Abstract
Friedreich ataxia (FRDA) is a recessive disorder resulting from relative deficiency of the mitochondrial protein frataxin. Frataxin functions in the process of iron–sulfur (Fe–S) cluster synthesis. In this review, we update some of the processes downstream of frataxin deficiency that may mediate the pathophysiology. Based on cellular models, in vivo models and observations of patients, ferroptosis may play a major role in the pathogenesis of FRDA along with depletion of antioxidant reserves and abnormalities of mitochondrial biogenesis. Ongoing clinical trials with ferroptosis inhibitors and nuclear factor erythroid 2-related factor 2 (Nrf2) activators are now targeting each of the processes. In addition, better understanding of the mitochondrial events in FRDA may allow the development of improved imaging methodology for assessing the disorder. Though not technologically feasible at present, metabolic imaging approaches may provide a direct methodology to understand the mitochondrial changes occurring in FRDA and provide a methodology to monitor upcoming trials of frataxin restoration.
Keywords: biomarkers, clinical trial, mitochondrial biogenesis
Background
Friedreich Ataxia (FRDA) is a recessive disorder beginning in childhood or juvenile years that causes progressive ataxia, dysarthria, loss of sensation, and loss of coordination [1–3]. In some individuals it also leads to cardiomyopathy, scoliosis, diabetes, sensorineural hearing loss, and optic neuropathy. FRDA is caused by biallelic mutations in the FXN gene, which codes for the small mitochondrially targeted protein frataxin [4–6]. The most common mutation in FRDA is an expansion of a naturally occurring guanine-adenine-adenine (GAA) repeat in intron 1 (96%) that decreases but does not totally eliminate transcription of FXN mRNA. Approx. 4% of individuals have point mutations or deletions [7–9]. All forms of FXN mutations decrease the levels of functional frataxin, making FRDA primarily a disease of frataxin deficiency with all disease manifestations reflecting dysfunction downstream of frataxin loss.
Frataxin carries a mitochondrial targeting sequence, and its relative absence leads to dysfunction of multiple mitochondrial processes. The primary function of frataxin appears to be in synthesis of iron–sulfur (Fe–S) clusters in the mitochondria, and facilitating their introduction to enzymes containing this prosthetic group [10–12]. Classically, such enzymes include many of the enzymes of oxidative phosphorylation and the Krebs cycle, but many other enzymes also utilize Fe–S clusters [13]. The partial loss of frataxin in FRDA leads to deficient activity of such enzymes including aconitase, complex I and complex II [14–16], decreasing adenosine triphosphate (ATP) production and producing downstream dysfunction in mitochondrial activity and reactive oxygen species (ROS) production [17–19].
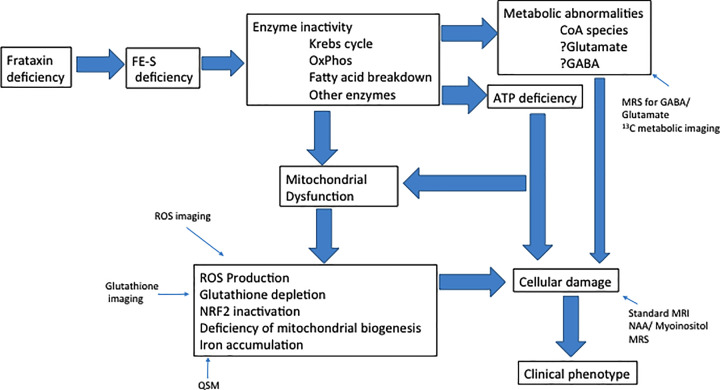
While initial characterization of mitochondrial dysfunction in FRDA concentrated on ROS production, other specific secondary processes likely mediate large components of the FRDA pathophysiology. These include iron accumulation and ferroptosis, depletion of endogenous antioxidant systems such as those controlled by nuclear factor erythroid 2-related factor 2 (Nrf2), and deficient mitochondrial biogenesis [20–23]. Along with primary enzymatic deficiency from Fe–S cluster deficiency, these collectively alter metabolism in many systems in FRDA, including iron metabolism, glutathione synthesis, and lipid metabolism. Such mechanisms have been reviewed here previously [20] (Figure 1). In the present work, we concentrate on new variations on these topics as well as further developments linking such mechanisms to clinical therapeutics and clinical monitoring.
