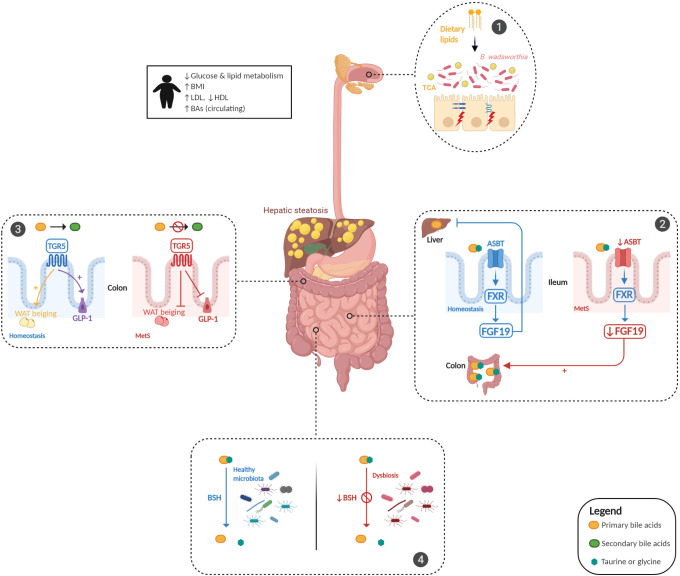
Figure 1.
Bile acid (BA) dysmetabolism in metabolic syndrome. BA metabolism is altered in patients with metabolic syndrome (MetS) and is associated with hepatic steatosis and glucose and lipid dysmetabolism. Dietary animal fat consumption promotes taurocholic acid (TCA) production, which favours the proliferation of sulfite-reducing bacteria, Bilophila wadsworthia, leading to an increase in intestinal permeability and inflammation (panel 1). Gut microbiota alterations induce an impairment in the ileal absorption of BAs, which occurs normally via the apical-sodium BA transporter (ASBT). This induces a decrease in the expression of nuclear Farnesoid-X receptor (FXR) and fibroblast growth factor 19 (FGF19) in intestinal epithelial cells and the abundance of colonic primary conjugated BAs (panel 2). Gut microbiota dysfunction leads to a decreased transformation of primary conjugated BAs to secondary BAs in the colon, leading to defective activation of Takeda-G-protein-receptor-5 (TGR5). The effect of TGR5 activation on the increase in glucagon-like peptide 1 (GLP-1) and white adipose tissue (WAT) browning was thus inhibited (panel 3). Gut microbiota alterations impair bile salt hydrolase (BSH) activity, leading to primary conjugated BA accumulation in the colon (panel 4). BMI, body mass index; HDL, high-density lipoprotein; LDL, low-density lipoprotein.