Abstract
Ascending aortic pseudoaneurysms following open-heart surgery are treated by redo surgery or endovascular therapy when surgical risks are high. Extreme variations in their morphology, proximity to coronary and arch branches and vascular access may vary the timing, strategy, device choice, and technique in each patient. Three patients with varying etiology, presentations, and morphology of the pseudoaneurysms underwent successful endovascular exclusion by individually tailored strategies. The approach includes optimal treatment of the underlying infections before the endovascular intervention despite the emergency to treat the condition; choosing appropriate device depending on the proximity to aortic branches, choosing appropriate access depending on the angulation of the entry of pseudoaneurysm to the aortic lumen, and use of adequate imaging for achieving procedural success.
<Learning objective: A tailored approach for transcatheter closure of postsurgical ascending aortic pseudoaneurysms should include: 1 Optimal infection control before the intervention. 2 Choosing nitinol occluders in high-flow aneurysms; vascular plugs and coils for residual leaks; and embolic protection for high clot burden. 3 Choice of femoral, brachial, or transapical access is decided based on angulation of the aneurysm with ascending aorta. 4 Meticulous planning of the interventions based on advanced three-dimensional imaging.>
Keywords: Nitinol occluders, Covered stents, Embolic protection devices, Vascular access, Infections
Introduction
Ascending aortic pseudoaneurysms that complicate 1–5% of aortic valve and ascending aortic surgeries are challenging and force clinicians to seek transcatheter options [1]. These large aneurysms are closed by nitinol occluders [2,3]. Their diverse morphology and proximity to coronary and arch branches need pre-procedural planning for choosing vascular access and delivery sheaths [4]. If covered stents or stent grafts are used, planning is imperative to prevent and address endoleaks [5]. Catheter manipulations within thrombus-lined pseudoaneurysms may need cerebral embolic protection [6]. The clinical presentations, underlying pathology, aneurysm morphology, and tailored transcatheter strategies for three different forms of postsurgical ascending aortic pseudoaneurysms are described to highlight the decision-making process.
Case series
The institutional review board discussed each patient and approved transcatheter closure.
Case 1
Coronary artery bypass grafting with mammary and venous grafts for triple vessel coronary artery disease in a 65-year-old diabetic hypertensive male was complicated with pseudomonal urosepsis and mediastinitis, needing surgical debridement and six weeks of parenteral antibiotics. When he presented three months later with a non-healing sternal wound with persisting infection, a computed tomogram showed sternal osteomyelitis along with an irregular large ascending aortic pseudoaneurysm. An extensive sternal excision with omentoplasty along with bovine pericardial repair of pseudoaneurysm was done on femoral cannulation and total circulatory arrest. No residual aneurysm was seen in an immediate postoperative computed tomogram. However, he presented again a few months later with Pseudomonas on blood culture and a recurring aortic pseudoaneurysm on echocardiography. Positron emission tomography showed a metabolically active thickened ascending aortic wall. A multidisciplinary team decided to continue conservative management with a prolonged course of antibiotics. After a complete eradication of infection with four months of parenteral antibiotics and normalization of inflammatory biomarkers, a repeat computed tomography showed a large 56 mm wide-mouthed aneurysm with a circular neck measuring 21 mm. Transcatheter closure was considered instead of a third surgery. The mouth of the aneurysm was too low in the ascending aorta precluding a stable placement of a long sheath from femoral arterial access. A left brachial arterial access was considered as the best possible route if the left arm was hyperabducted to bring the left brachial artery in line with the ascending aorta. A 12F long sheath was placed into the aneurysm. The pseudoaneurysm was closed using a 28 mm Amplatzer septal occluder (Abbott, Plymouth, MN, USA) (Fig. 1, Video 1). The left brachial artery access was surgically repaired. He was asymptomatic with stable device position completely sealing the pseudoaneurysm on a computed tomogram after 30 months of follow-up.
