Abstract
Background: Little is known about financial hardship among Hispanic women with thyroid cancer. The goal of this study was to determine the prevalence of financial hardship and to identify correlates of financial hardship in this understudied patient group.
Methods: We surveyed Hispanic women who had diagnoses of thyroid cancer reported to the Los Angeles Surveillance Epidemiology and End Results (SEER) registry in 2014–2015, and who had previously completed our thyroid cancer survey in 2017–2018 (N = 273; 80% response rate). Acculturation was assessed with the Short Acculturation Scale for Hispanics (SASH). Patients were asked about three outcome measures since their thyroid cancer diagnosis: (i) financial status, (ii) insurance status, and (iii) material measures of financial hardship, collapsed into a single composite measure of financial hardship. We used multivariable logistic regression to identify correlates of financial hardship.
Results: Patients' median age at diagnosis was 47 years (range 20–79 years); 49% were low-acculturated and 47% reported financial hardship. Since their thyroid cancer diagnosis, 31% and 12% of the cohort reported being worse off regarding financial and insurance status, respectively. In multivariable analysis, high-acculturated older women were less likely to experience financial hardship compared with high-acculturated 20-year-old women. While financial hardship decreased with age for high-acculturated women (p = 0.002), financial hardship remained elevated across all age groups for low-acculturated women (p = 0.54).
Conclusions: Our findings suggest that across all age groups, low-acculturated Hispanic women with thyroid cancer are vulnerable to financial hardship, emphasizing the need for tailored patient-focused interventions.
Keywords: thyroid carcinoma, health care disparities, Hispanics, women, acculturation, financial burden
Introduction
Thyroid cancer is the second most commonly diagnosed cancer in Hispanic women in the United States, with an estimated 6800 new thyroid cancer cases among Hispanic women in 2018 (1). The incidence of thyroid cancer in Hispanic patients has increased over time; and although the thyroid cancer mortality rate has been stable, mortality from thyroid cancer is greater for Hispanic women than for non-Hispanic white women (1,2).
A pressing issue for many patients with thyroid cancer is the risk of financial hardship due to the substantial cost of thyroid cancer care in the United States (U.S.). In 2013, the estimated societal cost of thyroid cancer care for all U.S. patients diagnosed after 1985 was $1.6 billion (3). Among cancer survivors, those with thyroid cancer more frequently reported psychological financial hardship and were at higher risk of bankruptcy compared with those with colon, breast, lung, and prostate cancer (4,5). Furthermore, studies of cancer survivors in general have demonstrated that minority race/ethnicity is associated with greater cancer-related financial hardship (6–8). However, granular data on specific factors that contribute to financial hardship in patients of minority race/ethnicity are limited, partly due to the relatively small percentage of nonwhite patients in these prior studies. Thus, little is known about patient-reported financial hardship in a Hispanic cohort and how factors such as acculturation influence financial hardship.
Given the high prevalence of thyroid cancer in Hispanic women and the paucity of research focused on financial hardship in Hispanic women with thyroid cancer, the goal of this study was to determine the prevalence of financial hardship and to identify correlates of financial hardship in this understudied patient group. We hypothesized that low acculturation and younger age would be associated with higher likelihood of financial hardship.
Methods
Data source and study population
Between May 2, 2019 and December 31, 2019, we identified Hispanic women aged 18–79 years who had diagnoses of differentiated thyroid cancer reported to the Los Angeles Surveillance Epidemiology and End Results (SEER) registry between January 1, 2014 and December 31, 2015, and who had previously completed our patient survey on thyroid cancer in 2017–2018 (N = 273; 80% response rate) (9–12). Similar to the methodology used in prior studies on Hispanic women, we surveyed female patients who completed our 2017–2018 thyroid cancer survey in Spanish or were identified in the SEER database as having a Spanish surname or being of Hispanic origin (13). To improve response rates, we provided a $20 cash incentive and used a modified Dillman method, which included multiple reminders to nonresponders (14). Patients were mailed surveys in both English and Spanish, and bilingual interviewers conducted follow-up calls. Survey data were electronically entered using a double entry method to ensure <1% error. Survey responses were merged with clinical cancer data from the Los Angeles SEER registry to create a de-identified data set.
The study was approved by the institutional review boards of the University of Michigan and the University of Southern California, the California Committee for the Protection of Human Subjects, and the California Cancer Registry.
Survey questionnaire design and content
The survey instrument was developed based on the research questions and hypotheses, and prior work in other cancers (9–12,15–23). We utilized standard techniques to assess content validity, including review by clinicians and survey design experts, and pilot testing in a select cohort of Hispanic patients at the University of Michigan.
The English version of the survey was translated into Spanish using well-established translation procedures, with the goal of achieving cultural equivalence between the English and Spanish versions of the instruments (10–13,19). Procedures for achieving cultural equivalence included examining measures for content equivalence, semantic equivalence, technical equivalence, criteria equivalence, and conceptual equivalence.