Figure 1. Schematic pathophysiology of FRDA.
Possible sites of imaging are also included.
Iron-mediated pathophysiology
Conceptually, FRDA is a disorder of iron distribution rather than simply overload. Iron accumulates in the mitochondria in FRDA and animal models based on frataxin deficiency, although the cytoplasm is iron deficient in FRDA, and patients systemically behave as if they are iron depleted [24–26]. In early models, mitochondrial iron accumulation was proposed as a direct contributor to ROS production through Fenton chemistry. Such a direct but simple role for iron accumulation in FRDA has largely been dismissed based on three types of observations. First, iron accumulation is not consistent across FRDA models or in brain regions in which the pathology of FRDA is most significant [27,28]. Second, direct demonstration of ROS production in patients with FRDA has proven difficult in humans [29]. Finally, direct iron chelation has not proven successful, though there is some evidence for selective effects of deferiprone in heart [30]. Deferiprone, a targeted iron chelating agent, improved cardiac hypertrophy in a modest size study but had no effects on neurological function. Overall, such results require a refinement of the role of iron in the pathophysiological mechanisms in FRDA to address the emerging concept of ferroptosis.
Ferroptosis is initiated by inhibition of the enzyme, glutathione peroxidase-4 (GPX4) in conjunction with lipid peroxidation and iron accumulation [,31–34]. It is distinct from classical apoptosis, involving no nuclear involution but mitochondrial morphologic changes instead. Inducers of ferroptosis include agents that deplete glutathione, and those that inhibit or destroy GPX4. Iron accumulation is crucial in ferroptosis through promotion of lipid peroxidation. Thus, two of the known promoters of ferroptosis (iron overload, glutathione depletion) create a predisposition to this mechanism in FRDA. In fibroblasts from FRDA patients, cell death occurs in response to erastin, which initiates ferroptosis by blocking the glutamate-cysteine antiporter and thus inhibiting glutathione synthesis. Ferroptosis inhibitors block such cell death in FRDA fibroblasts whereas caspase 3 inhibitors (which block apoptosis but not ferroptosis) have no effect. Such results identify ferroptosis as a major cell death mechanism in FRDA models.
It also provides a novel direction for FRDA-related drug development. As lipid peroxidation plays a crucial role in ferroptosis, introduction of distinct membrane-destined lipids less susceptible to peroxidation could ameliorate this process. Oleic acid has been suggested to be less amenable to peroxidation, and a novel stereoselective oleic acid derivative decreases ferroptosis in FRDA fibroblasts [,35]. In addition, lipophilic phenothiazine agents also have antiferroptotic activity in FRDA-derived cells, identifying a different class of agents for treatment of FRDA [,36] (Table 1).
Table 1. Novel mitochondrially targeted agents for FRDA.
| Agent | Mechanism | Status | References |
|---|---|---|---|
| Oleic acid derivative | Ferroptosis inhibitor | Preclinical | [,35] |
| Novel lipophilic phenothiazines | Ferroptosis inhibitor | Preclinical | [,36] |
| RT-001 | Ferroptosis inhibitor | Pivotal trial | [,37,38] |
| PTC 743 | Ferroptosis inhibitor | Pivotal trial | [,39] |
| Omaveloxolone | Nrf2 activator | Pivotal trial | [50,52,53] |
| Letiriglitozone | PPARgamma activator | Preclinical | [68] |
| Elamipretide | Cardioplipin facilitator | Early trials | [69–73] |
Agents discovered before the understanding of ferroptosis also may have antiferroptotic activity in FRDA. One approach is to lower the intrinsic susceptibility to lipid peroxidation by replacement of hydrogen with deuterium in lipid side chains of membrane lipids [,37,38]. The commercial agent RT001, 11,11-D2-ethyl linoleate, blocks FRDA-mediated cell death in the BSO-iron model, consistent with an inhibition of ferroptosis. In a phase I/II clinical trial, the agent was well tolerated, and subjects improved peak workload during a maximal exercise. It is presently in a phase III trial with results expected in late 2021.
In addition, a second agent linked to ferroptosis, vatiquinone (α-tocotrienol quinone, EPI 743, PTC 743) has entered clinical trials in FRDA [39]. This agent inhibits 15 lipoxygenase and blocks ferroptosis in FRDA cells in vitro. In a moderate-size clinical trial in adults with FRDA, it failed to reach its primary endpoint in the 6-month double-blind portin. However, subjects who remained on agent for 2 years progressed less than matched individuals from natural history data. Consequently, it is presently in a phase III trial in less progressed individuals with FRDA and being evaluated for a longer duration.
