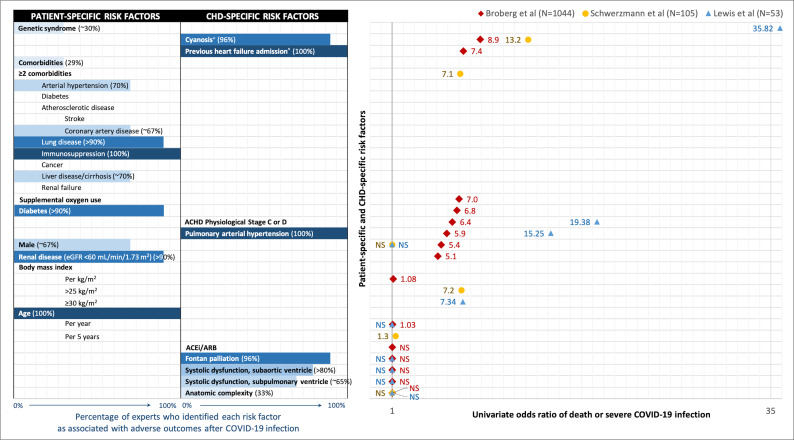
Figure 1.
Comparison of expert opinion vs real-world data on independent predictors of death or severe COVID-19 infection in ACHD patients. Patient-specific and CHD-specific risk factors assessed by Ruperti-Repilado et al, Broberg et al, Schwerzmann et al and Lewis et al are presented in two columns on the left. Blue horizontal bars indicate the percentage (%) of surveyed experts who perceived each risk factor to be associated with adverse outcomes after COVID-19 infection.3 Risk factors are listed by decreasing magnitude of OR from univariate analysis from Broberg et al (red diamond), Schwerzmann et al (yellow circle) and Lewis et al (blue triangle). ORs are plotted on the right from 1 (not statistically significant, NS) to 36. Overall, ACHD experts underestimated the importance of patient-specific risk factors, particularly that of body mass index, male sex and genetic syndrome. They overestimated the importance of CHD-specific risk factors such as anatomical complexity and Fontan palliation, and correctly identified the importance of cyanosis, pulmonary arterial hypertension or Eisenmenger syndrome and clinical heart failure. ACE inhibitor (ACEi) or angiotensin receptor blocker (ARB) use were not associated with adverse outcomes after COVID-19 infection. ˆIncluded as ‘symptomatic heart failure’ in Ruperti-Repilado et al’s survey. +Defined as: oxygen saturation<90% in Broberg et al; cyanotic heart disease or Eisenmenger syndrome in Schwerzmann et al. ACHD, adults with congenital heart disease. CHD, congenital heart disease.