Measures
Acculturation measure
We assessed acculturation with the Short Acculturation Scale for Hispanics (SASH) developed by Marin et al. (15). Patients were asked to indicate their language preference to the following five items: (i) In general, what language(s) do you read and speak? (ii) What was the language(s) you used as a child? (iii) What language(s) do you usually speak at home? (iv) In which language(s) do you usually think? and (v) What language(s) do you usually speak with your friends? Response categories were based on a five-point Likert scale from “only Spanish” to “only English.” A summary score (range 1–5) was calculated by averaging responses from the individual items. Higher scores indicate a higher level of acculturation.
For our cohort of Hispanic women, the five-item SASH demonstrated excellent internal consistency, with a Cronbach's alpha of 0.965. Given the ordinal nature of the SASH scale, a polychoric correlation matrix was constructed, which showed high inter-item correlations (all >0.71) and item-total correlations (all >0.78). Given the high correlation among the items, summary scores of patients who responded to four items (N = 8) or all five items (N = 263) of the SASH were included in the analysis. Similar to prior publications using the SASH, we used a cutoff of 2.99 to discriminate low-acculturated respondents from high-acculturated respondents (24–26).
Patient-reported financial hardship
To evaluate patients' financial and insurance status since their thyroid cancer diagnosis, we adapted questions about financial burden used in the breast cancer literature (Supplementary Material) (17–19). Patients were asked whether they were worse off regarding their financial status and health insurance since their thyroid cancer diagnosis (yes/no for each). If patients answered “yes,” they were asked how much of this was due to their thyroid cancer and treatment (five-point Likert scale from “not at all” to “very much”).
To identify material measures of financial hardship, we adapted questions derived from the National Consumer Bankruptcy Project and used in the literature on other cancer types (Supplementary Material) (16,20–23). The core survey items were validated by Veenstra et al. in a population-based survey study of colorectal cancer patients, and previously used in five additional studies of breast and colorectal cancer patients, including more than 900 Hispanic cancer patients (18–23). Patients were asked whether, due to the financial impact of having thyroid cancer, they had to use savings; could not make payments on credit cards or other bills; cut down on spending for food; had their utilities turned off; or had to move out of their house or apartment because they could not afford to stay there (yes/no for each). We developed a single binary composite measure of financial hardship, defined as a “yes” response to any of these five individual material measures of financial hardship.
Covariates
We obtained the following patient-reported demographic characteristics: highest level of education, annual household income, health insurance, and comorbidities as detailed in our prior study (11). Clinical cancer characteristics obtained from the SEER registry were age at time of diagnosis (years), and combined clinical and pathological details which the SEER registry used to derive a stage variable following definitions from the American Joint Committee on Cancer 7th edition (AJCC-7) staging system (27).
Statistical analyses
We generated descriptive statistics for all categorical variables. We used Rao–Scott adjusted chi-square tests to evaluate for collinearity between variables and to test for a relationship between the composite measure of financial hardship and the following variables: age at time of diagnosis, highest level of education, annual household income, health insurance, level of acculturation, derived AJCC-7 stage, number of comorbidities, and interaction between age and acculturation.
We used multivariable logistic regression analysis to determine factors associated with the composite measure of financial hardship. As part of the preliminary analyses to help us understand the relationships among our variables of interest, we performed Rao–Scott adjusted chi-square tests on age, income, and insurance. The tests showed a significant relationship among the variables (p < 0.05), consistent with previous established relationships between age and income, age and insurance, and income and insurance (28,29). Since there was collinearity among age, income, and insurance, and since age was most clinically relevant in prior work in thyroid and nonthyroid cancers (4–6,30), we only included the main effects of age, analyzed as a continuous variable, education, derived AJCC-7 stage, acculturation, and the interaction of age and acculturation in the statistical model. By including the interaction of age and acculturation, we allowed the model to have different effects of age for each of the acculturation group. To specify the comparison groups in the model, we centered age at diagnosis to the youngest age in our cohort and established the age of our reference group to be 20 years. We report adjusted odds ratios (OR) with 95% confidence intervals [CI] for all logistic regression models, with p-values <0.05 considered statistically significant.
All statistical analyses incorporated nonresponse weights to reduce potential nonresponse bias. Analyses were performed using SAS 9.4 (SAS, Cary, NC) and Stata 15.1 (StataCorp LLC, College Station, TX).
