Abstract
Childhood cancer survivors treated with hematopoietic stem cell transplantation are at high risk for pulmonary morbidity and mortality. In this retrospective study we described transplant characteristics of pediatric patients who underwent hematopoietic stem cell transplantation in Switzerland and how these characteristics changed over time, compared self-reported pulmonary outcomes between transplanted and non-transplanted survivors, and investigated risk factors for the reported pulmonary outcomes. As part of the population-based Swiss Childhood Cancer Survivor Study, we sent questionnaires to all ≥5-year childhood cancer survivors diagnosed 1976–2010 at age ≤20 years. We included 132 transplanted survivors and 368 matched non-transplanted survivors. During the study period transplant characteristics changed, with decreasing use of total body irradiation and increased use of peripheral blood stem cells and mismatched and unrelated donors as transplant source. One-fifth of transplanted survivors (20%, 95%CI 13–27%) and 18% of non-transplanted survivors (95%CI 13–21%) reported at least one pulmonary outcome. None of the analyzed factors was significantly associated with an increased risk of pulmonary outcomes in multivariable analysis. We found that pulmonary outcomes were frequently reported in transplanted and non-transplanted childhood cancer survivors, indicating a strong need for long-term pulmonary follow-up care.
Subject terms: Paediatrics, Epidemiology, Risk factors
Introduction
Hematopoietic stem cell transplantation (HSCT) is an effective but intensive treatment for childhood cancer. HSCT can be performed as allogeneic or autologous transplantation and is used either as first line or salvage treatment [1–4]. The history of allogeneic HSCT goes back to the 1980 s and indications, conditioning regimens, and donor sources have changed enormously since then [5, 6]. Pulmonary damage and late effects due to lung toxic treatments and complications prior to, during, or after transplantation can occur in childhood cancer survivors (CCS) [7–9]. Lung toxic treatments include the chemotherapeutics bleomycin, busulfan, carmustine (BCNU) or lomustine (CCNU), radiation involving the lung tissue, total body irradiation (TBI), and thoracic surgery [10–13]. Transplant-specific pulmonary complications include idiopathic pulmonary syndrome and complications from the spectrum of pulmonary graft versus host disease (GvHD), such as bronchiolitis obliterans or bronchiolitis obliterans organizing pneumonia [7, 14–16]. Severe pulmonary infections are additional complications due to long-lasting neutropenic episodes.
Pulmonary symptoms and diseases, summarized as pulmonary outcomes, are associated with high morbidity in survivors [17–19]. Cohort studies showed that survivors more often report pulmonary outcomes than siblings [20, 21]. To date, pulmonary outcomes in survivors after HSCT have only been reported by few single-center studies [22, 23]. Data based on national population-based assessments of pulmonary outcomes are lacking.
This nationwide retrospective study describes transplant characteristics, such as transplant indications and conditioning regimens, of pediatric patients who had HSCT in Switzerland and how these characteristics changed over time. Then, we compared self-reported pulmonary outcomes between transplanted and non-transplanted survivors and investigated risk factors for reporting pulmonary outcomes.
Methods
The Swiss Childhood Cancer Survivor Study
The Swiss Childhood Cancer Survivor Study (SCCSS) is a long-term national cohort study of all patients registered in the Swiss Childhood Cancer Registry (SCCR) who have been diagnosed since 1976, have survived ≥5 years after initial diagnosis, and were alive at the time of study inclusion [24]. The SCCR is a nationwide, population-based cancer registry including all patients diagnosed below age <21 years with leukemia, lymphoma, central nervous system (CNS) tumors, malignant solid tumors, or Langerhans cell histiocytosis [25]. From 2007 to 2017, we sent questionnaires to parents of children aged 5–15 years, adolescents aged 16–19 years, and adult CCS aged ≥20 years. The Ethics Committee of the Canton of Bern approved the SCCR and SCCSS (KEK-BE: 166/2014). The SCCSS is registered at ClinicalTrials.gov (identifier: NCT03297034).
Study population
We included all survivors who participated in the SCCSS and had been treated in a clinic affiliated to the Swiss Pediatric Oncology Group (SPOG) between 1976 and 2010. As the definition of 5-year survivors was based on the year of diagnosis and not the year of HSCT, some participants might have been transplanted <5 years before answering the questionnaire. As comparison group, we included survivors participating in the SCCSS who had not had a HSCT. Non-transplanted CCS were matched to transplanted CCS based on sex, diagnosis, age at diagnosis (range ± 2 years), and year of diagnosis (range ± 5 years) striving for a 1:3 ratio. Through this matching we wanted to achieve that CCS in both groups were as similar as possible in terms of sex, age at diagnosis and diagnosis, but did only differ by whether they had had HSCT or not. This matching did probably not eliminate all other differences between the groups since the reason for HSCT, such as high-risk status or relapse, already demands additional treatment for the HSCT patients.
Treatment and transplant characteristics
We collected treatment- and transplant-related characteristics of transplanted survivors from medical records. We calculated cumulative doses for eight known or suspected lung toxic agents: bleomycin, busulfan, carmustin (BCNU), cyclophosphamide, ifosfamide, lomustin (CCNU), melphalan, and thiotepa [11–13, 26]. We combined cumulative doses of alkylating agents (all chemotherapeutics except of bleomycin) by calculating the cyclophosphamide equivalent dose (CED) [27]. We categorized the cumulative CED as either lower/equal to or higher than 11,300 mg/m2 with a median-split. We converted busulfan given orally to busulfan intravenously by multiplying it by factor 0.8 [28]. We categorized chest radiation as yes/no according to the Children’s Oncology Group guidelines version 5.0 [13] and included irradiation of the upper abdomen. We recorded surgery to the thorax, lung, chest wall, mediastinum, and thoracic spine. Needle biopsies and implantation of venous devices were not coded as thoracic surgery. We collected date of transplantation, history of relapse, remission status, source of transplant, stem cell donor, cytomegalovirus (CMV) status, sex and blood group of donor and recipient, and information on graft versus host disease (GvHD). We categorized stem cell transplantation into autologous and allogeneic and further specified allogeneic transplantation into Human Leucocyte Antigen (HLA) matched (e.g., 12/12) and HLA-mismatched (e.g., 9/10) donors. As HLA typing and documentation changed substantially in the last decades, it was not possible to assess exact HLA matching [29, 30]. We categorized GvHD into acute and chronic according to information from medical records.
Pulmonary outcomes
We collected information on pulmonary symptoms (chronic cough defined as ≥3 months) and diseases (pneumonia in last 2 years, lung fibrosis, emphysema, or chest wall abnormality) from the SCCSS questionnaires. We categorized the different pulmonary outcomes as yes/no (present/absent) variables. In addition to answering the questions, participants could describe other problems as free text. Responses we could not assign to one of the existing categories were coded as “other pulmonary problem”. We had ≤5% missings on pulmonary outcomes except for pneumonia (6% missings). We allocated missing information to “not having the pulmonary outcome” assuming that survivors would mention pulmonary outcomes if they were clinically significant.
