Abstract
Background:
Psoriasis is a chronic incurable disease, and patients develop associated diseases such as obesity, diabetes, high blood pressure, dyslipidemia.
Objective:
The aim of the study is to determine the frequency of comorbidities (obesity, diabetes, dyslipidemia, high blood pressure) in men with psoriasis, and the relationship between the duration of psoriasis and the occurrence of comorbidities.
Methods:
A prospective study was conducted and included 88 male subjects, mean age 52,70 (SD=± 14,05) years, mean psoriasis duration 15,13 (SD=±12,43) years.
Results:
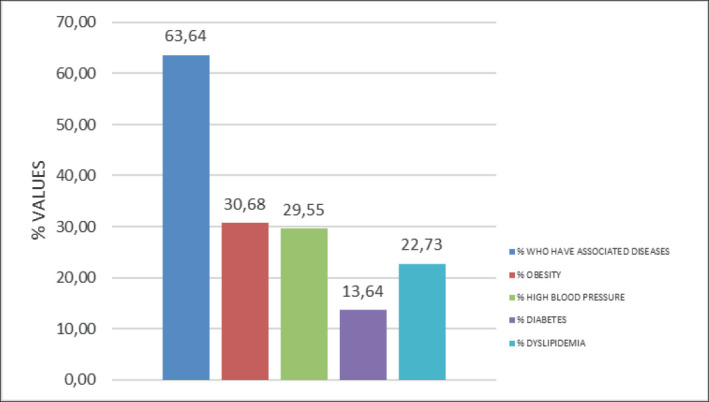
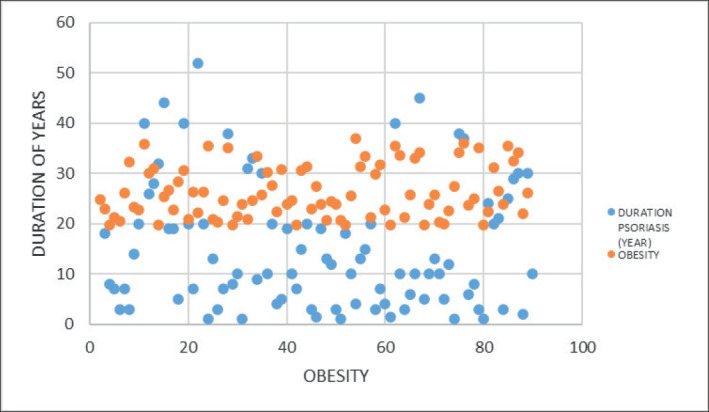
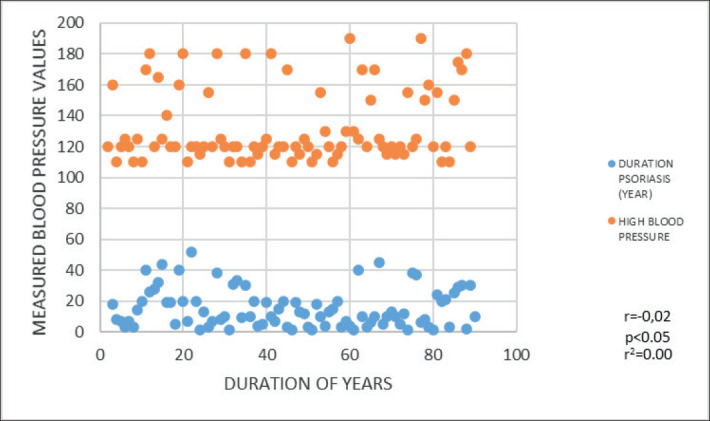
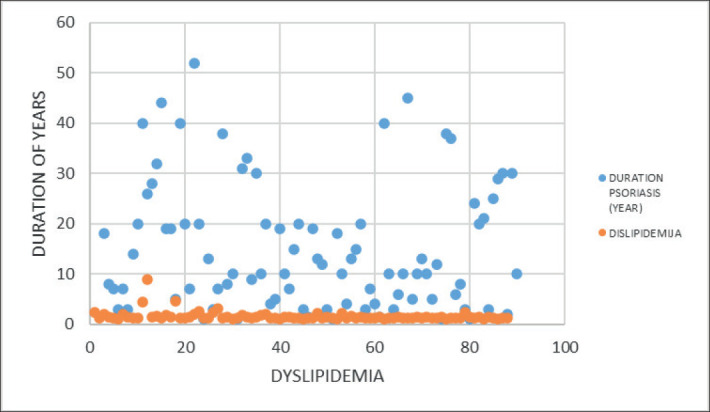
The incidence of obesity was 30,68%, high blood pressure 29,55%, dyslipidemia 22,73%, diabetes 13,64%. There was a weak correlation between the duration of psoriasis and the occurrence of obesity (r=0,11), dyslipidemia (r=0,18), diabetes (r=0,01), and high blood pressure (r=-0,02).