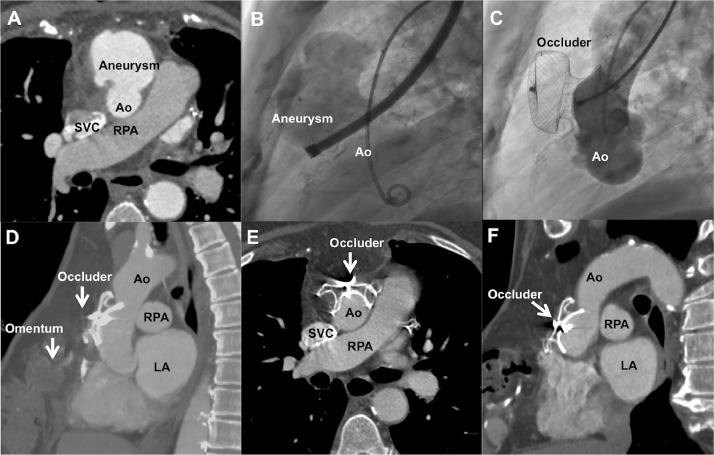
Fig. 1.
Recurrent aortic pseudoaneurysm. Recurrence after bovine pericardial patch repair of ascending aortic (Ao) pseudoaneurysm with sternal debridement and omentoplasty is shown in axial computed tomography (A). Angiogram from a large sheath advanced from the left brachial artery delineates the large pseudoaneurysm from the anterior wall of ascending aorta (Video 1) on lateral view aortogram (B) that is closed by an atrial septal occluder (C). Sagittal (D), axial (E), and long-axis (F) computed tomography images after 30 months confirms complete closure. LA, left atrium; SVC, superior vena cava; RPA, right pulmonary artery.
Case 2
A 61-year-old diabetic male presented with neck pain with a pulsatile mass behind the right clavicle, leukocytosis, and elevated erythrocyte sedimentation rate. Imaging showed a large aneurysm of the innominate artery up to the ascending aorta. Double vessel coronary artery disease warranted a coronary artery bypass grafting with a mammary and a venous graft. During surgery, the right common carotid, right subclavian, and right vertebral artery origins were seen to arise from the intense inflammatory saccular aneurysm. The aneurysm was repaired using a 10 mm Gore-Tex graft (Gore Medical, Flagstaff, AZ, USA) and the right common carotid, subclavian, and vertebral artery origins were anastomosed to the distal end of this graft as a single island. He was treated for Salmonella grown from the culture of the explanted aneurysmal vessel wall. On one-month follow-up, he developed a large 8 cm pseudoaneurysm near the distal anastomosis, without any evidence of residual infection. A redo-surgery through a repeat sternotomy was aborted midway during surgery as the thin walled aneurysm extended beneath the right clavicle. An angiogram showed a wide-mouthed aneurysm from an anastamotic dehiscence. The aneurysm filled antegrade from the aortic arch and retrograde from the right subclavian artery through vertebral steal. An 8F Flexor sheath (Cook Medical, Bloomington, IN, USA) was placed from right femoral artery through the graft into the right carotid artery to position a 10 mm x 58 mm Life-stream covered stent (Bard endovascular, Tempe, AZ, USA) and exclude the aneurysm from its antegrade flows. A 6F Flexor sheath was placed from right brachial artery to deploy multiple Gianturco embolization coils (Cook Medical) and a 16 mm Amplatzer vascular plug II (Abbott) at origin of the left subclavian artery to close retrograde flows (Fig. 2, Video 2). The right brachial artery systolic pressures reduced by 30 mmHg after the occlusion of the left subclavian artery. Final angiogram showed complete seal of the aneurysm. On 24-month follow-up, computed tomography showed no residual pseudoaneurysm.
Fig. 2.