Results
Characteristics of study cohort
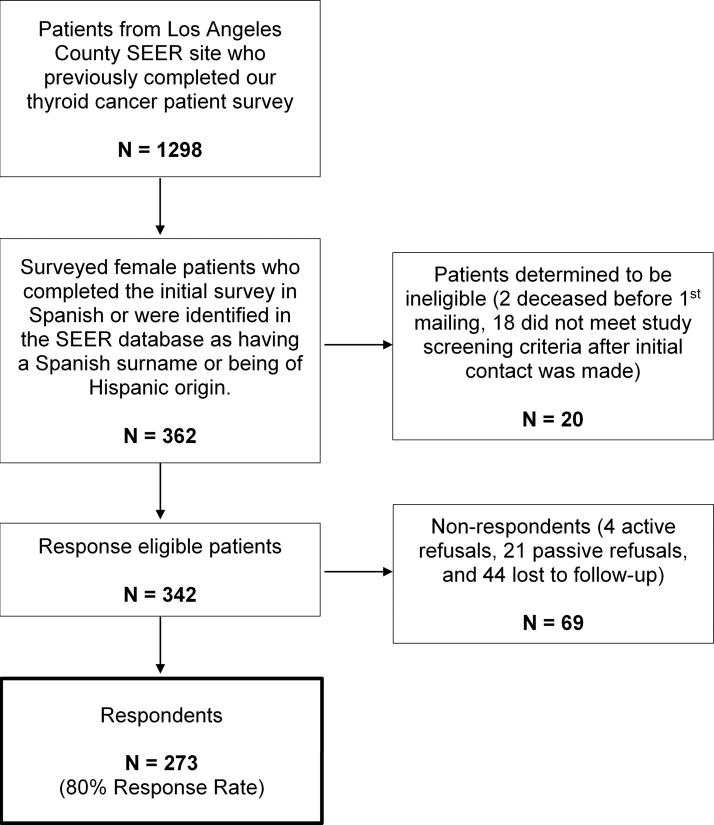
Of the 362 patients identified and mailed a survey, 342 were determined to be eligible. A total of 273 patients responded, yielding an 80% response rate (Fig. 1). Patients' median age at time of diagnosis was 47 years (range 20–79 years), with 74.6% (N = 203) of Mexican origin, 48.7% (N = 135) of low acculturation, and 46.5% (N = 125) with report of financial hardship as determined by the composite measure. There was no significant difference in receipt of total thyroidectomy versus lobectomy, or receipt of radioactive iodine therapy between low- and high-acculturated Hispanic women (p = 0.40 and p = 0.45, respectively).
FIG. 1.
Flow diagram of survey respondents (N = 273, 80% response rate). SEER indicates Surveillance, Epidemiology, and End Results program.
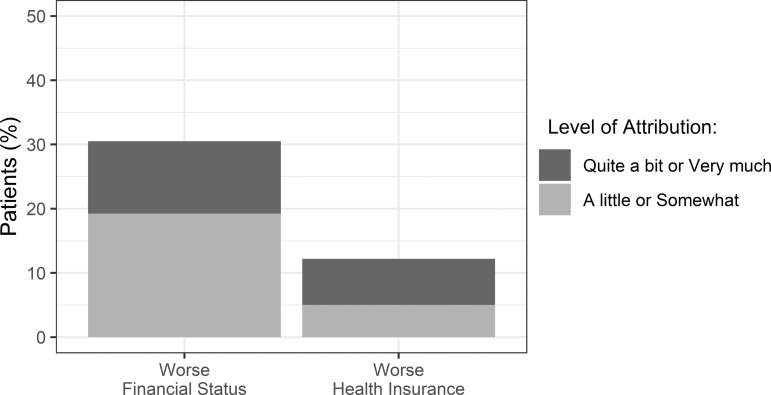
Patient perception of financial hardship
Figure 2 shows the patients who reported worse financial status and health insurance due to their thyroid cancer and treatment. Since their thyroid cancer diagnosis, 30.5% (N = 81) of the cohort endorsed being worse off regarding financial status, with 19.2% (N = 51) attributing a little/somewhat and 11.2% (N = 30) attributing quite a bit/very much of this due to their thyroid cancer and treatment. Regarding health insurance, 12.2% (N = 34) of the cohort endorsed being worse off, with 5.0% (N = 14) attributing a little/somewhat and 7.2% (N = 20) attributing quite a bit/very much of this due to their thyroid cancer and treatment.
FIG. 2.
Patient report of worse financial and health insurance status since their thyroid cancer diagnosis. Distribution of patients who attributed a little/somewhat or quite a bit/very much of this change due to their thyroid cancer and treatment.