Nrf2 and endogenous antioxidant defenses
Many lines of evidence demonstrate the depletion of endogenous antioxidants in FRDA. Superoxide dismutase (SOD) levels are decreased in FRDA models and fail to induce in response to frataxin knockdown, and multiple models of FRDA demonstrate altered homeostasis of the endogenous antioxidant glutathione [40,41]. Such protective mechanisms are controlled transcriptionally by the antioxidant response element (ARE) in DNA, and the transcription factor Nrf2. Nrf2 levels are abnormal and mislocalized in FRDA cells and tissue from many different FRDA models [42–47]. Nrf2 activation increases transcription of mRNA for endogenous antioxidant enzymes such as SOD, glutathione S-transferase (GST), and NADPH: quinone oxidoreductase (NQO1), making the dysfunction of Nrf2 in FRDA a therapeutic target in FRDA. Ubiquitination of Nrf2 controls its localization and turnover; the ubiquitin E3 ligase Keap 1 provides the primary mechanism mediating these events. ROS production during mitochondrial dysfunction can modify the sulfhydryl residues of Keap I, dissociating it from Nrf2 and allowing Nrf2 to enter the nucleus and activate ARE containing genes. However, to some degree Nrf2 activation is also controlled by other E3 ligases such as Hrd1, an E3 ligase associated with ER stress [48].
Nrf2 activation with several agents improves cell viability and mitochondrial function in cells from FRDA patients. Such agents include dimethylfumarate (DMF), omavaloxolone, and at lower potency sulforaphane. Each increases Nrf2 levels by binding to Keap1, but their properties in vivo and in vitro vary to some degree. This may reflect individual pharmacokinetic features of such agents, but they also may not have identical targets of action. For example, omavaloxolone not only increases Nrf2 levels but also inhibits nuclear factor κ B (NFK-B), and DMF also raises frataxin levels both in cell culture and in vivo. No such effect on frataxin level has been clearly shown for omavaloxolone [49,50]. Consequently, these distinct Nrf2 activators may have varying effects in clinical trials. Such agents also may block ferroptosis, thus demonstrating the overlapping nature of pathophysiological mechanisms downstream from frataxin deficiency [51].
Clinical trials with Nrf2 activators have shown initial success [50,52–54]. Two successive studies with omavaloxolone demonstrated benefit on the neurological exam-based marker of FRDA known as the mFARS, as well as biomarkers of Nrf2 activity such as ferritin and on FRDA-based abnormal metabolism. It also provided benefit on activities of daily living in some subgroups of patients. Perhaps most importantly, there was evidence for endurance of the effects of omavaloxolone. Benefit was not immediate but accrued over 6 months with persistence to 1 year, differentiating it from previous studies of antioxidants. In clinical trials of exogenous antioxidants, apparent benefit was almost immediate and began to wane within 6 months such that no sustained benefit could be identified [55–58]. This potentially differentiates the temporal effect of transcription factor-mediated control of endogenous antioxidants from the transient effect of exogenously administered compounds. Although not yet approved for treatment of FRDA, studies of omavaloxolone provide proof-of-concept for augmentation of the endogenous antioxidant response as a target in FRDA.
The Nrf2 pathway offers other targets for intervention [48,59]. These include the alternative ubiquitin ligase HRD1 as well as the downstream enzymes such as those controlling thioredoxin and glutaredoxin. Theoretically, each of these could act synergistically in control of antioxidant defenses with Keap1-mediated control of Nrf2 degradation. Interestingly, the ubiquitin ligase Hrd1 is most commonly associated with control of ER stress, a process implicated in some models of FRDA [60]. This could provide a pathologic feedback cycle in which loss of Nrf2 leads to ER stress, which leads to further loss of Nrf2 and a potentiation of the pathophysiology of FRDA.