Innominate artery pseudoaneurysm. Axial (A) and coronal (B) tomograms show a large right innominate artery (RIA) pseudoaneurysm following a distal anastamotic blowout after a graft repair. Angiogram (C) from a long sheath placed in the surgical graft fills the aneurysm (Video 2). After deploying a covered stent graft from innominate artery to right carotid artery, endoleak from right subclavian artery is closed from right brachial sheath (D) using a vascular plug. Digital subtraction shows complete closure of aneurysm (E) and subclavian artery filling through vertebral steal (F). Axial (G) and coronal (H) tomograms after two years show complete occlusion. Ao, aorta.
Case 3
Following aortic valve replacement with a mechanical prosthesis in a 59-year-old hypertensive male for severe calcific bicuspid aortic valve stenosis, echocardiography during a routine one-year review identified a large ascending aortic pseudoaneurysm causing extrinsic compression of the main pulmonary artery. Computed tomography showed a massive 10 cm partially thrombosed pseudo-aneurysm with a 12 mm mouth from the aortic bypass cannulation site, located 6 mm proximal to the origin of the innominate artery. There was no evidence of infection. An aortogram through femoral arterial route delineated the anteriorly arising pseudoaneurysm. Two Filterwire EZ carotid filters (Boston Scientific, Natick, MA, USA) provided cerebral protection from a migrating thrombus from the aneurysm. The pseudoaneurysm was cannulated using a right Judkins catheter through the femoral arterial access and an 8F long sheath was parked in the pseudoaneurysm. A 14 mm Amplatzer Muscular VSD device (Abbott) was deployed across the mouth of the pseudoaneurysm. Aortogram showed complete closure of the mouth of the defect (Fig. 3, Video 3). At 15-month follow-up, there were no residual flows on tomographic imaging and no evidence of right arm ischemia.
Fig. 3.
Pseudoaneurysm in bicuspid aortopathy. Axial (A), sagittal (B), and coronal (C) slices of computed tomogram show a clot-lined large aortic (Ao) pseudoaneurysm, causing extrinsic compression of the pulmonary trunk (PA). Angiogram (Video 3) shows the aneurysm (D). Axial (E), sagittal (F), and coronal (G) slices of computed tomogram done 15 months after occlusion of the pseudoaneurysm using a muscular ventricular septal occluder device (H) show a complete closure and relief of the extrinsic pulmonary artery compression. LV, left ventricle; RV, right ventricle.
Discussion
Pseudoaneurysms from the aortic suture lines are partially contained by surgical adhesions, enlarge rapidly, and lead to hemodynamic collapse. When infections cause these pseudoaneurysms, optimal antibiotics are vital before endovascular therapy [1]. Inherent aortic weakness in bicuspid aortopathy is another predisposing factor [7]. Endovascular therapy is chosen as an alternative to high-risk surgery on circulatory arrest [8].
Acute angulation of a large mouthed pseudoaneurysm from the ascending aorta poses difficulties for sheath and device positioning. Atrial septal occluders with large retention skirts are preferred in very large mouthed aneurysms, but encroach on aortic branches [1]. Muscular ventricular septal occluders with smaller retention skirts may risk embolization [9]. Sheaths with an additional curve and oversized devices will prevent malalignment when deploying large devices perpendicular to the vessel long-axis [3,4].
If occluders are not suitable for pseudoaneurysms, endovascular stent grafts may be used [5]. The pseudoaneurysm involving innominate artery received antegrade seal with a covered stent and retrograde seal with coils and plugs, preventing endoleaks. Even though vertebral steal was seen after subclavian artery exclusion, it did not result in arm ischemia. Positioning an additional brachial catheter in the pseudoaneurysm for a ‘coil & plug’ technique was the key to seal the endoleaks into the aneurysm completely [10].
Catheter manipulation in a pseudoaneurysm poses a real risk of cerebral embolism to warrant embolic protection devices [9]. Optimal understanding of aneurysm morphology and hardwares help these procedures. Long-term follow-up data will help in developing further technical finesse in these evolving new technologies on high-risk patients. A tailored transcatheter approach to postsurgical pseudoaneurysms should include optimal infection control, correct choice of devices and vascular access, and use of appropriate imaging
Declaration of Competing Interest
There are no competing interests.
