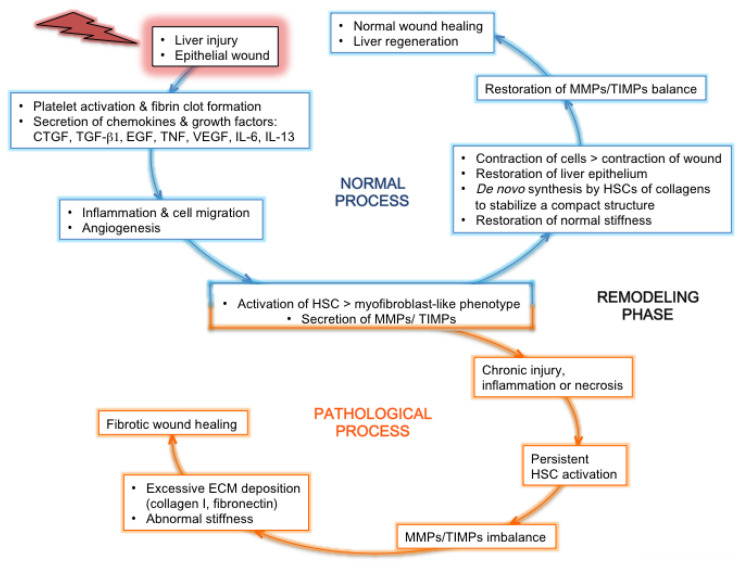
Figure 2.
Normal or pathological process after liver injury: tissue regeneration or fibrosis. After the initial event of liver injury, the epithelial wound accompanied by a breach in the endothelium triggers the coagulation cascade, followed by an inflammatory and proliferation phase mediated by the secretion of inflammatory cytokines and growth factors. The profibrotic cytokines IL-13 and TGF-β1 are secreted by activated leukocytes coming from the blood circulation and by sinusoidal cells [36]. Concomitantly, HSCs are activated, thereby adopting a myofibroblast-like phenotype and secreting MMPs and TIMPs. These proteins contribute to ECM remodeling, together with cytokines and chemokines that recruit leukocytes at the site of injury and activate them. In the loop of a normal wound-healing process (blue), the inflammatory process gives way to a progressive tissue repair, with the cleaning up of tissue debris and dead cells by leukocytes, the contraction of epithelial cells to restore a normal epithelium, and the de novo synthesis by HSCs of ECM components that organize in order to stabilize a compact structure between and around cells. This helps to restore normal stiffness. In parallel, endothelial cells form new blood vessels. The balance of secretion and activity between MMPs and TIMPs is restored to normal. All these features lead to normal wound healing and liver regeneration. In the loop of a pathological/fibrotic wound-healing process (orange), a state of chronic injury and inflammation is maintained, accompanied by tissue necrosis instead of repair. This leads to the persistent activation of HSCs. Thereby, the tight balance between MMPs and TIMPs secretion and activity is disrupted, and overly abundant amounts of ECM components produced by activated HSCs are deposited in the interstitial tissue, which becomes scar tissue with abnormal stiffness. Within this stiffer tissue, the migration of cells and chemokines that could contribute to healing is greatly impaired. Altogether, these features contribute to a fibrotic wound-healing phenotype, with the formation of a permanent fibrotic scar.