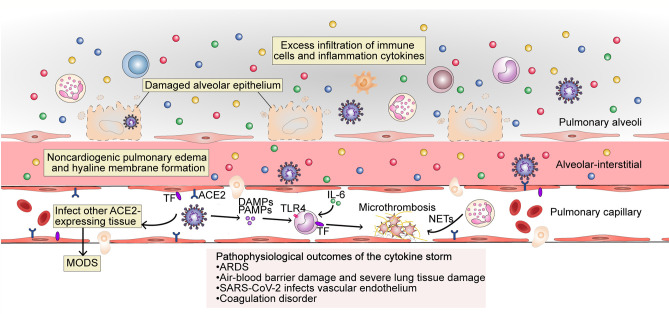
Figure 3.
The pathophysiological outcome of the cytokine storm in SARS-CoV-2 infection. The excess filtration of immune cells and accumulation of cytokines at infected sites results in acute respiratory distress syndrome (ARDS); non-cardiogenic pulmonary edema and hyaline membrane formation; severe lung tissue damage; and destruction of the blood–blood barrier. SARS-CoV-2 can infect vascular endothelial cells that also express ACE2 and enter the blood circulation to infect other ACE2-expressing tissues. The occurrence of an inflammatory storm in other organs may lead to MODS. PAMPs, DAMPs and cytokines trigger monocyte activation and induce the membrane expression of TF on monocytes and endothelial cells. Endothelial damage can also expose TF. Under the action of cytokines (mainly IL-6), endothelial cells recruit TF-expressing inflammatory monocytes, while TF can also promote the conversion of prothrombin to thrombin, forming a fibrin-based blood clot. Recruited by activated endothelial cells, neutrophils release NETs, which activate the contact activation pathway of coagulation and platelets, thereby amplifying blood clotting. MODS, multi-organ dysfunction syndrome; TF, tissue factor; TLR, Toll-like receptor; NETs, neutrophil extracellular traps.