Conclusion:
Comorbidities occur in men with psoriasis, and their occurrence is not related to the duration of the disease.
Keywords: psoriasis, comorbidities, men
1. BACKGROUND
Psoriasis is a chronic inflammatory disease with multiple comorbidities (1). Studies in patients with psoriasis have shown an increased incidence of comorbidities, such as obesity, metabolic syndrome, high blood pressure, dyslipidemia, diabetes (2-5). Although the exact mechanisms of this association are not known, the occurrence of comorbidity is considered to be responsible for the state of chronic inflammation present in patients with psoriasis and elevated levels of proinflammatory cytokines (6). In addition, genetic factors (7), lifestyle of patients (diet, physical activity, habits), prejudices and stigmatization of patients (8) influence. Studies show that the risk of comorbidities, including cardiovascular diseases, is higher in patients with a longer duration of psoriasis (9, 10).
2. OBJECTIVE
To determine the frequency of comorbidities (obesity, diabetes, dyslipidemia, high blood pressure) in men with psoriasis, and the relationship between the duration of psoriasis and the occurrence of comorbidities.
3. PATIENTS AND METHODS
A prospective study was conducted that included 88 men with psoriasis over the age of 18. The mean age of the subjects was 52,70 (SD=±14,05) years. The average duration of psoriasis was 15,13 (SD=±12,43) years. The prevalence of psoriasis was: psoriasis vulgaris 86,36%, psoriasis guttata 13,64% of respondents. Respondents were introduced to the manner and purpose of the research, and signed a written consent to participate in the research. The study included men with psoriasis diagnosed with psoriasis pathohistologically. The study did not include subjects who, in addition to psoriasis, also suffer from another skin disease, who have been suffering from psoriasis for less than a year and who use systemic therapy.
The research was approved by the Ethics Committee of the University Clinical Center.
Anamnesis was taken, including data on psoriasis, when it was started, which therapy was used, data on psoriasis in the family. A dermatological examination of the skin and visible mucous membranes was then performed. Determining the presence, that is diagnosing obesity, high blood pressure, diabetes and dyslipidemia was performed by examination by an internist (internist’s findings).
Sugar and fat values were measured by standard biochemical procedures, after taking a venous blood sample from subjects who did not eat during the night for at least 8 hours.
The reference values are:
Reference values for lipids are: cholesterol ≤ 5,2 mmol/l, triglycerides ≤ 1,7 mmol/l.,
Glucose reference values are: ≤ 5,6 mmol/l.
Reference values of blood pressure are: <130/85mmHg.
Body mass index (BMI) was determined for all subjects.
Body weight (expressed in kg) and body height (expressed in cm) were measured.
Then the body mass index was calculated by the formula: body weight in kg divided by body height expressed in meters squared:
BMI = body weight (kg)/body height (m)2
The reference values are:
Malnutrition, BMI lower 18,5 kg/m2
Normal body weight, BMI 18,5-24,9 kg/m2
Overweight, BMI 25,0 to 29,9 kg/m2
Obesity, BMI greater than 30 kg/m2
Statistical analysis
Actual data, which were processed in Microsoft Excel, were used for statistical data processing and obtaining results. Intergroup differences determined by mean with standard deviation. The correlation between the two variables was performed by Pearson’s correlation coefficient (since they are linear models). The lowest value of the significance level is p <0,05.
4. RESULTS
The mean age of the subjects was 52,70 (SD=±14,05) years. The average duration of psoriasis was 15,13 (SD=±12,43) years. The representation of psoriasis was: psoriasis vulgaris 86,36%, psoriasis guttata 13,64% of respondents.
One associated disease was present in 40,91% of subjects, two associated diseases were present in 15,91% of subjects, three associated diseases were present in 3,41% of subjects, and four associated diseases were present in 3,41% of subjects.
The value of the correlation coefficient, that is the product-moment coefficient of disease duration and obesity is r=0,11, which indicates a weak correlation, and when we talk about the strength of the connection, it indicates a weak relationship between these two variables.
