Abstract
In this era of the COVID-19 pandemic, patients with diabetes mellitus are at an increased risk of secondary infections and systemic complications. Here we are reporting 2 cases in post-covid-19 patients, who were uncontrolled type 2 diabetics and diagnosed with fungal osteomyelitis and mucormycosis respectively. Both patients were treated surgically immediately.
Keywords: Osteomyelitis, Mucormycosis, Diabetics, COVID 19
Introduction
Diabetes mellitus (DM) is one of the major causes of morbidity at the global level, becoming one of the risk factors for certain infectious diseases owing to the development of an immunocompromised state, the main culprit being hyperglycemia, affecting overall defence mechanisms of the body via various pathways.
The major oral and maxillofacial complications of diabetes include periodontal pathologies, salivary and taste dysfunction, neurosensory oral disorders, infections like bacterial, fungal infections leading to serious complications like rhino cerebral mucormycosis, synergistic necrotizing cellulitis, osteomyelitis of the jaws [1].
Mucormycosis is an uncommon, acute fungal disease, caused by the genera Mucor, Rhizopus, and Absidia. It occurs in the head and neck region, respiratory system, CNS, GIT, etc. Rhinocerebral mucormycosis is the type that involves the head and neck region. It occurs predominantly in dehydrated and acidotic patients, like patients with poorly controlled diabetics, patients with leukemia, etc. [2]. The nose is the most common site of initiation extending to paranasal sinuses, orbit, and cranial cavity. Odontalgia and extraction of maxillary teeth have been associated with the onset of symptoms. [2].
Osteomyelitis is an inflammatory condition involving the bone that usually initiates from the medullary cavity, rapidly involving the Haversian systems, and extending to the periosteum of the area [2]. The pus developed from the infection compromises the blood supply beneath the periosteum, leading to ischemia which in turn becomes necrotic. The frequency of occurrence of maxillary osteomyelitis is less owing to the extensive blood supply, presence of thin cortical plates, and scantiness of medullary tissues impeding the limitation of infections within the bone. The involvement of fungus in the bone marrow renders the fungal organisms’ growth, affecting the endothelial lining of vessels causing vascular insufficiency eventually leading to necrosis of the bone developing into fungal osteomyelitis. Fungal osteomyelitis offers high diagnostic difficulty and is more aggressive.
The current global health issue, coronavirus disease (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) and has become an emergency per se. COVID-19 patients are predisposed to developing fungal infections during the course and also in later stages of this disease, especially severely ill ones, due to a decrease of CD4 + T cells and CD8 + T cells leading to immune suppression. So the main objective of this case report is to document cases of oral and maxillofacial pathologies which are associated with COVID-19 infection.
Case Reports
Case Report 1: 34-year-old male patient reported to our hospital with a complaint of continuous pain and swelling over the right side of the midface since 2 months. The patient gave a past medical history for the same complaint. He was diagnosed with COVID-19 and was symptomatically treated for the same meanwhile developed pain over the first quadrant teeth and swelling with the same area. He was diagnosed in a local hospital with acute right maxillary sinusitis by the Department of ENT and it did not resolve after the antibiotic course. Later he was referred to a faciomaxillary surgeon and was advised for a CBCT of the maxilla. It revealed aggressive osteolytic lesions with respect to the right maxilla. So a biopsy was done, curettage and saucerization was performed, and the sample was sent for histopathological examination which in turn confirmed as fungal osteomyelitis. History of paresthesia was present in the same region. Then the patient came to our hospital with no relief of pain and also the radiation of pain towards the zygoma region of the right side. The patient was also a known case of Hypertension and type 2 Diabetes Mellitus and was under medication for the same. On extraoral examination gross facial asymmetry was noted with swelling extending from the infraorbital rim till zygomatic bone anteroposteriorly and medial canthus of the eye till the alar base of the nose of the right side. The swelling was firm, tender on palpation, non-erythematous, non-fluctuant, and was devoid of any surface change. The reduction in the mouth opening was noticed. Intraoral examination revealed a large defect involving the first quadrant, with no active pus discharge. Medically the treatment was started by administering insulin and iv liposomal Amphotericin B 5 mg/kg/day. Surgical resection via Weber Ferguson approach according to the involvement of midface bone as shown in the CT scan (Fig. 1) was done. Later antifungal drug was changed to oral Itraconazole 200 mg. 2 months post-discharge patient has not shown any signs of re-infection.