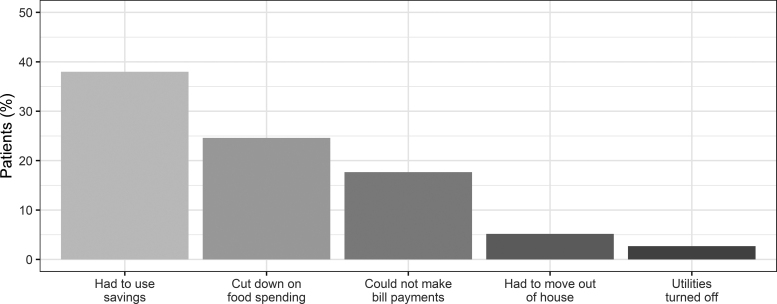
Patient report of material measures of financial hardship
Figure 3 illustrates the distribution of patients who endorsed individual material measures of financial hardship due to thyroid cancer. In the cohort, 38.0% (N = 99) had to use savings, 24.6% (N = 63) cut down on spending for food, 17.7% (N = 44) could not make payments on credit cards or other bills, 5.2% (N = 14) had to move out of their house or apartment because they could not afford to stay there, and 2.7% (N = 7) had their utilities turned off because the bill was not paid.
FIG. 3.
Patient report of material measures of financial hardship due to having thyroid cancer. In the cohort, 38.0% (N = 99) had to use their savings and 2.7% (N = 7) had their utilities turned off because the bill was not paid.
Factors associated with composite measure of financial hardship
Table 1 displays the demographic and clinical characteristics of respondents by composite measure of financial hardship (defined as a “yes” response to any of the five individual material measures of financial hardship). Reported annual household income and health insurance were associated with composite measure of financial hardship (both p < 0.05). To account for the higher percentage of younger individuals with no or minimal savings (31–33), we performed a sensitivity analysis excluding the individual measure of “I had to use savings” from the composite measure of financial hardship (new total of 85 patients, or 31.7% of the cohort with report of financial hardship). This sensitivity analysis demonstrated that reported annual household income and younger age at diagnosis (both p < 0.05), but not health insurance (p = 0.08), correlated with the composite measure of financial hardship.
Table 1.
Distribution of Patient Demographic and Clinical Characteristics by Composite Measure of Financial Hardship (N = 273)
| Characteristica | All patients (N = 273), n (%) | No financial hardship (N = 148), n (%) | Endorsed financial hardshipb(N = 125), n (%) | pc |
|---|---|---|---|---|
| Age at diagnosis (years) | 0.08 | |||
| 20–39 | 88 (34.3) | 41 (46.2) | 47 (53.8) | |
| 40–49 | 68 (24.0) | 34 (50.2) | 34 (49.8) | |
| 50–64 | 82 (30.3) | 48 (57.5) | 34 (42.5) | |
| 65–79 | 35 (11.4) | 25 (71.3) | 10 (28.7) | |
| Highest level of education | 0.55 | |||
| High school diploma and below | 140 (52.1) | 79 (55.4) | 61 (44.6) | |
| Some college | 71 (27.3) | 37 (52.4) | 34 (47.6) | |
| College degree and above | 54 (20.6) | 26 (46.7) | 28 (53.3) | |
| Annual household income | 0.004 | |||
| ≤$49,000 | 121 (43.8) | 52 (41.9) | 69 (58.1) | |
| >$49,000 | 76 (28.4) | 47 (61.8) | 29 (38.2) | |
| Missing value | 76 (27.8) | 49 (63.2) | 27 (36.8) | |
| Health insurance | 0.04 | |||
| Private insurance | 129 (50.1) | 64 (49.5) | 65 (50.5) | |
| Medicare | 55 (19.5) | 38 (68.9) | 17 (31.1) | |
| Otherd | 79 (30.4) | 39 (48.2) | 40 (51.8) | |
| Level of acculturation | 0.33 | |||
| Low acculturation | 135 (48.7) | 70 (50.4) | 65 (49.6) | |
| High acculturation | 136 (51.3) | 77 (56.5) | 59 (43.5) | |
| Derived AJCC-7 stage | 0.69 | |||
| Stage I/II | 192 (72.7) | 105 (53.8) | 87 (46.2) | |
| Stage III/IV | 75 (27.3) | 39 (51.1) | 36 (48.9) | |
| No. of comorbidities | 0.98 | |||
| 0 | 174 (64.6) | 95 (53.3) | 79 (46.7) | |
| 1 | 68 (24.6) | 36 (53.3) | 32 (46.7) | |
| ≥2 | 31 (10.8) | 17 (55.1) | 14 (44.9) |
Percentages are calculated based on the responders.
The composite measure of financial hardship is defined as a “yes” response to any of the five individual material measures of financial hardship: I had to use savings; I could not make payments on credit cards or other bills; I cut down on spending for food; I had my utilities turned off because the bill was not paid; or I had to move out of my house or apartment because I could not afford to stay there.
p-Values are derived from Rao–Scott adjusted chi-square tests.
Other health insurance includes insurance purchased from an exchange; Medicaid or other state provided insurance; Veteran Affairs health care; or self-pay.
AJCC-7, American Joint Committee on Cancer 7th edition.
