cells and intermediate monocytes that upregulate HLA-DR expression, suggesting recovery of immunocompetence. T-cell numbers recover with an increase in polyfunctional and follicular helper T cells. These changes are accompanied by a humoral antibody response produced by activated and expanded B cells. During recovery, neutrophil numbers normalise. Red area: a more severe disease course is characterised by a decrease in dendritic cells, natural killer cells, and monocytes; monocytes further downregulate HLA-DR expression but upregulate IL-1β, TNF, and ISGs. Although low in number, CD8+ T cells in severe COVID-19 show substantial upregulation of their effector molecules, such as granzyme B and perforin. Of note, the numbers of B cells decrease, whereas plasmablasts are increased in the blood; specific antibodies are also produced in patients with severe COVID-19. Profound changes occur among myeloid cells including egress of immature neutrophils and myeloid-derived suppressor cells from the bone marrow, and enhanced formation of NETs. NET formation is likely to be an important contributor to the development of organ and endothelial injury in conjunction with activation of the complement and coagulation cascades. CCR=C-C chemokine receptor. CTLA-4=cytotoxic T-lymphocyte protein 4. CXCR=C-X-C chemokine receptor. HLA-DR=HLA DR isotype. IL=interleukin. ISGs=interferon-stimulated genes. NETs=neutrophil extracellular traps. PD-1=programmed cell death 1. TIGIT=T-cell immunoglobulin and ITIM domain. TNF=tumour necrosis factor. Tregs=regulatory T cells.