Clinical and lifestyle characteristics
We extracted the following clinical characteristics from the SCCR: sex, age at diagnosis, year of diagnosis, and cancer diagnoses according to the International Classification of Childhood Cancer, 3rd edition [31]. For analyses, we used the following four diagnostic categories: leukemia, where patients with relapsed and refractory disease often receive allogeneic HSCT, lymphoma, and neuroblastoma, where autologous HSCT is used for relapsed or high-risk disease, and other diagnoses, where HSCT is used less frequently. For lifestyle characteristics we extracted smoking status from the questionnaires (Supplementary Explanation E1).
Statistical analysis
We used descriptive statistics to describe sociodemographic, lifestyle, and clinical characteristics of transplanted and non-transplanted CCS. To assess trends in transplant characteristics across transplant eras we used the “nptrend” command in STATA software [32]. We compared the prevalence of pulmonary outcomes between transplanted and non-transplanted CCS using chi-square tests. We used logistic regression and likelihood ratio tests to quantify associations between sociodemographic, lifestyle, clinical, and transplant-related variables and pulmonary outcomes in transplanted CCS. We retained variables with a p value ≤ 0.1 in the univariable analysis for inclusion into the multivariable model and included radiotherapy as a priori confounder according to the literature. We compared sociodemographic and clinical characteristics of transplanted CCS who did or did not respond to the questionnaire by using chi-square tests and student’s t-tests. We used STATA software (Version 16.0, Stata Corporation, Austin, TX) to analyze the data.
Results
Characteristics of study population
We included 132 transplanted and 368 matched non-transplanted CCS (Supplementary Figs. F1 and F2). Transplanted responders and non-responders did not differ in sociodemographic, lifestyle, and clinical characteristics (Supplementary Table S1). The median age of transplanted CCS was 6.5 years (interquartile range, IQR 2.9–11.6 years) at cancer diagnosis and 8.8 years (IQR 4.8–13.6) at transplantation. Median follow-up time was 9.8 years (IQR 7.2–15.9). Leukemia was the most frequent cancer diagnosis (55%), followed by lymphoma (15%), and neuroblastoma (14%) (Table 1).
Table 1.
Characteristics of transplanted (N = 132) and non-transplanted (N = 368) childhood cancer survivors, matched by sex, age at diagnosis, diagnosis, and year of diagnosis (1:3 ratio).
| Transplanted CCS (n = 132) | Non-transplanted CCS (n = 368) | |
|---|---|---|
| n (%) | n (%) | |
| Sociodemographic and lifestyle characteristics | ||
| Sex, male | 69 (52) | 195 (53) |
| Age at questionnaire, median years (IQR) | 18.4 (13.8–22.9) | 18.5 (13.6–23.8) |
| Smoking statusa | ||
| Active smoking | 7 (5) | 27 (7) |
| Passive smoking | 63 (48) | 163 (44) |
| Former active smoking | 9 (6) | 20 (6) |
| Never smoking | 54 (41) | 158 (43) |
| Clinical characteristics | ||
| Age at diagnosis, median years (IQR) | 6.5 (2.9–11.6) | 6.4 (2.7–11.4) |
| Age at transplantation, median years (IQR) | 8.8 (4.8–13.6) | NA |
| Follow-up timeb, median years (IQR) | 9.8 (7.2–15.9) | 10.1 (7.9–15.1) |
| Era of diagnosis | ||
| 1976–1995 | 40 (30) | 120 (33) |
| 1996–2005 | 60 (45) | 156 (42) |
| 2006–2010 | 32 (25) | 92 (25) |
| Childhood cancer diagnosis according to ICCC-3 | ||
| I: Leukemia | 72 (55) | 214 (58) |
| II: Lymphoma | 20 (15) | 60 (16) |
| IV: Neuroblastoma | 19 (14) | 44 (12) |
| Otherc | 21 (16) | 50 (14) |
CCS childhood cancer survivors, ICCC-3 International Classification of Childhood Cancer, 3rd edition, IQR interquartile range.
a“Active” and “former active smoking” assessed in adolescents and adults; “passive smoking” in children corresponds to having parents who currently smoke or formerly smoked, “never smoking” in children corresponds to having both parents who never smoked.
bTime from first diagnosis until date of answering the questionnaire.
cOther tumors in transplanted survivors include: tumors of the central nervous system (n = 6), retinoblastoma (n = 1), malignant bone tumors (n = 7), soft tissue sarcomas (n = 4), malignant germ cell tumors (n = 3) Other tumors in non-transplanted survivors include: tumors of the central nervous system (n = 12), retinoblastoma (n = 1), malignant bone tumors (n = 9), soft tissue sarcomas (n = 4), malignant germ cell tumors (n = 3).
Transplant characteristics and change over time
The absolute number of transplanted CCS who participated in the SCCSS increased over time. Leukemia remained the most common underlying cancer diagnosis in all three eras (Table 2). Conditioning regimens changed with a relative but non-significant reduction in TBI-containing regimens from 61% in the first to 39% in the other two eras (p for trend = 0.083). Among chemotherapeutics, the proportion of CCS who received ifosfamide increased (p = 0.002) but the median cumulative dose decreased non-significantly (p = 0.477). Also cyclophosphamide dosage decreased (p < 0.001) with no significant reduction in the proportion of CCS receiving it (p = 0.186). For bleomycin there was a trend towards lower cumulative doses in more recent eras (p = 0.094). Two-thirds (65%) of CCS had radiotherapy involving the thorax with no significant change over time, and 9% had thoracic surgery with a trend to an increasing proportion of CCS in more recent years. Nearly half of transplanted CCS received autologous HSCT (46%) and in 57% HSCT was performed in first remission or refractory disease. The proportion of transplanted CCS receiving peripheral blood stem cells increased from 27% to 71% with a corresponding reduction in the proportion of those receiving bone marrow stem cells (p for trend <0.001). Eight CCS developed chronic GvHD (cGvHD) but none had pulmonary GvHD (Supplementary Table S2). Supplementary Tables S2 and S3 provide summaries of clinical, treatment, and transplant characteristics for CCS transplanted in autologous or allogeneic settings, stratified by era of transplantation. Differences in CCS exposed to allogeneic or autologous HSCT are shown in Supplementary Table S4.
Table 2.