Mitochondrial biogenesis
A second pathway downstream from mitochondrial dysfunction is the peroxisome proliferator-activated co-activator 1-α (PGC1α)/peroxisome proliferator-activated receptor-γ (PPARγ) pathway of mitochondrial biogenesis [61–65]. Frataxin deficiency leads to decreased levels of PGC1α in multiple models of FRDA, which, as reviewed previously, should then cause specific metabolic abnormalities and decreased mitochondrial biogenesis. Such metabolic abnormalities, including decreased levels of oxidative phosphorylation and fatty acid oxidation, and failure to renew mitochondria through their biogenesis could directly mediate the pathophysiology of FRDA [66]. Thus, this pathway represents a pharmacological target in FRDA.
Still, targeting PGC1α and its co-activator PPARγ has proven difficult. The results of a trial of pioglitazone, a PPARγ activator, have never been reported, but presumptively led to no benefit [67]. More recently, a related drug letiriglitazone has shown promise in animal and cellular models [68]. This brain penetrant, biologically active metabolite of pioglitazone, increases frataxin levels and ameliorates cell death in mouse dorsal root ganglion cell models of FRDA; it also improves altered motor function in one mouse FRDA model. Finally, it augments fatty acid B oxidation (independent of frataxin levels) and increases markers of mitochondrial biogenesis. It thus provides a possible therapeutic approach in FRDA by reversing the effects of PPARγ/PGC1α down-regulation.
The mitochondrial biogenesis pathway is not completely independent of the effects of Nrf2 as agents such as DMF have actions on both. This again suggests the possibility that multiple agents could act synergistically in augmenting downstream pathways that protect against frataxin deficiency. In addition, many agents that directly improve the mitochondrial response to frataxin deficiency (letiriglitazone, DMF) also increase frataxin levels secondarily. Another such agent is SS-31 (Elamipretide) [69–71]. This small peptide stabilizes cardiolipin in mitochondrial membranes and improves mitochondrial function. It also improves bioenergetics specifically in FRDA models and can raise frataxin levels in some situations [72–74]. This may reflect an indirect effect of cardiolipin on the level of frataxin [74].
Extra-mitochondrial frataxin
Since the identification of the mutation in FRDA, most conceptualizations have viewed FRDA as a variant upon mitochondrial disease. However, cytosolic frataxin may also be involved. Erythrocytes make a specific form of frataxin without a mitochondrial targeting sequence, derived from a specific splice variant [75]. In mice, cytosolic forms of frataxin appear in multiple tissues, though the mechanism of their origin is not clear [76]. At present, the function of cytosolic frataxin is unknown although it could aid is cytosolic Fe–S cluster syntheses. In addition, its role in the pathogenesis of FRDA is unclear [77].
Tracking FRDA with mitochondrial biomarkers and imaging
While mitochondrially targeted approaches may be important in therapy of FRDA, definitive therapy requires restoration of frataxin. Gene therapy, protein replacement and epigenetics-based reactivation of the FXN gene offer the best opportunities for sustained improvement across multiple tissues [1–3,78]. However, clinical trials of frataxin restoration require a method for confirming re-expression of frataxin in affected tissues such as heart, skeletal muscle, and brain. Most methods to measure frataxin are sufficiently invasive to be problematic in clinical trials, meaning that frataxin re-expression must be monitored by assessment of downstream processes. Imaging of mitochondrial pathophysiology in vivo thus becomes a crucial component of assessment of frataxin restoration.
Magnetic resonance imaging/spectroscopy background in FRDA
Magnetic resonance imaging/spectroscopy (MRI/MRS) provides non-invasive and inexpensive techniques to image not only brain anatomy, but also metabolic function [79]. In diseases like FRDA and other ataxias, MRI can clinically provide diagnostic information by observing structural changes in specific anatomic areas and allows for monitoring of the structural changes in brain and spinal cord that correlate with neurological decline [80]. Clinical MRI studies in patients with FRDA using 3T MRI scanners can assess gray matter integrity while such scanners also create diffusion tensor images that identify previously unsuspected abnormalities in white matter in FRDA [81–88]. MRS assessing myoinositol and n-actylaspartate (NAA) can quantify the pathological changes chemically, perhaps before axons cell bodies die. However, while highly quantitative, such structural imaging is not usually needed for diagnosis or management, and its utility as a biomarker is limited as it captures mainly the fixed features of neurodegeneration. Essentially, present methods monitor the later stages in the pathophysiology of the disease and may be useful in assessing response to therapies acting on this aspect of disease but cannot readily identify the earlier steps. In contrast, chemically based imaging approaches may be needed to monitor the early, biochemical events in FRDA, before structural damage appears. Such techniques also serve as pharmacodynamic markers that may detect response to frataxin restoration more rapidly than structural imaging. Imaging approaches that capture metabolic events immediately downstream from frataxin as well as methods to image secondary processes reflecting mitochondrial dysfunction could provide imaging approaches for following the course of frataxin restoration in FRDA.