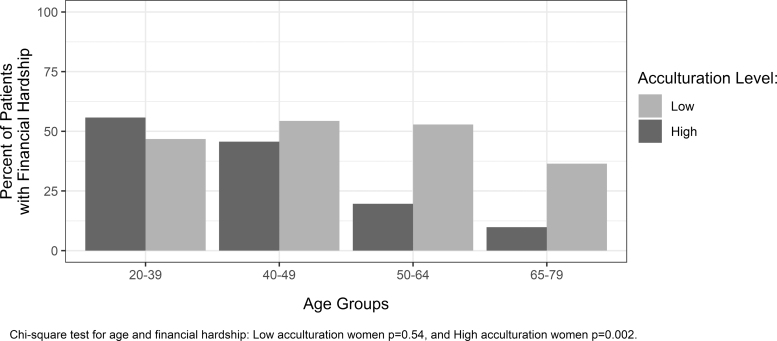
Figure 4 demonstrates the impact of age and acculturation on composite measure of financial hardship. For Hispanic women with high acculturation, financial hardship decreased with older age (p = 0.002). However, for Hispanic women with low acculturation, financial hardship remained elevated across all age groups (p = 0.54).
FIG. 4.
The influence of age and level of acculturation on financial hardship in Hispanic women. While financial hardship decreased with age for high-acculturated women (p = 0.002), financial hardship remained elevated across all age groups for low-acculturated women (p = 0.54).
Table 2 shows factors associated with the composite measure of financial hardship. After adjustment for education, stage, and level of acculturation, high-acculturated older women had lower odds of financial hardship (OR 0.93 [CI 0.90–0.97]) compared with high-acculturated 20-year-old women. Low-acculturated older women, however, had similar odds of financial hardship (OR 0.98 [CI 0.95–1.01]) compared with high-acculturated 20-year-old women. Sensitivity analysis excluding the individual measure “I had to use savings” from the composite measure of financial hardship yielded similar results: high-acculturated, but not low-acculturated, older women had lower odds of financial hardship (high-acculturated older women: OR 0.94 [CI 0.91–0.97]; low-acculturated older women: OR 0.98 [CI 0.95–1.01]) compared with high-acculturated 20-year-old women. Similarly, when we excluded cancer stage, which exhibited collinearity with age (p < 0.05), as a covariate in the model, high-acculturated, but not low-acculturated, older women had lower odds of financial hardship (high-acculturated older women: OR 0.94 [CI 0.91–0.97]; low-acculturated older women: OR 0.99 [CI 0.96–1.02]) compared with high-acculturated 20-year-old women. Education and stage were not associated with the composite measure of financial hardship in the multivariable model.
Table 2.
Multivariable Adjusted Odds Ratios and 95% Confidence Intervals of Patient Characteristics Associated with Composite Measure of Financial Hardship Among Hispanic Women with Thyroid Cancer
| OR [CI] | |
|---|---|
| Highest level of education | |
| High school diploma and below | 0.73 [0.33–1.61] |
| Some college | 0.81 [0.38–1.71] |
| College degree and above | Reference |
| Derived AJCC-7 stage | |
| Stage I/II | Reference |
| Stage III/IV | 1.80 [0.94–3.44] |
| Level of acculturation | |
| Low acculturation | 0.60 [0.17–2.13] |
| High acculturation | Reference |
| Effect of age by acculturationa | |
| Age for low-acculturated women | 0.98 [0.95–1.01] |
| Age for high-acculturated women | 0.93 [0.90–0.97] |
Reference categories: college degree and above (highest level of education), stage I/II (derived AJCC-7 stage), high acculturation (level of acculturation), high-acculturated 20-year-old (effect of age by acculturation).
Age is analyzed as a continuous variable in the statistical model. Therefore, the OR for “effect of age by acculturation” represents the OR for an increase of one year in age.
CI, 95% confidence interval; OR, odds ratio.
Discussion
Our study, which to our knowledge is the first population-based survey study to examine financial hardship in a cohort of Hispanic women with thyroid cancer, provides novel insights into the relationship between acculturation, age, and financial hardship in this understudied patient group. Our findings in women with high acculturation mirror prior studies, with younger age associated with greater financial hardship (4–6,30). However, unique from prior studies and for the first time, we found that in women with low acculturation, financial hardship remained elevated across all age groups. That is, older women with low acculturation had similar susceptibility to financial hardship as did younger women.
Consistent with studies of patients with other malignancies, we found that income was associated with financial hardship. In a prospective study of patients with head and neck cancers, Beeler et al. showed that lower median household income (less than $50,000 per year) by county was associated with worse financial burden (30). Additionally, Han et al. found that among cancer survivors, lower family income was associated with greater financial hardship (8). Similarly, Huang et al. demonstrated that among adult survivors of childhood cancer, annual household income of $39,999 or less, compared with $80,000 or more, increased risk of financial hardship (34). In contrast to these prior nonthyroid cancer studies in which the majority of the cohort were non-Hispanic white patients, our study examined financial hardship in a cohort of Hispanic women with thyroid cancer.