Characteristics of transplanted childhood cancer survivors (N = 132) stratified by era of transplantation.
| Total (n = 132) | 1976–1995 (n = 33) | 1996–2005 (n = 51) | 2006–2015 (n = 48) | p value* | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Clinical characteristics | |||||
| Cancer diagnosis according to ICCC-3 | 0.806 | ||||
| I: Leukemia | 72 (55) | 18 (55) | 26 (51) | 28 (58) | |
| II: Lymphoma | 20 (15) | 8 (24) | 7 (14) | 5 (10) | |
| IV: Neuroblastoma | 19 (14) | 5 (15) | 8 (16) | 6 (13) | |
| Othera | 21 (16) | 2 (6) | 10 (19) | 9 (19) | |
| Treatment characteristics | |||||
| Conditioning containing TBI | 59 (45) | 20 (61) | 20 (39) | 19 (39) | 0.083 |
| Conditioning regimens | 0.003 | ||||
| TBI + cyclophosphamide ± others | 34 (26) | 16 (48) | 12 (23) | 6 (13) | |
| TBI + others | 25 (19) | 4 (12) | 8 (16) | 13 (27) | |
| Busulfan + cyclophosphamide ± other | 28 (21) | 7 (21) | 11 (21) | 10 (21) | |
| Busulfan ± others | 8 (6) | 1 (3) | 4 (8) | 3 (6) | |
| Carmustine ± others | 9 (7) | 3 (9) | 3 (6) | 3 (6) | |
| Cyclophosphamide ± others | 9 (7) | 1 (3) | 6 (12) | 2 (4) | |
| Melphalan ± carboplatin ± others | 19 (14) | 1 (3) | 7 (14) | 11 (23) | |
| Chemotherapeutic agents | |||||
| Alkylating agents combinedb | 131 (99) | 33 (100) | 50 (98) | 48 (100) | |
| Busulfan | 37 (28) | 9 (27) | 16 (31) | 12 (25) | 0.776 |
| Carmustine | 9 (7) | 4 (12) | 3 (6) | 2 (4) | 0.180 |
| Cyclophosphamide | 123 (93) | 33 (100) | 46 (90) | 44 (92) | 0.186 |
| Ifosfamide | 62 (47) | 9 (27) | 23 (45) | 30 (63) | 0.002 |
| Lomustine | 2 (2) | 1 (3) | - | 1 (2) | 0.835 |
| Melphalan | 44 (33) | 9 (27) | 17 (33) | 18 (38) | 0.342 |
| Thiotepa | 14 (11) | 3 (9) | 8 (16) | 3 (6) | 0.563 |
| Bleomycin | 8 (6) | 3 (9) | 3 (6) | 2 (4) | 0.371 |
| Chemotherapeutic agents, mg/m2 (IQR) | |||||
| Alkylating agents combinedb | 11329 (5687–17164) | 11658 (7924–17391) | 11367 (5879–21425) | 8546 (4447–16131) | 0.199 |
| Busulfan | 443 (324–480) | 480 (470–587) | 344 (297–480) | 440 (374–449) | 0.021 |
| Carmustine | 300 (298–300) | 300 (298–351) | 300 (298–300) | 300 (291–306) | 0.737 |
| Cyclophosphamide | 4200 (3021–7535) | 7299 (4200–8684) | 4247 (3090–8230) | 3439 (2634–5258) | <0.001 |
| Ifosfamide | 9941 (4032–22500) | 11500 (5200–16032) | 10227 (4032–22500) | 8181 (4017–19767) | 0.477 |
| Lomustine | 395 (190–600) | 190 | – | 600 | 0.317 |
| Melphalan | 140 (139–169) | 140 (140–142) | 140 (140–140) | 140 (139–180) | 0.739 |
| Thiotepa | 680 (588–900) | 750 (168–900) | 749 (591–900) | 610 (307–900) | 0.921 |
| Bleomycin | 40 (40–46) | 42 (40–80) | 40 (40–50) | 30 (20–40) | 0.094 |
| Radiotherapy involving the thoraxc | 86 (65) | 25 (76) | 32 (63) | 29 (60) | 0.175 |
| Thoracic surgeryd | 12 (9) | 1 (3) | 5 (10) | 6 (13) | 0.157 |
| Transplant characteristics | |||||
| Remission status at transplantation | 0.906 | ||||
| First remission | 75 (57) | 16 (48) | 35 (69) | 24 (50) | |
| Relapsed disease | 57 (43) | 17 (52) | 16 (31) | 24 (50) | |
| Stem cell donor | 0.098 | ||||
| Autologous | 61 (46) | 17 (52) | 25 (49) | 19 (39) | |
| HLA identical sibling / HLA matched (un-)relative donor | 56 (42) | 16 (48) | 19 (37) | 21 (44) | |
| HLA mismatch (un-)related /haploidentical | 15 (11) | 0 | 7 (14) | 8 (17) | |
| Source of transplant | <0.001 | ||||
| Cord blood | 6 (5) | – | 1 (2) | 5 (10) | |
| Peripheral blood | 75 (57) | 9 (27) | 32 (63) | 34 (71) | |
| Bone marrow | 46 (35) | 22 (67) | 17 (33) | 7 (15) | |
| Unknown | 5 (4) | 2 (6) | 1 (2) | 2 (4) | |
| Pulmonary outcome | 26 (20) | 7 (21) | 11 (22) | 8 (17) | 0.582 |
HLA human leukocyte antigen, ICCC-3 International Classification of Childhood Cancer, 3rd edition, IQR interquartile range, N number, TBI total body irradiation.
*p value for trend.
aOther tumors include: tumors of the central nervous system (n = 6), retinoblastoma (n = 1), malignant bone tumors (n = 7), soft tissue sarcoma (n = 4), malignant germ cell tumors (n = 3).
bCombination according to Cyclophosphamide Equivalent Dose (CED) [27].
cThoracic radiation fields according to COG guidelines, Version 4.0, Oct 2018, including radiation to the chest, whole lung, mediastinum, (mini-)mantle field, TBI and additionally upper abdomen and thoracic spine, including craniospinal irradiation.
dThoracic surgery according to COG guidelines, Version 4.0, Oct 2018, including thoracotomy, chest wall surgery, rib resection, lobectomy, pulmonary metastasectomy and wedge resection.
Prevalence of pulmonary outcomes
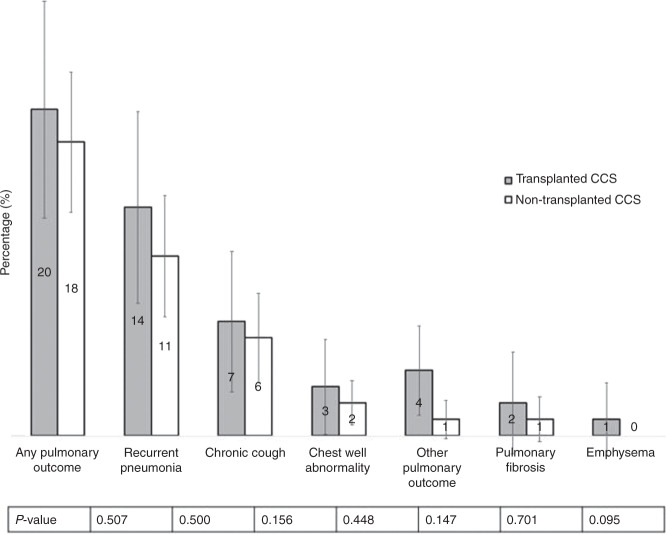
Any pulmonary outcome was reported as often in transplanted (20%) as in non-transplanted CCS (18%; p = 0.507). The occurrence of the listed pulmonary outcomes was not significantly different between transplanted and non-transplanted CCS. Pneumonia was the most frequently reported outcome (Fig. 1). The proportion of transplanted CCS reporting any pulmonary outcome did not change by era of transplantation (Table 2).