Iron accumulation imaging techniques
Quantitative susceptibility mapping (QSM) uses MRS to quantify iron content in the brain [89], which could provide a useful biomarker in FRDA [90] through its potential link to iron accumulation [91]. Iron accumulation in the dentate nucleus correlates with clinical status and may improve in response to proposed therapy [91]. However, atrophy may precede iron accumulation, suggesting that iron accumulation likely lies relatively far downstream from the primary genetic defect. Ideally, quantifying iron accumulation would be most beneficial in measuring the events leading to ferroptosis, but the present data suggest it reflects a more empiric marker of neuronal change without direct link to the early pathophysiology. QSM thus could track components of disease progression but may not monitor the earliest events following frataxin loss or restoration.
γ-Aminobutyric acid, glutamate, and Krebs cycle intermediates
In order to image markers closer to frataxin deficiency than accumulation of iron in FRDA, one could examine various metabolic abnormalities and enzymes altered by loss of frataxin-enhanced Fe–S cluster formation, such as Krebs cycle intermediates and compounds metabolically derived from the Krebs cycle. γ-Aminobutyric acid (GABA) and glutamate are synthesized from Krebs cycle intermediates to some degree and are key molecules in mediating metabolic dysfunction in the brain based on their role as neurotransmitters [92]. Their levels may reflect metabolic dysfunction in early FRDA based on synthetic differences, but in later disease levels of GABA and glutamate could reflect the progression of disease based on neuronal dropout. In particular, imaging these neurotransmitters could provide a method for identifying neuronal loss more selectively; for example, in FRDA, the neuronal loss in the dentate nucleus reflects loss of glutamatergic but not GABAergic cells [93]. Spectroscopic assessment GABA levels should reveal in increase over time as glutamatergic cells die. Both GABA and glutamate have been successfully imaged and quantified with 3T MRI scanners [94–96] but have not been reported in FRDA. Still, though both molecules could provide quantifiable markers of metabolic abnormalities in early disease, they are still several enzymatic steps removed from frataxin deficiency in the pathophysiology of FRDA [95–97]. Other metabolic alterations should also be proximal to cell damage or iron accumulation though such markers also may not identify the earliest features of frataxin restoration. However, even if the enzymes within the Krebs cycle could be measured, metabolism within the CNS involves complex shuttling of molecules between cells and could make exact interpretations very complex.
Glutathione and ROS imaging and measurement
Like many small molecules in the brain, glutathione production and regeneration are impacted by mitochondrial dysfunction. Glutathione has been successfully imaged and quantified using 3T MRS techniques, though images obtained at this field strength may lack the fidelity and accuracy for detecting small changes in clinical trials [85]. Along with the 3T imaging glutathione, 7T MRS imaging can also assess glutathione as well [98]. Ultra-high MRI uses 7T scanners that are primarily used for research on human subjects, but it has not been used regularly in clinical studies. 7T images can be heavily affected by the smallest movements; in some cases, subjects’ heartbeats could move the brain by under a millimeter, altering the results [98]. Its safety in children is also unknown. While research has been conducted using 7T imaging in FRDA adults in the past [99], the clinical features of ataxia (uncontrolled movement) might confound such studies. Still this type of imaging provides significant potential in being able to quantify glutathione and can create much clearer brain images and potentially more useful biomarkers for measurement in FRDA.
Quantifying and tracking the development of ROS could provide another potential biomarker for disease progression in FRDA, looking specifically at the decline of mitochondrial function (which should lead to an increase in ROS production). ROS have been quantified and measured using fluorescent probes both in vitro and in vivo [100,101]. While this technology and advancements in research techniques could prove useful in the future, they have not been used in humans or any clinical setting. Currently, no one technique satisfies all of the constraints required to constitute an ideal imaging technique for ROS in humans; however, a combination of anatomical and functional imaging techniques may allow this technology to develop clinical utility [102]. Much like the other biomarkers, this marker is substantially downstream from frataxin deficiency. However, this information could be valuable in clinical and research settings to measure mitochondrial dysfunction related to FRDA, as well as, provide a sensitive manner for answering the question of whether ROS production actually occurs in FRDA, an ongoing pathophysiological question [29].