The observed differences in Hispanic women's susceptibility to financial hardship based on their level of acculturation are unlikely to be due to differences in thyroid cancer treatment but may be a result of disparities in income, employer-sponsored retirement plans, and social security benefits. In 2013, median earnings for foreign-born Hispanic women aged 25–64 years who were employed full-time were $23,400 compared with $35,600 for U.S.-born Hispanic women and $41,700 for non-Hispanic white women (35). The lower earning potential of foreign-born Hispanic women may partly be due to employment barriers for women with limited English proficiency (35,36). In 2014, among employed foreign-born Hispanic women aged 25–64 years, 26% worked in food prep, building and grounds cleaning, and personal care; 15% in office and administrative support; and 9% in management, business operations, and finance. This was compared with the 9%, 27%, and 17% of employed U.S.-born Hispanic women who worked in these occupations, respectively (35). Furthermore, full-time Hispanic women employees aged 25–64 years were less likely to participate in an employer-sponsored retirement plan (30% of foreign-born Hispanic women and 46% of U.S.-born Hispanic women) compared with their non-Hispanic white counterparts (57%) (35). The financial impact of these shortcomings in earnings and workplace retirement plans is compounded when individuals apply for social security benefits, which require at least 10 years of employment to qualify. In 2013, only 75% of Hispanic adults aged 65 years and older received social security benefits compared with almost 90% of non-Hispanic white adults. Unfortunately, even among recipients aged 65 years and older, there is income inequality such that the median 2013 social security income for foreign-born Hispanic recipients was $9100 compared with $11,600 for U.S.-born Hispanic recipients and $14,200 for non-Hispanic white recipients (35).
Hispanic women with thyroid cancer are an underrepresented and understudied patient population, thus studies such as this one are needed to improve the depth of thyroid cancer disparities research (37). While our study has several strengths, including a high response rate among surveyed patients, focus on an understudied patient population, and use of the validated SASH to assess acculturation, it also has limitations. First, there may be other aspects of cancer-related financial hardship that were not assessed. However, the individual measures of financial hardship used in our survey were adapted from the Consumer Bankruptcy Project, which provides free legal assistance to low-income consumers with outstanding debts (16), and are measures that have previously been used to study financial hardship in more than 4000 patients with colorectal and breast cancer, including more than 900 Hispanic patients (18–23). Second, our cohort was restricted to Hispanic women with thyroid cancer from the Los Angeles County (predominantly Mexican and Central American origin), and thus, findings may not be generalizable to Latinas with origins from the Caribbean or South America. Third, patients were not asked about out-of-pocket cancer-related expenses or about social security benefits, information that could provide insight into financial hardship among low-acculturated Hispanic women.
Our study highlights the unique vulnerability of low-acculturated Hispanic women and their need for patient-focused interventions to address cancer-related financial hardships. Such financial hardships have negative consequences on patients' mental and physical health with patients at increased risk for anxiety and depression, and some patients choosing to forgo prescription medications or delay medical care as a result (6,38,39). Identification of patients at risk for cancer-related financial hardship followed by meetings with financial counselors may be beneficial in helping patients to mitigate out-of-pocket expenses and access information about financial assistance programs. Psychosocial interventions may also be necessary to address any psychological distress that patients may develop as a result of their financial difficulties. Furthermore, these interventions will need to be tailored to the unique needs of low-acculturated Hispanic women. Specifically, it will be important to involve bilingual staff, have resources available in both English and Spanish, utilize social media platforms (40), be accessible outside traditional office hours for patients with limited flexibility for time off work, and/or offer virtual visits through video/telephone communication for patients who would otherwise need to travel long distances.
Acknowledgment
Brittany Gay assisted with the tables and figures.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This study is supported by the National Cancer Institute (NCI) Grant No. R01 CA201198 with R01 supplement from the Office of Research on Women's Health (ORWH) to Principal Investigator, Dr. Megan R. Haymart. Dr. Haymart also receives funding from R01 HS024512 from the Agency for Healthcare Research and Quality. Dr. Debbie W. Chen receives support from grant T32DK007245 from the National Institutes of Diabetes and Digestive and Kidney Diseases. The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; the Centers for Disease Control and Prevention's (CDC) National Program of Cancer Registries, under Cooperative Agreement No. 5NU58DP003862-04/DP003862; and the NCI's SEER Program under Contract No. HHSN261201000035C awarded to the University of Southern California. The ideas and opinions expressed herein are those of the authors, and endorsement by the State of California Department of Public Health, the NCI, and the CDC or their contractors and subcontractors is not intended nor should be inferred.