Fig. 1. Prevalence of self-reported pulmonary diseases and symptoms in transplanted (N = 132) and non-transplanted matched childhood cancer survivors (N = 368).
Error bars represent 95% confidence intervals. P value comparing prevalence between transplanted and non-transplanted survivors. *Total N reduced for pulmonary fibrosis and emphysema because question only asked in adolescents and adults: N = 85 transplanted survivors, N = 195 non-transplanted survivors. ** “Other pulmonary outcome” includes reduced lung function (n = 3) and pulmonary GvHD (n = 1).
Risk factors for pulmonary outcomes
In univariable logistic regression analysis, we found associations between older age at cancer diagnosis (increase per year; odds ratio [OR] 1.2, 95% confidence interval [CI] 1.05–1.28), exposure to bleomycin (OR 4.63, 95%CI 1.08–19.97), and thoracic surgery (OR 7.44, 95%CI 2.13–25.92) with any pulmonary outcome (Table 3). We found no significant association with era of diagnosis, treatment with other chemotherapeutics, median CED, and thoracic radiotherapy, but numbers were small. Transplant-related factors were also not significantly associated with reporting of pulmonary outcomes (Table 3). In multivariable logistic regression analysis, the effect of thoracic surgery was reduced to an OR of 3.91 (95%CI 0.95–16.02), suggesting that it has been confounded by other factors related to disease and treatment (Table 4). Most of the 12 CCS treated with thoracic surgery have been diagnosed with Ewing sarcoma (n = 7) or lymphoma (n = 4). All except one CCS have been transplanted autologous, most suffered from relapsed disease (n = 10), received radiotherapy to the chest (n = 10), were treated with open thoracic surgeries (n = 9), received at least one lung toxic chemotherapeutic agent (n = 7), or have been exposed to a combination of radiotherapy and thoracic surgery or resection of lung tissue (n = 9) (Supplementary Table S5).
Table 3.
Association between sociodemographic, clinical, treatment, and transplant characteristics on self-reported pulmonary outcomes.
| Reporting of any pulmonary outcome | ||||||
|---|---|---|---|---|---|---|
| noutcome | Ntotal | % | OR | 95% CI | p value* | |
| Sociodemographic and lifestyle characteristics | ||||||
| Sex | 0.795 | |||||
| Male | 13 | 69 | 19 | 1 | ||
| Female | 13 | 63 | 21 | 1.12 | 0.47–2.64 | |
| Age at questionnaire, continuous (years) | 26 | 132 | 20 | 1.05 | 0.99–1.11 | 0.088 |
| Smoking statusa | 0.924 | |||||
| Never smoking | 12 | 60 | 20 | 1 | ||
| Passive smoking | 10 | 56 | 18 | 0.87 | 0.34–2.21 | |
| Former active smoking | 2 | 9 | 22 | 1.14 | 0.21–6.21 | |
| Active smoking | 2 | 7 | 29 | 1.60 | 0.27–9.28 | |
| Clinical characteristics | ||||||
| Age at diagnosis, continuous (years) | 26 | 132 | 20 | 1.2 | 1.05–1.28 | 0.002 |
| Follow-up time, continuous (years) | 26 | 132 | 20 | 0.98 | 0.91–1.06 | 0.613 |
| Era of diagnosis | 0.800 | |||||
| 1976–1990 | 5 | 20 | 25 | 1 | ||
| 1991–2000 | 8 | 45 | 18 | 0.64 | 0.18–2.31 | |
| 2001–2010 | 13 | 67 | 19 | 0.72 | 0.22–2.35 | |
| Cancer diagnosis according to ICCC-3 | 0.271 | |||||
| Leukemia | 15 | 72 | 21 | 1 | ||
| Lymphoma | 5 | 20 | 25 | 1.27 | 0.39–4.04 | |
| Neuroblastoma | 1 | 19 | 5 | 0.21 | 0.03–1.71 | |
| Otherb | 5 | 21 | 24 | 1.18 | 0.37–3.76 | |
| Treatment characteristics | ||||||
| Bleomycin | 0.040 | |||||
| No | 22 | 124 | 18 | 1 | ||
| Yes | 4 | 8 | 50 | 4.63 | 1.08–19.97 | |
| Busulfan | 0.190 | |||||
| No | 16 | 95 | 17 | 1 | ||
| Yes | 10 | 37 | 27 | 1.83 | 0.74–4.51 | |
| Nitrosureas (BCNU and CCNU) | 0.107 | |||||
| No | 22 | 122 | 18 | 1 | ||
| Yes | 4 | 10 | 40 | 3.03 | 0.79–11.65 | |
| Cyclophosphamide | 0.844 | |||||
| No | 2 | 9 | 22 | 1 | ||
| Yes | 24 | 123 | 20 | 0.84 | 0.16–4.34 | |
| Ifosfamide | 0.596 | |||||
| No | 15 | 70 | 21 | 1 | ||
| Yes | 11 | 62 | 18 | 0.79 | 0.33–1.88 | |
| Melphalan | 0.281 | |||||
| No | 15 | 88 | 17 | 1 | ||
| Yes | 11 | 44 | 25 | 1.62 | 0.67–3.91 | |
| Treosulfan | 0.400 | |||||
| No | 24 | 126 | 19 | 1 | ||
| Yes | 2 | 6 | 33 | 2.12 | 0.36–12.28 | |
| Alkylating agentsc | 0.084 | |||||
| ≤11,300 mg/m2 | 9 | 66 | 14 | 1 | ||
| >11,300 mg/m2 | 17 | 66 | 26 | 2.19 | 0.89–5.37 | |
| Radiotherapy to chest (including TBI) | 0.165 | |||||
| No | 6 | 46 | 13 | 1 | ||
| Yes | 20 | 86 | 23 | 2.02 | 0.75–5.45 | |
| Thoracic surgery | <0.001 | |||||
| No | 19 | 120 | 16 | 1 | ||
| Yes | 7 | 12 | 58 | 7.44 | 2.13–25.92 | |
| Transplant characteristics | ||||||
| Remission status at transplantation | 0.223 | |||||
| First remission/primary refractory | 12 | 75 | 16 | 1 | ||
| Relapsed disease | 14 | 57 | 24 | 1.71 | 0.72–4.05 | |
| Type of transplantation | 0.995 | |||||
| Allogeneic | 14 | 71 | 20 | 1 | ||
| Autologous | 12 | 61 | 20 | 0.99 | 0.42–2.35 | |
| Stem cell donor | 0.739 | |||||
| Autologous | 12 | 61 | 20 | 1 | ||
| HLA ident. sibling, matched (un)related donor | 11 | 56 | 20 | 0.99 | 0.40–2.48 | |
| HLA mismatched (un)related, haploidentical | 3 | 15 | 20 | 1.02 | 0.25–4.19 | |
| Source of transplant (n = 66)d | 0.933 | |||||
| Bone marrow | 7 | 34 | 21 | 1 | ||
| Peripheral blood | 6 | 26 | 23 | 1.15 | 0.34–3.98 | |
| Cord blood | 1 | 6 | 17 | 0.77 | 0.08–7.71 | |
| Graft versus host disease (n = 71)d | 0.449 | |||||
| No | 4 | 15 | 27 | 1 | ||
| Yes | 10 | 56 | 18 | 0.59 | 0.16–2.27 | |
Results from univariable logistic regression analysis. N = 132, median age at study 18.4 years.