Acknowledgments
Acknowledgments
None.
Funding
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jccase.2020.11.009.
Appendix. Supplementary materials
References
- 1.Kanani RS, Neilan TG, Palacios IF, Garasic JM. Novel use of Amplatzer septal occluder device in percutaneous closure of ascending aortic pseudoaneurysms. A case series. Cath Cardiovasc Interv. 2007;69:146–153. doi: 10.1002/ccd.20794. [DOI] [PubMed] [Google Scholar]
- 2.Miguel B, Camilleri L, Gabrillargues J, Macheda B, Kubota H, Ravel A, De Riberolles C, Boyer L. Coil embolization of a false aneurysm with aorto-cutaneous fistula after prosthetic graft replacement of the ascending aorta. Eur J Radiol. 2000;34:57–59. doi: 10.1016/s0720-048x(99)00094-7. [DOI] [PubMed] [Google Scholar]
- 3.Bashir F, Quaife R, Carroll JD. Percutaneous closure of ascending aortic pseudoaneurysm using Amplatzer septal occluder device: the first clinical case report and literature review. Catheter Cardiovasc Interv. 2005;65:547–551. doi: 10.1002/ccd.20422. [DOI] [PubMed] [Google Scholar]
- 4.Kpodonu J, 3rd Wheatley GH, Ramaiah VG, Rodriguez-Lopez JA, Strumpf RK, Diethrich EB. Endovascular repair of an ascending aortic pseudoaneurysm with a septal occluder device: mid-term follow-up. Ann Thorac Surg. 2008;85:349–351. doi: 10.1016/j.athoracsur.2007.06.053. [DOI] [PubMed] [Google Scholar]
- 5.Roselli EE, Idrees J, Greenberg RK, Johnston DR, Lytle BW. Endovascular stent grafting for ascending aorta repair in high-risk patients. J Thorac Cardiovasc Surg. 2015;149:144–151. doi: 10.1016/j.jtcvs.2014.07.109. [DOI] [PubMed] [Google Scholar]
- 6.Seeger J, Gonska B, Otto M, Rottbauer W, Wöhrle J. Cerebral embolic protection during transcatheter aortic valve replacement significantly reduces death and stroke compared with unprotected procedures. JACC Cardiovasc Interv. 2017;10:2297–2303. doi: 10.1016/j.jcin.2017.06.037. [DOI] [PubMed] [Google Scholar]
- 7.Santini F, Telesca M, Bertolini P, Tomezzoli A, Schiavo N, Faggian G, Mazzucco A. Precocious giant pseudoaneurysm of an "innocent" ascending aorta after bicuspid aortic valve replacement redo. Ann Thorac Surg. 2008;86:e1. doi: 10.1016/j.athoracsur.2008.04.062. [DOI] [PubMed] [Google Scholar]
- 8.D'Attellies N, Diemont FF, Julia PL, Cardon C, Fabiani JN. Management of pseudoaneurysm of the ascending aorta performed under circulatory arrest by port-access. Ann Thorac Surg. 2001;71:1010–1011. doi: 10.1016/s0003-4975(00)02265-7. [DOI] [PubMed] [Google Scholar]
- 9.Noble S, Ibrahim R. Embolization of an Amplatzer mVSD occluder device used for percutaneous closure of an ascending aortic pseudoaneurysm: case report and literature review. Catheter Cardiovasc Interv. 2012;79:334–338. doi: 10.1002/ccd.23094. [DOI] [PubMed] [Google Scholar]
- 10.Khanji MY, Kumar P, Ionescu A. Ascending aortic pseudo-aneurysm treated with 'coil and plug'. Eur Heart J Cardiovasc Imaging. 2017;18:1299. doi: 10.1093/ehjci/jex179. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.