Supplementary Material
Supplementary Material
References
- 1. Miller KD, Goding Sauer A, Ortiz AP, Fedewa SA, Pinheiro PS, Tortolero-Luna G, Martinez-Tyson D, Jemal A, Siegel RL. 2018. Cancer statistics for Hispanics/Latinos, 2018. CA Cancer J Clin 68:425–445 [DOI] [PubMed] [Google Scholar]
- 2. Kotwal A, Bleyer A, Brito JP. 2019. Thyroid cancer incidence continues to rise but mortality remains stable in Young, Hispanic, and Black Populations in the United States. Endocr Pract 25:115–116 [DOI] [PubMed] [Google Scholar]
- 3. Lubitz CC, Kong CY, McMahon PM, Daniels GH, Chen Y, Economopoulos KP, Gazelle GS, Weinstein MC. 2014. Annual financial impact of well-differentiated thyroid cancer care in the United States. Cancer 120:1345–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ramsey S, Blough D, Kirchhoff A, Kreizenbeck K, Fedorenko C, Snell K, Newcomb P, Hollingworth W, Overstreet K. 2013. Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 32:1143–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Barrows CE, Belle JM, Fleishman A, Lubitz CC, James BC. 2020. Financial burden of thyroid cancer in the United States: an estimate of economic and psychological hardship among thyroid cancer survivors. Surgery 167:378–384 [DOI] [PubMed] [Google Scholar]
- 6. Kent EE, Forsythe LP, Yabroff KR, Weaver KE, de Moor JS, Rodriguez JL, Rowland JH. 2013. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care? Cancer 119:3710–3717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. de Souza JA, Yap BJ, Wroblewski K, Blinder V, Araujo FS, Hlubocky FJ, Nicholas LH, O'Connor JM, Brockstein B, Ratain MJ, Daugherty CK, Cella D. 2017. Measuring financial toxicity as a clinically relevant patient-reported outcome: the validation of the COmprehensive Score for financial Toxicity (COST). Cancer 123:476–484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Han X, Zhao J, Zheng Z, de Moor JS, Virgo KS, Yabroff KR. 2020. Medical financial hardship intensity and financial sacrifice associated with cancer in the United States. Cancer Epidemiol Biomarkers Prev 29:308–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Esfandiari NH, Hughes DT, Reyes-Gastelum D, Ward KC, Hamilton AS, Haymart MR. 2019. Factors associated with diagnosis and treatment of thyroid microcarcinomas. J Clin Endocrinol Metab 104:6060–6068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen DW, Reyes-Gastelum D, Wallner LP, Papaleontiou M, Hamilton AS, Ward KC, Hawley ST, Zikmund-Fisher BJ, Haymart MR. 2020. Disparities in risk perception of thyroid cancer recurrence and death. Cancer 126:1512–1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Papaleontiou M, Reyes-Gastelum D, Gay BL, Ward KC, Hamilton AS, Hawley ST, Haymart MR. 2019. Worry in thyroid cancer survivors with a favorable prognosis. Thyroid 29:1080–1088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Papaleontiou M, Evron JM, Esfandiari NH, Reyes-Gastelum D, Ward KC, Hamilton AS, Worden F, Haymart MR. 2020. Patient report of recurrent and persistent thyroid cancer. Thyroid 30:1297–1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Katz SJ, Wallner LP, Abrahamse PH, Janz NK, Martinez KA, Shumway DA, Hamilton AS, Ward KC, Resnicow KA, Hawley ST. 2017. Treatment experiences of Latinas after diagnosis of breast cancer. Cancer 123:3022–3030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dillman DA, Smyth JD, Christian LM. 2009. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method. John Wiley, Hoboken, NY [Google Scholar]
- 15. Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. 1987. Development of a short acculturation scale for hispanics. Hispanic J Behav Sci 9:183–205 [Google Scholar]
- 16. Pottow JAE, Lawless RM, Littwin AK, Porter KM, Thorne DK. 2008. Did bankruptcy reform fail? An empirical study of consumer debtors. Am Bankr L J 82:349–405 [Google Scholar]
- 17. Veenstra CM, Wallner LP, Jagsi R, Abrahamse P, Griggs JJ, Bradley CJ, Hawley ST. 2017. Long-term economic and employment outcomes among partners of women with early-stage breast cancer. J Oncol Pract 13:e916–e926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jagsi R, Ward KC, Abrahamse PH, Wallner LP, Kurian AW, Hamilton AS, Katz SJ, Hawley ST. 2018. Unmet need for clinician engagement regarding financial toxicity after diagnosis of breast cancer. Cancer 124:3668–3676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jagsi R, Pottow JA, Griffith KA, Bradley C, Hamilton AS, Graff J, Katz SJ, Hawley ST. 2014. Long-term financial burden of breast cancer: experiences of a diverse cohort of survivors identified through population-based registries. J Clin Oncol 32:1269–1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Graff J, Katz SJ. 2011. Racial/ethnic differences in job loss for women with breast cancer. J Cancer Surviv 5:102–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Regenbogen SE, Veenstra CM, Hawley ST, Banerjee M, Ward KC, Kato I, Morris AM. 2014. The personal financial burden of complications after colorectal cancer surgery. Cancer 120:3074–3081 [DOI] [PubMed] [Google Scholar]