BCNU Lomustine, CCNU Carmustine, HLA human leukocyte antigen, ICCC-3 International Classification of Childhood Cancer, 3rd edition, OR Odds ratio, TBI total body irradiation, CI confidence interval.
*p value calculate by logistic regression (Wald test) for continuous and binary independent variables and by likelihood ratio test for independent variables with >2 categories.
aActive and former active smoking assessed in adolescents and adults. Passive and never smoking assessed in children, adolescent and adults.
bOther diagnostic groups include: malignant bone tumors (n = 7), tumors of the central nervous system (n = 6), soft tissue sarcomas (n = 4), germ cell tumors (n = 3), retinoblastoma (n = 1).
cCumulative alkylating dose according to cyclophosphamide equivalent dose (CED); categorized in smaller or equal to the median or larger as the median cumulative dose.
dIn survivors undergone allogeneic transplantation only.
Table 4.
Association between sociodemographic, clinical, treatment, and transplant characteristics on self-reported pulmonary outcomes.
| OR | 95% CI | p value | |
|---|---|---|---|
| Age at diagnosis | 1.13 | 0.99–1.28 | 0.055 |
| Age at questionnaire | 1.00 | 0.91–1.08 | 0.892 |
| Bleomycin exposure | 1.57 | 0.28–8.81 | 0.608 |
| Median CED dose >11,300 mg/m2 | 1.74 | 0.57–5.33 | 0.330 |
| Thoracic surgery | 3.91 | 0.95–16.02 | 0.058 |
| Thoracic radiotherapy | 1.58 | 0.49–5.14 | 0.446 |
Results from multivariable logistic regression analysis, adjusted for all factors in the table. N = 132, median 18.4 years at study.
CED cyclophosphamide equivalent dose, CI confidence interval, OR Odds ratio.
Discussion
This nationwide population-based cohort study found that transplant characteristics changed over time with fewer HSCT recipients receiving TBI or lung toxic chemotherapeutics. One-fifth of ≥5-year CCS reported at least one pulmonary outcome 10 years after cancer diagnosis irrespective of whether they had been transplanted or not. Our analyses point to older age at diagnosis and thoracic surgery as possible risk factors for self-reported pulmonary outcomes.
TBI is a crucial component of conditioning regimens for allogeneic HSCT, but known to be lung toxic. Even though TBI cannot completely be replaced by chemotherapy, such as in acute lymphoblastic leukemia [33], we found that the use of TBI has become less common in more recent eras. There was a non-significant trend towards lower cumulative doses of bleomycin and we found no evidence for a change in cumulative doses of carmustine, but numbers were small. The increasing use of peripheral blood stem cells in more recent eras is in line with literature [34–36] and the increasing use of mismatched (un-) related donors reflects the overall progress in HSCT over time.
The proportion of transplanted CCS reporting any pulmonary outcome did not change during the three HSCT eras. Studies that compared self-reported pulmonary outcomes in transplanted CCS are few. Fanfulla et al. examined children during the first 18 months after allogeneic HSCT [22]. Cough was reported by 15–25% of children and pneumonia was diagnosed in the first 6 months in 19% of children. The occurrence of pneumonia in the first 6 months, is indicative of delayed immune reconstitution rather than late pulmonary outcomes. Since the follow-up (18 months) is shorter than in our population (10 years) direct comparison is difficult. Also in the entire cohort of Swiss CCS (N = 1 894) pneumonia was the most frequently reported pulmonary outcome (10%), and pulmonary fibrosis (0.8%) and emphysema (0.2%) were reported by few CCS [20]. CCS in the North American Childhood Cancer Survivor Study showed a different distribution of pulmonary outcomes with chronic cough being the most frequent outcome (7.8%), followed by pulmonary fibrosis (1.9%), and recurrent pneumonia (1.7%) [21]. We found no difference in the prevalence of pulmonary outcomes between transplanted and non-transplanted CCS in our study (20% vs. 18%). This could be explained by the high proportion of leukemia (58%) and lymphoma (16%) diagnoses in non-transplanted CCS due to the matching. A Danish cohort study included 94 leukemia survivors a median of 10 years from diagnosis, treated with chemotherapy only, and 11% suffered from pulmonary problems, mainly cough [37]. A US study including Hodgkin’s lymphoma survivors treated with chest radiation but without HSCT showed that 17% had at least one episode of pneumonia and 9% reported dyspnea [38].
CCS who had undergone thoracic surgery in addition to HSCT reported more pulmonary outcomes than those without thoracic surgery. This might be because this group of CCS had received more often thoracic radiotherapy or lung toxic chemotherapeutics, had more often been diagnosed with relapsed disease, and underwent open thoracic surgeries in most cases, which goes along with a more intensive treatment. Residual confounding by these additional lung toxic treatment modalities probably leads to an overestimation of the association between thoracic surgery and pulmonary outcomes. Older age at diagnosis, resulting in older age at HSCT, was another risk factor for pulmonary outcomes in univariable analysis. No study has assessed self-reported pulmonary outcomes in the context of age at HSCT, but four studies showed an association between older age at HSCT and deterioration in selected pulmonary function parameters [23, 39–41]. In multivariable analysis, bleomycin was not a risk factor for pulmonary outcomes anymore, which is in line with findings from the whole Swiss CCS cohort [20]. In our cohort, we found no significant effect of other selected chemotherapeutics and transplant-related factors on the reporting of pulmonary outcomes. All studies that evaluated the impact of cGvHD on the lung, used pulmonary function tests as outcome measure [41–44]. They reported a negative effect of cGvHD on pulmonary function. We explain the missing effect of cGvHD, lomustine, and carmustine by the low number of survivors exposed to each of these factors. Also some CCS with severe pulmonary cGvHD might have died before receiving the SCCSS questionnaire and missing or non-detailed documentation in the medical records might have led to an underestimation of the effect of cGvHD on pulmonary outcomes.