The value of the correlation coefficient, that is the product-moment coefficient of the duration of the disease and high blood pressure is r=-0.02, which indicates a relatively weak negative correlation, and when we talk about the strength of the connection, it indicates a weak relationship between these two variables.
The value of the correlation coefficient, that is the product-moment coefficient of the duration of the disease and dyslipidemia is r=0,18, which indicates a weak correlation, and when we talk about the strength of the connection, it indicates a weak connection between these two variables.
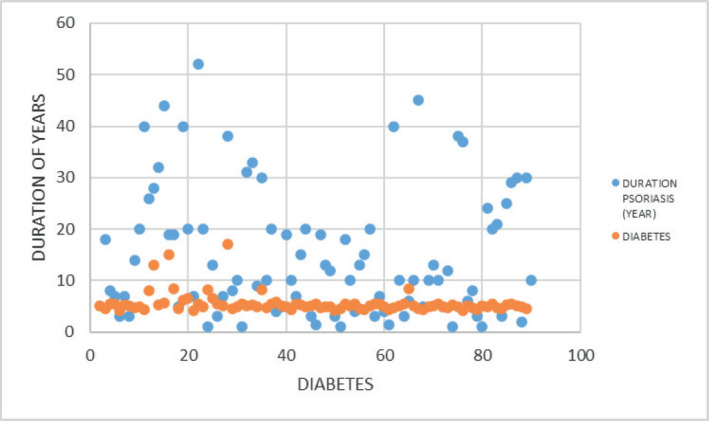
The value of the correlation coefficient, that is the product-moment coefficient of the duration of the disease and diabetes is r=0,01, which indicates a weak correlation, and when we talk about the strength of the connection, it indicates a weak connection between these two variables.
.5. DISCUSSION
Psoriasis is a chronic disease of unknown cause. In this study, we examined comorbidity in men with psoriasis, and the relationship between the duration of psoriasis and the occurrence of comorbidity. Thus, the incidence of obesity was 30,68%, high blood pressure 29,55%, dyslipidemia 22,73%, diabetes 13,64%. Other studies have also shown a higher incidence of obesity, diabetes, dyslipidemia, and high blood pressure in patients with psoriasis (11-17).
Although we did not find comorbidity research exclusively in men with psoriasis in the available literature, in a study in Taiwan, there were more male subjects and it was shown that men have a higher incidence of high blood pressure, diabetes, dyslipidemia (18). Men also have higher BMI values than women (19). In a study in Japan, where the majority of respondents were men, they were found to be more likely to get psoriasis if they were obese (20). Other studies also showed the occurrence of associated diseases in patients with psoriasis, so a study that included more men (they made up about 70% of the sample) showed an incidence of obesity of 34,5%, high blood pressure 63,1%, and high blood sugar 28,1% (21). Dyslipidemia was more common in psoriatic patients was shown by a study that had more male subjects (22) but also other studies on dyslipidemia in patients with psoriasis (23-25).
Regarding the association, that is the influence of the duration of psoriasis on the occurrence of comorbidities, in this study there was a weak correlation, that is the association of the duration of psoriasis and the occurrence of obesity (r=0,11), dyslipidemia (r=0,18), diabetes (r=0,01), and high blood pressure (r=-002). Other studies have shown the effect of the duration of psoriasis on the occurrence of comorbidities, so in a study in Malaysia that examined the incidence of comorbidities in psoriasis patients, the incidence of high blood pressure in psoriasis patients was 25,9%, and was more common if psoriasis lasted longer, it develops later (26). Also, Santos et al. (27) showed that patients with psoriasis with comorbidity, dyslipidemia, and obesity had a longer duration of psoriasis than those without these comorbidities. The connection between psoriasis and comorbidity is complex, because several factors are intertwined, such as genetic, immunological, and chronic inflammatory conditions (28), and they should not be neglected.
Although no statistically significant association was found between the duration of psoriasis and the occurrence of associated diseases in this study, the frequency of associated diseases obliges, in addition to the treatment of skin changes, the prevention, detection and treatment of associated diseases. Because in this study, 63,64% or 56 subjects or almost 2/3 had comorbidity, 40,91% or more than one third had one associated disease, and almost one third had obesity, more precisely 30,68% or 27 respondents. Associated rashes are an additional burden for the patient in several ways: they complicate treatment, economic burden, reduce work capacity and productivity, quality of life, but change the picture of psoriasis from skin to systemic disease.
