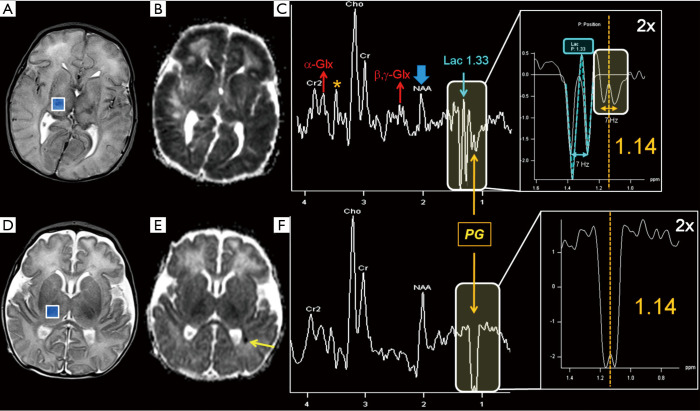
Figure 12.
Top row: 5-day-old female full-term newborn, without a history of hypoxic-ischemic encephalopathy, developing on day 2 after birth repeated seizures, resistant to phenobarbital and phenytoin treatment. In conventional imaging diffuse bihemispheric edema was seen (A, axial T2-WI); DWI ADC maps (B) showed symmetric restricted diffusion in the cerebral cortex, subcortical WM, basal ganglia, and thalami, with sparing of the cerebellum (not shown). In most voxels of the intermediate TE 2D-CSI grid (right thalamo-capsular voxel depicted in A), along with a marked reduction of NAA (thick blue arrow in C) and a moderate increase of α,β,γ-Glx peaks (thin red arrows in C), two adjacent inverted doublets (labeled respectively in light blue and orange in C) with a J-coupling constant of ~7 Hz were seen: the peak centered at 1.14 ppm (separated from the prominent Lac peak at 1.33 ppm), was assigned to propylene glycol (PG), the solvent used for phenobarbital and phenytoin parenteral administration. An encephalopathy due to sulfite oxidase deficiency was hypothesized, and then confirmed. The peaks at the chemical shift range of 3.4–3.6 ppm could not be unequivocally assigned because of the possible overlap of Tau, m-Ins, and S-sulfocysteine with the other known singlet peaks of PG (orange asterisks in C). Bottom row: 8-day-old male full-term newborn with hypoglycemia, severe hypotonia, respiratory acidosis and convulsive status epilepticus treated with phenobarbital. Conventional imaging (axial T2-WI in D, DWI ADC map in E) showed only a punctate focus of coagulative necrosis in the left paratrigonal WM (yellow arrow in E). In all voxels of the intermediate TE 2D-CSI grid (right thalamo-capsular voxel depicted in D) a huge inverted doublet peak centered at 1.14, ppm (mistakable with Lac, without careful inspection) was seen and assigned to PG. The amount of NAA peak reduction was doubtful, possibly influenced by fluctuating baseline due to PG. Antiepileptic therapy was changed (phenobarbital was discontinued as a precaution), the patient significantly improved during the following weeks and, to date, no metabolic disease has been found. Acronyms and abbreviations are shown in Appendix 1.