We found no difference in pulmonary outcomes between CCS treated with autologous and allogeneic HSCT. Thoracic surgery was overrepresented in the autologous group because of the underlying diagnoses, mainly bone tumors. In contrast, CCS treated with allogeneic HSCT were more often exposed to chest radiotherapy, which can lead to radiation pneumonitis and an increased risk of interstitial pneumonitis due to infections such as CMV. Both factors have not been assessed in detail.
The strengths of this study include the population-based national design of the SCCSS, the high response rate of transplanted CCS (71%), and the comparability between responding and nonresponding transplanted survivors. This makes us confident, that our results can be extrapolated to ≥5-year Swiss survivors who underwent HSCT. In addition, the completeness of exact treatment exposure, including cumulative doses of chemotherapeutics and detailed information on HSCT in transplanted CCS is another strength.
The reliance on self-reported outcome data is a limitation and our study did not include objective pulmonary function tests. CCS treated with open thoracic surgery are reminded by the scar of their history and thus may be more sensitive in dealing with their lung health, and may remember and report pulmonary outcomes better. However, Louie et al. reported a high agreement between self-reported pulmonary outcomes, such as chronic cough, pulmonary fibrosis, and emphysema, and their validation by extractions from medical records (sensitivity 96.2%; specificity 90.8%) [45]. The SCCSS has not been designed for survivors after HSCT specifically, neither for the assessment of pulmonary outcomes only and did not include specific questions on exertion-induced dyspnea or effort intolerance. This might have led to underreporting of pulmonary outcomes in our study. Also “pneumonia” might have been misunderstood by lay persons, as it was not defined in the questionnaire. Survival bias due to inclusion of ≥5-year survivors could have led to underestimation of pulmonary outcomes as more severely affected patients might have died. The small number of transplanted CCS who have been exposed to specific chemotherapeutics and transplant-related exposures did not allow for a multivariable analysis of all exposures in a single model. Also the detailed information on treatment exposures, such as cumulative doses, was only available for transplanted CCS. Finally, the absolute numbers of CCS reporting pulmonary outcomes was small, because the study population was young with a relatively short follow-up time, and the incidence of pulmonary outcomes increases over lifetime [20, 21, 39, 46].
In summary, we found that one-fifth of CCS, including those who underwent HSCT and matched controls, developed long-term pulmonary outcomes. As we only assessed self-reported outcomes, using a limited number of questions, this proportion probably only represents the tip of the iceberg. This underlines that we should implement long-term pulmonary follow-up recommendations on a large scale [13, 47–49] using sensitive outcome measures, such as lung function tests, to assess the full spectrum of long-term pulmonary sequelae after childhood cancer at an early stage.
Supplementary information
Acknowledgements
We thank all childhood cancer patients and families for participating in our survey. We thank the study team of the SCCR (Luzius Mader, Sven Strebel, Nicolas Waespe), Marcel Zwahlen for statistical support, the data managers of the SPOG (Claudia Althaus, Nadine Assbichler, Pamela Balestra, Heike Baumeler, Nadine Beusch, Sarah Blanc, Susann Drerup, Janine Garibay, Franziska Hochreutener, Monika Imbach, Friedgard Julmy, Eléna Lemmel, Rodolfo Lo Piccolo, Heike Markiewicz, Veneranda Mattielo, Annette Reinberg, Renate Siegenthaler, Astrid Schiltknecht, Beate Schwenke, and Verena Stahel) and the data managers and administrative staff of the SCCR (Meltem Altun, Erika Brantschen, Katharina Flandera, Elisabeth Kiraly, Nadine Lötscher, Verena Pfeiffer, Shelagh Redmond, Julia Ruppel, and Ursina Roder). This study is supported by Swiss Cancer League (KLS-3886-02-2016), Swiss Cancer Research (KFS-4157-02-2017 and KFS-4722-02-2019), and Lung League Bern.
The Swiss Pediatric Oncology Group (SPOG)
M. Ansari6,7, M. Beck Popovic13, J. P. Bourquin14, P. Brazzola15, J. Greiner16, J. Rössler12, F. Schilling17, K. Scheinemann2,8,9, N. von der Weid4
Funding
Open access funding provided by University of Bern.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Members of the Swiss Pediatric Oncology Group (SPOG) are listed below Acknowledgements.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Claudia E. Kuehni, Email: claudia.kuehni@ispm.unibe.ch
for the Swiss Pediatric Oncology Group (SPOG):
M. Ansari, M. Beck Popovic, J. P. Bourquin, P. Brazzola, J. Greiner, J. Rössler, F. Schilling, K. Scheinemann, and N. von der Weid
Supplementary information
The online version of this article (10.1038/s41409-020-01137-1) contains supplementary material, which is available to authorized users.