It is important to understand the characteristics of patients with psoriasis, given the high prevalence of psoriasis, and comorbidities in patients, so that treatment and prevention are as effective as possible. In addition, detecting risk factors for comorbidities in psoriasis is certainly important for everyday practice can provide guidelines for screening patients.
6. CONCLUSION
Comorbidities occur in men with psoriasis, and their occurrence is not related to the duration of the disease. Detection and treatment of these diseases should be part of a comprehensive treatment of psoriasis, and it is certainly important to identify risk factors for comorbidities.
Graph 1. Percentage of associated diseases.
Graph 2. Relationship between psoriasis duration and obesity.
Graph 3. Relationship between psoriasis duration and high blood pressure.
Graph 4. Relationship between the duration of psoriasis and dyslipidemia.
Graph 5. Relationship between the duration of psoriasis and diabetes.
Author's contribution:
All authors were involved in all steps of preparation this article. Final proofreading was made by the first author.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Serrano L, Maloney V, Gordon KB. Risankizumab in Moderate-To-Severe Plaque Psoriasis. Immunotherapy. 2019 Nov;11(16):1357–1370. doi: 10.2217/imt-2019-0116. [DOI] [PubMed] [Google Scholar]
- 2.Armstrong AW, Harskamp CT, Armstrong EJ. The association between psoriasis and obesity: a systematic review and meta-analysis of observational studies. Nutr Diabetes. 2012 Dec;2(12):e54. doi: 10.1038/nutd.2012.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Love TJ, Qureshi AA, Karlson EW, Gelfand JM, Choi HK. Prevalence of the metabolic syndrome in psoriasis: results from the National Health and Nutrition Examination Survey, 2003-2006. Arch Dermatol. 2011 Apr;47(4):419–424. doi: 10.1001/archdermatol.2010.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ahlehoff O, Skov L, Gislason G, Lindhardsen J, Kristensen SL, Iversen L, et al. Pharmacological undertreatment of coronary risk factors in patients with psoriasis: observational study of the Danish nationwide registries. PLoS One. 2012;7(4):e36342. doi: 10.1371/journal.pone.0036342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khalid U, Hansen PR, Gislason GH. Psoriasis and New-Onset Diabetes Mellitus: A Danish nationwide cohort study. Diabetes Care. 2013 Aug;36(8):2402–2407. doi: 10.2337/dc12-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nijsten T, Wakke M. Complexity of the Association Between Psoriasis and Comorbidities. J Invest Dermatol. 2009 Jul;129(7):1601–1603. doi: 10.1038/jid.2009.55. [DOI] [PubMed] [Google Scholar]
- 7.Benhadou F, Mintoff D, Del Marmol V. Psoriasis: Keratinocytes or Immune Cells–Which Is the Trigger? Dermatology. 2019;235(2):91–100. doi: 10.1159/000495291. [DOI] [PubMed] [Google Scholar]
- 8.Link BG, Phelan JC. Conceptualizing stigma Annu Rev Soc. 2001 Aug;27(1):363–385. [Google Scholar]
- 9.Boehncke WH. Systemic Inflammation and Cardiovascular Comorbidity in Psoriasis Patients: Causes and Consequences. Front Immunol. 2018 Apr;9:579. [Google Scholar]
- 10.Li WQ, Han JL, Manson JE, Rim EB, Rexrode KM, Curhan GC, Qureshi AA. Psoriasis and risk of nonfatal cardiovascular disease in U.S. women: a cohort study. Br J Dermatol. 2012 Apr;166(4):811–818. doi: 10.1111/j.1365-2133.2011.10774.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madanagobalane S, Anandan S. Prevalence of metabolic syndrome in South Indian patients with psoriasis vulgaris and the relation between disease severity and metabolic syndrome: a hospital-based case-control study. Indian J Dermatol. 2012 Sep;57(5):353–357. doi: 10.4103/0019-5154.100474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khunger N, Gupta D, Ramesh V. Is psoriasis a new cutaneous marker for metabolic syndrome? A study in Indian patients. Indian J Dermatol. 2013 Jul;58(4):313–314. doi: 10.4103/0019-5154.113958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carrascosa JM, Vilavella M, Garcia-Doval I, Carretero G, Vanaclocha F, Daudén E, et al. Body mass index in patients with moderate-to-severe psoriasis in Spain and its impact as an independent risk factor for therapy withdrawal: results of the Biobadaderm Registry. J Eur Acad Dermatol Venereol. 2014 Jul;28(7):907–914. doi: 10.1111/jdv.12208. [DOI] [PubMed] [Google Scholar]
