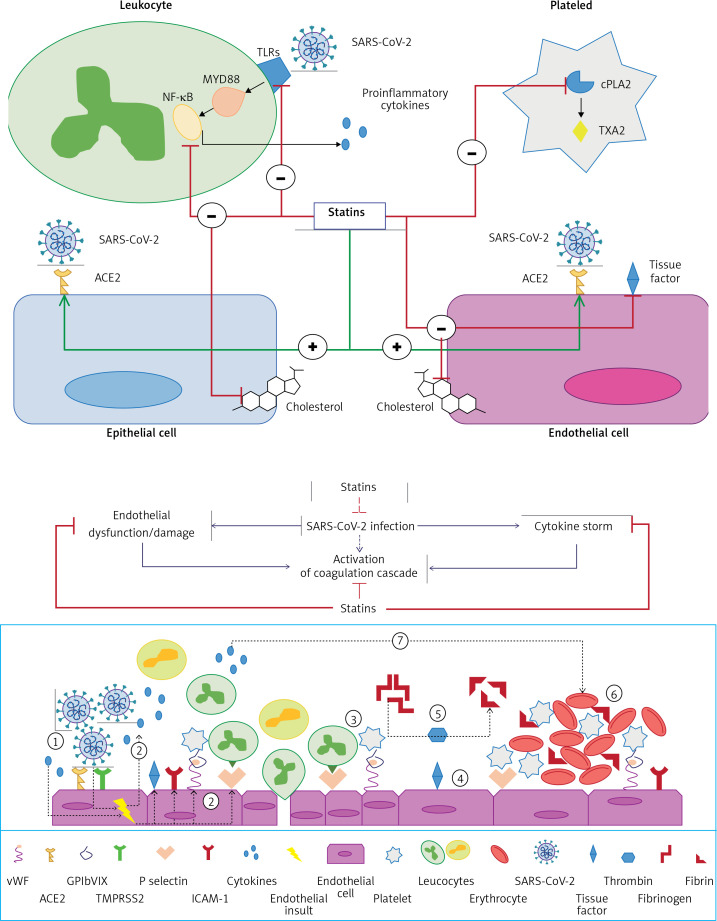
Figure 5.
(Upper figure) Proposed mechanisms for the beneficial effects of statins in SARS-CoV-2 infection. Cellular pathways altered by statins during the course of infection in COVID-19 patients. Surface expression of ACE2 in epithelial and endothelial cells is enhanced by statins. Statins also mitigate the MYD88–NF-κB pathway and the ensuing proinflammatory cytokine response following interaction of SARS-CoV-2 with toll-like receptors (TLRs). The anti-thrombotic effects of statins are mediated by suppressive effects on tissue factor, and cytosolic phospholipase A2 (cPLA2)-induced thromboxane A2 (TXA2) synthesis and inactivated endothelial cells and platelets, respectively. Statins have also been suggested to decrease plasma membrane cholesterol content in the host cells, which can interfere with the replication of virus particles. (Lower figure) Proposed mechanisms for the anti-thrombotic effects of statins in SARS-CoV-2 infection SARS-CoV-2 induces activation of endothelial cells and the release of pro-inflammatory cytokines, which can lead to:1) over-expression of adhesion molecules (e.g. P-selectins, intercellular adhesion molecule 1 (ICAM-1), von Willebrand factor, αvβ3) and further release of proinflammatory cytokines; 2) increased recruitment of leukocytes and platelets; 3) activated endothelial cells also express tissue factor, which activates factor VII, factor Xa, and thrombin formation; 4) fibrinogen is cleaved into fibrin by thrombin; 5) thrombin is essential for thrombus formation; 6)pro-inflammatory factors can also promote coagulation and accelerate platelet activation and thrombus formation; and 7)statins downregulate proinflammatory cytokine release from endothelial cells and mitigate coagulation cascade. Moreover, statins interfere with SARS-CoV-2 entry intoACE2- expressing endothelial cells and ensuing endothelial activation (reproduced with permission from [18])