References
- 1.Merli P, Algeri M, Del Bufalo F, Locatelli F. Hematopoietic stem cell transplantation in pediatric acute lymphoblastic leukemia. Curr Hematologic Malignancy Rep. 2019;14:94–105. doi: 10.1007/s11899-019-00502-2. [DOI] [PubMed] [Google Scholar]
- 2.Yalcin B, Kremer LC, van Dalen EC. High-dose chemotherapy and autologous haematopoietic stem cell rescue for children with high-risk neuroblastoma. Cochrane Database Syst Rev. 2015:Cd006301. [DOI] [PMC free article] [PubMed]
- 3.Guerra JA, Dhall G, Marachelian A, Castillo E, Malvar J, Wong K, et al. Marrow-ablative chemotherapy followed by tandem autologous hematopoietic cell transplantation in pediatric patients with malignant brain tumors. Bone Marrow Transplant. 2017;52:1543–8. doi: 10.1038/bmt.2017.166. [DOI] [PubMed] [Google Scholar]
- 4.Shankar A, Hayward J, Kirkwood A, McCarthy K, Hewitt M, Morland B, et al. Treatment outcome in children and adolescents with relapsed Hodgkin lymphoma–results of the UK HD3 relapse treatment strategy. Br J Haematol. 2014;165:534–44.. doi: 10.1111/bjh.12768. [DOI] [PubMed] [Google Scholar]
- 5.Niethammer D, Bader P, Handgretinger R, Klingebiel T. Stem cell transplantation. Klinische Padiatrie. 2013;225(Suppl 1):S94–8. doi: 10.1055/s-0033-1337970. [DOI] [PubMed] [Google Scholar]
- 6.Dopfer R, Henze G, Bender-Gotze C, Ebell W, Ehninger G, Friedrich W, et al. Allogeneic bone marrow transplantation for childhood acute lymphoblastic leukemia in second remission after intensive primary and relapse therapy according to the BFM- and CoALL-protocols: results of the German Cooperative Study. Blood. 1991;78:2780–4. [PubMed] [Google Scholar]
- 7.Diab M, ZazaDitYafawi J, Soubani AO. Major pulmonary complications after hematopoietic stem cell transplant. Exp Clin Transplant: Off J Middle East Soc Organ Transplant. 2016;14:259–70. doi: 10.6002/ect.2015.0275. [DOI] [PubMed] [Google Scholar]
- 8.Soubani AO, Pandya CM. The spectrum of noninfectious pulmonary complications following hematopoietic stem cell transplantation. Hematol/Oncol Stem Cell Ther. 2010;3:143–57.. doi: 10.1016/s1658-3876(10)50025-6. [DOI] [PubMed] [Google Scholar]
- 9.Collaco JM, Gower WA, Mogayzel PJ., Jr Pulmonary dysfunction in pediatric hematopoietic stem cell transplant patients: overview, diagnostic considerations, and infectious complications. Pediatr Blood Cancer. 2007;49:117–26.. doi: 10.1002/pbc.21061. [DOI] [PubMed] [Google Scholar]
- 10.Huang TT, Hudson MM, Stokes DC, Krasin MJ, Spunt SL, Ness KK. Pulmonary outcomes in survivors of childhood cancer: a systematic review. Chest. 2011;140:881–901. doi: 10.1378/chest.10-2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skinner R, Kaplan R, Nathan PC. Renal and pulmonary late effects of cancer therapy. Semin Oncol. 2013;40:757–73.. doi: 10.1053/j.seminoncol.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Versluys AB, Bresters D. Pulmonary complications of childhood cancer treatment. Paediatr Respiratory Rev. 2016;17:63–70. doi: 10.1016/j.prrv.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 13.COG COG. Children’s Oncology Group [COG] Long Term Follow-Up guidelines Version 5.0 2018. 2019. http://www.survivorshipguidelines.org/pdf/2018/COG_LTFU_Guidelines_v5.pdf.
- 14.Sano H, Kobayashi R, Iguchi A, Suzuki D, Kishimoto K, Yasuda K, et al. Risk factor analysis of idiopathic pneumonia syndrome after allogeneic hematopoietic SCT in children. Bone Marrow Transplant. 2014;49:38–41. doi: 10.1038/bmt.2013.123. [DOI] [PubMed] [Google Scholar]
- 15.Hildebrandt GC, Fazekas T, Lawitschka A, Bertz H, Greinix H, Halter J, et al. Diagnosis and treatment of pulmonary chronic GVHD: report from the consensus conference on clinical practice in chronic GVHD. Bone Marrow Transplant. 2011;46:1283. doi: 10.1038/bmt.2011.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshihara S, Yanik G, Cooke KR, Mineishi S. Bronchiolitis obliterans syndrome (BOS), bronchiolitis obliterans organizing pneumonia (BOOP), and other late-onset noninfectious pulmonary complications following allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2007;13:749–59.. doi: 10.1016/j.bbmt.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Fidler MM, Kobayashi RC, Bright CJ, Henson KE, Kelly JS, Jenney M, et al. Respiratory mortality of childhood, adolescent and young adult cancer survivors. Thorax. 2018;73:959–68. doi: 10.1136/thoraxjnl-2017-210683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reulen RC, Winter DL, Frobisher C, Lancashire ER, Stiller CA, Jenney ME, et al. Long-term cause-specific mortality among survivors of childhood cancer. Jama. 2010;304:172–9. doi: 10.1001/jama.2010.923. [DOI] [PubMed] [Google Scholar]
- 19.Kirchhoff AC, Fluchel MN, Wright J, Ying J, Sweeney C, Bodson J, et al. Risk of hospitalization for survivors of childhood and adolescent cancer. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology. 2014;23:1280–9. doi: 10.1158/1055-9965.EPI-13-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kasteler R, Weiss A, Schindler M, Sommer G, Latzin P, von der Weid NX, et al. Long-term pulmonary disease among Swiss childhood cancer survivors. Pediatric Blood Cancer. 2018;65. [DOI] [PubMed]
- 21.Dietz AC, Chen Y, Yasui Y, Ness KK, Hagood JS, Chow EJ, et al. Risk and impact of pulmonary complications in survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Cancer. 2016;122:3687–96.. doi: 10.1002/cncr.30200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fanfulla F, Locatelli F, Zoia MC, Giorgiani G, Bonetti F, Spagnolatti L, et al. Pulmonary complications and respiratory function changes after bone marrow transplantation in children. Eur Respiratory J. 1997;10:2301–6. doi: 10.1183/09031936.97.10102301. [DOI] [PubMed] [Google Scholar]
- 23.Wieringa J, van Kralingen KW, Sont JK, Bresters D. Pulmonary function impairment in children following hematopoietic stem cell transplantation. Pediatr Blood Cancer. 2005;45:318–23.. doi: 10.1002/pbc.20304. [DOI] [PubMed] [Google Scholar]
- 24.Kuehni CE, Rueegg CS, Michel G, Rebholz CE, Strippoli MP, Niggli FK, et al. Cohort profile: the Swiss childhood cancer survivor study. Int J Epidemiol. 2012;41:1553–64.. doi: 10.1093/ije/dyr142. [DOI] [PubMed] [Google Scholar]
- 25.Michel G, von der Weid NX, Zwahlen M, Adam M, Rebholz CE, Kuehni CE. The Swiss childhood cancer registry: rationale, organisation and results for the years 2001-2005. Swiss Med Wkly. 2007;137:502–9. doi: 10.4414/smw.2007.11875. [DOI] [PubMed] [Google Scholar]
- 26.Mertens AC, Yasui Y, Liu Y, Stovall M, Hutchinson R, Ginsberg J, et al. Pulmonary complications in survivors of childhood and adolescent cancer. A report from the Childhood Cancer Survivor Study. Cancer. 2002;95:2431–41.. doi: 10.1002/cncr.10978. [DOI] [PubMed] [Google Scholar]
- 27.Green DM, Nolan VG, Goodman PJ, Whitton JA, Srivastava D, Leisenring WM, et al. The cyclophosphamide equivalent dose as an approach for quantifying alkylating agent exposure: a report from the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2014;61:53–67. doi: 10.1002/pbc.24679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ciurea SO, Andersson BS. Busulfan in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2009;15:523–36.. doi: 10.1016/j.bbmt.2008.12.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fleischhauer K. Selection of matched unrelated donors moving forward: from HLA allele counting to functional matching. Hematol Am Soc Hematol Educ Program. 2019;2019:532–8. doi: 10.1182/hematology.2019000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eyrich M, Schulze H. HLA Matching in Pediatric Stem Cell Transplantation. Transfus Med hemotherapy: offizielles Organ der Dtsch Ges fur Transfusionsmedizin und Immunhamatologie. 2019;46:348–55.. doi: 10.1159/000502422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P. International classification of childhood cancer, third edition. Cancer. 2005;103:1457–67.. doi: 10.1002/cncr.20910. [DOI] [PubMed] [Google Scholar]
- 32.Software S STATA manual: nptrend [22.04.2020]. https://www.stata.com/manuals13/rnptrend.pdf.