- 14.Li W, Han J, Hu FB, Curhan GC, Qureshi AA. Psoriasis and risk of type 2 diabetes among women and men in the United States: a population-based cohort study. J Invest Dermatol. 2012 Feb;132(2):291–298. doi: 10.1038/jid.2011.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Azfar R, Gelfand J. Psoriasis and metabolic disease: epidemiology and pathophysiology. Curr Opin Rheumatol. 2008 Jul;20(4):416–422. doi: 10.1097/BOR.0b013e3283031c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosa DJ, Machado RF, Matias FA, Cedrim SD, Noronha FL, Gaburri D, et al. Influence of severity of the cutaneous manifestations and age on the prevalence of several cardiovascular risk factors in patients with psoriasis. Eur Acad Dermatol Venereol. 2012 Mar;26(3):348–353. doi: 10.1111/j.1468-3083.2011.04076.x. [DOI] [PubMed] [Google Scholar]
- 17.Jacobi A, Kupke C, Behzad M, Hertl M. Comorbidities, metabolic risk profile and health-related quality of life in German patients with plaque-type psoriasis: a cross-sectional prospective study. Int J Dermatol. 2013 Sep;52(9):1081–1087. doi: 10.1111/j.1365-4632.2012.05517.x. [DOI] [PubMed] [Google Scholar]
- 18.Wu CY, Hu HY, Li CP, Chou YJ, Chang YT. Comorbidity profiles of psoriasis in Taiwan: A latent class analysis. PLoS One. 2018 Feb;13(2):e0192537. doi: 10.1371/journal.pone.0192537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hägg D, Sundström A, Eriksson M, Schmitt-Egenolf M. Severity of Psoriasis Differs Between Men and Women: A Study of the Clinical Outcome Measure Psoriasis Area and Severity Index (PASI) in 5438 Swedish Register Patients. Am J Clin Dermatol. 2017 Aug;18(4):583–590. doi: 10.1007/s40257-017-0274-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naito R, Imafuku S. Distinguishing features of body mass index and psoriasis in men and women in Japan: A hospital-based case-control study. J Dermatol. 2016 Dec;43(12):1406–1411. doi: 10.1111/1346-8138.13439. [DOI] [PubMed] [Google Scholar]
- 21.Chan WMM, Yew YW, Theng TSC, Liew CF, Oon HH. Prevalence of metabolic syndrome in patients with psoriasis: a cross-sectional study in Singapore. Singapore Med J. 2020 Apr;61(4):194–199. doi: 10.11622/smedj.2019152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miao C, Li J, Li Y, Zhang X. Obesity and dyslipidemia in patients with psoriasis: A case-control study. Medicine (Baltimore) 2019 Aug;98(31):e16323. doi: 10.1097/MD.0000000000016323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ma C, Harskamp CT, Armstrong EJ, Armstrong AW. The association between psoriasis and dyslipidaemia: a systematic review. Br J Dermatol. 2013 Mar;168(3):486–495. doi: 10.1111/bjd.12101. [DOI] [PubMed] [Google Scholar]
- 24.Takahashi H, Iizuka H. Psoriasis and metabolic syndrome. J Dermatol. 2012 Mar;39(3):212–218. doi: 10.1111/j.1346-8138.2011.01408.x. [DOI] [PubMed] [Google Scholar]
- 25.Gyldenløve M, Jensen P, Linneberg A, Thyssen JP, Zachariae C, Hansen PR, et al. Psoriasis and the Framingham risk score in a Danish hospital cohort. Int J Dermatol. 2014 Sep;53(9):1086–1090. doi: 10.1111/ijd.12196. [DOI] [PubMed] [Google Scholar]
- 26.Mazlin MB, Chang CC, Baba R. Comorbidities associated with psoriasis - data from the malaysian psoriasis registry. Med J Malaysia. 2012 Oct;67(5):518–521. [PubMed] [Google Scholar]
- 27.Santos M, Fonseca MH, Jalkh PH, Gomes GP, de Souza Cavalcante A. Obesity and Dyslipidemia in Patients With Psoriasis Treated at a Dermatologic Clinic in Manaus. An Bras Dermatol. 2013 Nov-Dec;88(6):913–916. doi: 10.1590/abd1806-4841.20132090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xu X, Zhang HY. The Immunogenetics of Psoriasis and Implications for Drug Repositioning. Int J Mol Sci. 2017 Dec;18(12):2650. doi: 10.3390/ijms18122650. [DOI] [PMC free article] [PubMed] [Google Scholar]