- 22. Veenstra CM, Regenbogen SE, Hawley ST, Griggs JJ, Banerjee M, Kato I, Ward KC, Morris AM. 2014. A composite measure of personal financial burden among patients with stage III colorectal cancer. Med Care 52:957–962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Veenstra CM, Regenbogen SE, Hawley ST, Abrahamse P, Banerjee M, Morris AM. 2015. Association of paid sick leave with job retention and financial burden among working patients with colorectal cancer. JAMA 314:2688–2690 [DOI] [PubMed] [Google Scholar]
- 24. Sepucha K, Feibelmann S, Chang Y, Hewitt S, Ziogas A. 2015. Measuring the quality of surgical decisions for Latina breast cancer patients. Health Expect 18:2389–2400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dancel LD, Perrin E, Yin SH, Sanders L, Delamater A, Perreira KM, Bronaugh AB, Eden S, Shintani A, Rothman RL. 2015. The relationship between acculturation and infant feeding styles in a Latino population. Obesity (Silver Spring) 23:840–846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Silveira ML, Dye BA, Iafolla TJ, Adesanya MR, Boroumand S, Youngblood ME, Salazar CR, Finlayson TL, Khambaty T, Beaver SM, Garcia AI. 2020. Cultural factors and oral health-related quality of life among dentate adults: hispanic community health study/study of Latinos. Ethn Health 25:420–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Adamo M DL, Ruhl J. 2014. 2014 SEER Program Coding and Staging Manual. National Cancer Institute, Bethesda, MD [Google Scholar]
- 28. Barnett JC, Berchick ER. 2017. Health Insurance Coverage in the United States: 2016. U.S. Government Printing Office, Washington, DC [Google Scholar]
- 29. York E. Average income tends to rise with age. Available at https://taxfoundation.org/average-income-age (accessed April1, 2020)
- 30. Beeler WH, Bellile EL, Casper KA, Jaworski E, Burger NJ, Malloy KM, Spector ME, Shuman AG, Rosko A, Stucken CL, Chinn SB, Dragovic AF, Chapman CH, Owen D, Jolly S, Bradford CR, Prince MEP, Worden FP, Jagsi R, Mierzwa ML, Swiecicki PL. 2020. Patient-reported financial toxicity and adverse medical consequences in head and neck cancer. Oral Oncol 101:104521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Board of Governors of the Federal Reserve System 2019 Report of the Economic Well-Being of U.S. Households in 2018. Federal Reserve Board, Washington, DC [Google Scholar]
- 32. Bank of America. 2018 Better money habits millenial report. Available at https://bettermoneyhabits.bankofamerica.com/content/dam/bmh/pdf/ar6vnln9-boa-bmh-millennial-report-winter-2018-final2.pdf (accessed April1, 2020)
- 33. Huddleston C. Survey: 69% of Americans have less than $1,000 in savings. Available at https://www.gobankingrates.com/saving-money/savings-advice/americans-have-less-than-1000-in-savings (accessed April1, 2020)
- 34. Huang IC, Bhakta N, Brinkman TM, Klosky JL, Krull KR, Srivastava D, Hudson MM, Robison LL. 2019. Determinants and consequences of financial hardship among adult survivors of childhood cancer: a Report From the St. Jude Lifetime Cohort Study. J Natl Cancer Inst 111:189–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Johnson RW, Mudrazija S, Wang CX. Hispanics' retirement security: past trends and future prospects. Available at https://www.urban.org/research/publication/hispanics-retirement-security/view/full_report (accessed April1, 2020)
- 36. Bleakley H, Chin A. 2004. Language skills and earnings: evidence from childhood immigrants. Rev Econ Stat 86:481–496 [Google Scholar]
- 37. Chen DW, Haymart MR. 2020. Disparities research in thyroid cancer: challenges and strategies for improvement. Thyroid 30:1231–1235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sharp L, Carsin AE, Timmons A. 2013. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology 22:745–755 [DOI] [PubMed] [Google Scholar]
- 39. Mongelli MN, Giri S, Peipert BJ, Helenowski IB, Yount SE, Sturgeon C. 2020. Financial burden and quality of life among thyroid cancer survivors. Surgery 167:631–637 [DOI] [PubMed] [Google Scholar]
- 40. Center for Disease Control and Prevention. Cultural insights: communicating with Hispanics/Latinos. Available at https://www.cdc.gov/healthcommunication/pdf/audience/audienceinsight_culturalinsights.pdf (accessed April1, 2020)