- 33.Willasch AM, Peters C, Sedlacek P, Dalle JH, Kitra-Roussou V, Yesilipek A, et al. Myeloablative conditioning for allo-HSCT in pediatric ALL: FTBI or chemotherapy?-A multicenter EBMT-PDWP study. Bone Marrow Transplant. 2020;55:1540–51. doi: 10.1038/s41409-020-0854-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eapen M, Horowitz MM, Klein JP, Champlin RE, Loberiza FR, Jr, Ringden O, et al. Higher mortality after allogeneic peripheral-blood transplantation compared with bone marrow in children and adolescents: the Histocompatibility and Alternate Stem Cell Source Working Committee of the International Bone Marrow Transplant Registry. J Clin Oncol. 2004;22:4872–80.. doi: 10.1200/JCO.2004.02.189. [DOI] [PubMed] [Google Scholar]
- 35.Simonin M, Dalissier A, Labopin M, Willasch A, Zecca M, Mouhab A, et al. More chronic GvHD and non-relapse mortality after peripheral blood stem cell compared with bone marrow in hematopoietic transplantation for paediatric acute lymphoblastic leukemia: a retrospective study on behalf of the EBMT Paediatric Diseases Working Party. Bone Marrow Transplant. 2017;52:1071–3. doi: 10.1038/bmt.2017.66. [DOI] [PubMed] [Google Scholar]
- 36.Pulsipher MA, Levine JE, Hayashi RJ, Chan KW, Anderson P, Duerst R, et al. Safety and efficacy of allogeneic PBSC collection in normal pediatric donors: the pediatric blood and marrow transplant consortium experience (PBMTC) 1996-2003. Bone Marrow Transplant. 2005;35:361–7. doi: 10.1038/sj.bmt.1704743. [DOI] [PubMed] [Google Scholar]
- 37.Nysom K, Holm K, Olsen JH, Hertz H, Hesse B. Pulmonary function after treatment for acute lymphoblastic leukaemia in childhood. Br J Cancer. 1998;78:21–7. doi: 10.1038/bjc.1998.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Venkatramani R, Kamath S, Wong K, Olch AJ, Malvar J, Sposto R, et al. Pulmonary outcomes in patients with Hodgkin lymphoma treated with involved field radiation. Pediatr Blood Cancer. 2014;61:1277–81. doi: 10.1002/pbc.24969. [DOI] [PubMed] [Google Scholar]
- 39.Inaba H, Yang J, Pan J, Stokes DC, Krasin MJ, Srinivasan A, et al. Pulmonary dysfunction in survivors of childhood hematologic malignancies after allogeneic hematopoietic stem cell transplantation. Cancer. 2010;116:2020–30.. doi: 10.1002/cncr.24897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ginsberg JP, Aplenc R, McDonough J, Bethel J, Doyle J, Weiner DJ. Pre-transplant lung function is predictive of survival following pediatric bone marrow transplantation. Pediatr Blood Cancer. 2010;54:454–60.. doi: 10.1002/pbc.22337. [DOI] [PubMed] [Google Scholar]
- 41.Leung W, Ahn H, Rose SR, Phipps S, Smith T, Gan K, et al. A prospective cohort study of late sequelae of pediatric allogeneic hematopoietic stem cell transplantation. Medicine. 2007;86:215–24.. doi: 10.1097/MD.0b013e31812f864d. [DOI] [PubMed] [Google Scholar]
- 42.Madanat-Harjuoja LM, Valjento S, Vettenranta K, Kajosaari M, Dyba T, Taskinen M. Pulmonary function following allogeneic stem cell transplantation in childhood: a retrospective cohort study of 51 patients. Pediatr Transplant. 2014;18:617–24.. doi: 10.1111/petr.12313. [DOI] [PubMed] [Google Scholar]
- 43.Uderzo C, Pillon M, Corti P, Tridello G, Tana F, Zintl F, et al. Impact of cumulative anthracycline dose, preparative regimen and chronic graft-versus-host disease on pulmonary and cardiac function in children 5 years after allogeneic hematopoietic stem cell transplantation: a prospective evaluation on behalf of the EBMT Pediatric Diseases and Late Effects Working Parties. Bone Marrow Transplant. 2007;39:667–75.. doi: 10.1038/sj.bmt.1705652. [DOI] [PubMed] [Google Scholar]
- 44.Hoffmeister PA, Madtes DK, Storer BE, Sanders JE. Pulmonary function in long-term survivors of pediatric hematopoietic cell transplantation. Pediatr Blood Cancer. 2006;47:594–606. doi: 10.1002/pbc.20531. [DOI] [PubMed] [Google Scholar]
- 45.Louie AD, Robison LL, Bogue M, Hyde S, Forman SJ, Bhatia S. Validation of self-reported complications by bone marrow transplantation survivors. Bone Marrow Transplant. 2000;25:1191–6. doi: 10.1038/sj.bmt.1702419. [DOI] [PubMed] [Google Scholar]
- 46.Kaya Z, Weiner DJ, Yilmaz D, Rowan J, Goyal RK. Lung function, pulmonary complications, and mortality after allogeneic blood and marrow transplantation in children. Biol Blood Marrow Transplant. 2009;15:817–26.. doi: 10.1016/j.bbmt.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 47.Chow EJ, Anderson L, Baker KS, Bhatia S, Guilcher GMT, Huang JT, et al. Late effects surveillance recommendations among survivors of childhood hematopoietic cell transplantation: a Children’s Oncology Group Report. Biol Blood Marrow Transplant. 2016;22:782–95.. doi: 10.1016/j.bbmt.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dietz AC, Duncan CN, Alter BP, Bresters D, Cowan MJ, Notarangelo L, et al. The second pediatric blood and marrow transplant consortium international consensus conference on late effects after pediatric hematopoietic cell transplantation: defining the unique late effects of children undergoing hematopoietic cell transplantation for immune deficiencies, inherited marrow failure disorders, and hemoglobinopathies. Biol Blood Marrow Transplant. 2017;23:24–9. doi: 10.1016/j.bbmt.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shenoy S, Gaziev J, Angelucci E, King A, Bhatia M, Smith A, et al. Late effects screening guidelines after hematopoietic cell transplantation (HCT) for hemoglobinopathy: consensus statement from the second pediatric blood and marrow transplant consortium international conference on late effects after pediatric HCT. Biol Blood Marrow Transplant. 2018;24:1313–21. doi: 10.1016/j.bbmt.2018.04.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.