Fig. 1.
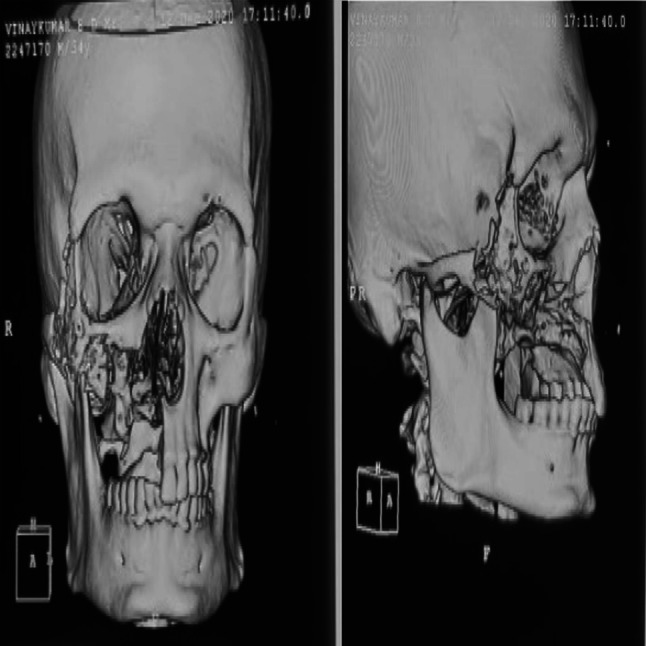
3D CT of patient mentioned in the first case report, diagnosed with fungal osteomyelitis of right maxilla and zygoma
Case Report 2: 50-year-old male patient reported to our hospital with a complaint of swelling over the right side of the midface since 2 months. His history included swelling of the same region with pus discharge treated by extraction of all teeth of the upper right quadrant with grade III mobility following an antibiotic course 2 months before. Despite the treatment, the swelling did not reduce. The patient is a known case of uncontrolled type 2 Diabetes Mellitus. Initial examination showed a firm, non-tender, non-erythematous, non-fluctuant swelling in the right malar region with no evidence of any drainage. Intraoral examination revealed a necrotic alveolar region in the right posterior maxillary region and swelling involving the hard palate. A biopsy was performed. Histopathological examination revealed thick-walled aseptate fungal hyphae with right-angled branching in P.A.S. stain and we diagnosed it as mucormycosis of the right maxilla. Medically the treatment was started by administering insulin and intrevenous liposomal Amphotericin B 250 mg. Surgical resection via Weber Ferguson approach according to the involvement of midface bone as shown in the CT scan (Fig. 2) was done. Post surgically antifungal drug was changed to oral Posaconazole 300 mg. 2 months post-discharge patient has not shown any signs of re-infection.
Fig. 2.
3D CT of patient mentioned in the second case report diagnosed with mucormycosis of right maxilla and zygoma
Discussion
These case reports were transcribed in the view of documenting cases of oral and maxillofacial pathologies in association with COVID-19 infection. In COVID-19, infected lung epithelial cells produce IL-8 and IL-6. IL-8 is a chemoattractant for neutrophils and T cells. Infiltration of inflammatory cells in a massive amount owing to lymphopenia was observed in the lungs of severe COVID-19 patients. In severe cases, thrombosis and pulmonary embolism were other prominent symptoms along with respiratory distress. These patients also showed elevated d-dimer and fibrinogen levels. The function of the endothelium includes the promotion of vasodilation, fibrinolysis, and anti-aggregation. COVID-19 patient’s hypercoagulable profiles indicate a significant endothelial injury. This will increase microvascular permeability facilitating bacterial invasion [3]. Chinese studies have found a high percentage of secondary infections (8–15%) in COVID-19 patients, including bacterial or fungal infections, and Chen et al. concluded in their study on 99 COVID-19 patients that only 5% cases developed fungal infections [4].
Patients with uncontrolled Diabetes Mellitus are immunocompromised due to ill effects of a hyperglycemic environment along with immune dysfunction such as damage to the function of neutrophils, weakening of antioxidant system, and humoral immunity [5]. Germination and invasive growth of acquired fungal spores are facilitated by high glucose levels, excess levels of ketone bodies, low pH environment, reduced oxygen, and high iron levels. Hyperglycaemia causes excessive glycosylation of transferrin and ferritin with a subsequent decrease in the iron-binding affinity of these proteins. Rhizoferrin produced by fungal hyphae forms iron-rhizoferin complexes after binding to serum iron which is required for the growth, development, and multiplication of fungal spores [6]. Vascular invasion of the vegetative forms into vessels forms thrombus within, causing ischemic infarcts sequentially causing necrosis of adjacent tissues.
The pathophysiology of diabetes mellitus and the host response to SARS-CoV-2 have similarities that might be adding up to the situation and resulting in an increased incidence of such pathologies of the jaw. With very little information on this correlation, it is difficult to avowal whether patients after getting infected by COVID-19 have a significant contribution towards the development of these pathologies. More literature on such conditions and larger multicentric studies will provide us with a better understanding of the pathophysiology of these conditions in post-COVID-19 infection patients.
Declarations
Conflict of interests
Authors declare that they don’t have any conflict of interest.
Ethical Approval
The manuscript has been read and approved by all the authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work.
Research Involving Human Participants and/or Animals
Study involves Human participants from Out Patient Department of Oral and Maxillofacial Surgery.
Informed Consent
The authors confirm that informed consent from the patients and their attenders was taken before their inclusion.
Consent to Participate
The authors confirm that informed consent from the patients and their attenders was taken before their inclusion.
Consent for Publication
Informed consent for publication from the participants was obtained.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
D. Sai Krishna, Email: degalasaikrishna@gmail.com
Harsha Raj, Email: harsharajbs@gmail.com.
Pranav Kurup, Email: k.pranav95maxfax@gmail.com.
Mehak Juneja, Email: mehakjuneja07@gmail.com.
References
- 1.Pathology M, Pathology M, Pathology M, Pathology M (2016) Research article prevalence of fungal osteomyelitis of the jaws associated with diabetes mellitus in north Karnataka population: a retrospective study *, 1 KochliChannappa Niranjan, 2 Niharika Sarathy, 3 Devendra Alrani and 4 Kaveri Hallikeri Professor
- 2.Topazian RG, Goldberg MH, Hupp JR. Oral and maxillofacial infections. 4. Philadelphia: W.B. Saunders; 2002. [Google Scholar]
- 3.Yuki K, Fujiogi M, Koutsogiannaki S (2020) COVID-19 pathophysiology: a review. Clin Immunol 2015(April) [DOI] [PMC free article] [PubMed]
- 4.Song G, Liang G, Liu W. Fungal co-infections associated with global COVID-19 pandemic: a clinical and diagnostic perspective from China. Mycopathologia [Internet] 2020;185(4):599–606. doi: 10.1007/s11046-020-00462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akash MSH, Rehman K, Fiayyaz F, Sabir S, Khurshid M. Diabetes-associated infections: development of antimicrobial resistance and possible treatment strategies. Arch Microbiol [Internet] 2020;202(5):953–965. doi: 10.1007/s00203-020-01818-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khandelwal P, Saluja H, Shah S, Dadhich A, Hajira N (2020) Diabetic maxillary osteomyelitis: a worrisome vulnerability—our experience. J Maxillofac Oral Surg [Internet]. 10.1007/s12663-020-01371-6 [DOI] [PMC free article] [PubMed]