ATP deficiency and imaging
ATP deficiency in FRDA results from inactivity of Fe–S containing enzymes and ultimately, frataxin deficiency. In cell culture, ATP levels provide a marker of cell viability as well, and both in cell culture and in FRDA patients ATP levels parallel disease features. Thus, the ability to measure and quantify ATP and the rate at which it changes in FRDA would provide a pharmacodynamic biomarker to track the progression of enzyme inactivity in the mitochondria, the overall pathophysiology, and the response to therapy. ATP levels can be measured in muscle (skeletal and cardiac) using 31-P nuclear magnetic resonance (NMR) or analogous approaches [17,103,104]. A number of techniques have been developed to image ATP in the brain using optical microscopy paired with probes [105,106], as well as some magnetic resonance techniques for in vivo studies [105]. Biosensors have been used in vivo and in yeast [107], but none of the techniques so far are ideal, preventing them from being used in human subjects. There have also been several non-imaging approaches to quantify ATP; however, these also have failed in humans and cannot provide content equivalent to imaging methods [105]. Unfortunately, the technology has not advanced enough to make measuring ATP in the brain a safe and efficient resource in FRDA at this time.
Metabolic function imaging
While ATP levels or synthesis cannot be imaged with current technology, metabolic labeling can examine other measurable markers such as reactants or products of the Krebs cycle. Pyruvate, lactate, and glutamate can be labeled in vivo by introducing heavy carbon (13C)-containing precursors into a subject, which can then be imaged using a 3T MRI scanner [108,109]. The 13C is then identified by MRI/MRS and separated into quantitative measures of the compounds into which it is metabolized, such as pyruvate, lactate, and glutamate [109]. By measuring the reactants and products of the metabolic process, overall and specific metabolic functions in the brain can be assessed in patients (such as those with FRDA) in comparison with controls. Metabolic dysfunction is a known consequence of frataxin deficiency thus potentially resulting in altered levels or flux of compounds such as GABA and glutamate [110]. Much like trying to image Krebs cycle intermediates, this technique is imperfect for a few reasons. Metabolism in the CNS involves many enzymes that are not directly tracked with this method, making it hard to draw exact interpretations of the effect of frataxin deficiency on metabolic function. This method is also more invasive (due to the need to introduce labeled substances) and expensive (the cost of the 13C compound) than a typical MRI [108,109].
Conclusions
The present review has extended previous discussions on the mitochondrial pathophysiology of FRDA and how it may be used therapeutically and in future monitoring of the disorder. These events are complex, seemingly involving many different mechanisms that eventually lead to a relatively selective neurological and systemic disease—a true metabolic disease from frataxin deficiency (Figure 1). By isolating these pathways, targeting them with therapeutic strategies, and assessing them in human in clinical trials, one can logically move toward successful therapy. Further understanding of such events, and technological imaging advances to monitor mitochondrial events in vivo may facilitate pharmaceutical advances. However, even this approach is overly simplistic. Each step or pathway in Figure 1 does not occur in isolation; there is substantial cross-talk between the pathways. In some cases, the interactions are cooperative, leading to pathological positive feedback cycles. In other cases, they are compensatory, as nominally abnormal events block the toxicity of other pathways. In still other interactions, observations are likely to be epiphenomena, representing markers but not causes of disease. This complexity emphasizes the need to understand both the early and late events of FRDA, such that therapeutic development can become successful.
Abbreviations
- ARE
antioxidant response element
- ATP
adenosine triphosphate
- BSO
buthionine sulfoximine
- DMF
dimethylfumarate
- Fe–S
iron–sulfur
- FRDA
Friedreich ataxia
- GABA
γ-aminobutyric acid
- GPX4
glutathione peroxidase-4
- MRI
magnetic resonance imaging
- MRS
magnetic resonance spectroscopy
- NFK-B
nuclear factor κ B
- NQO1, NADPH
quinone oxidoreductase
- Nrf2
nuclear factor erythroid 2-related factor 2
- PGC1α
peroxisome proliferator-activated co-activator 1-α
- PPARγ
peroxisome proliferator-activated receptor-γ
- QSM
quantitative susceptibility mapping
- ROS
reactive oxygen species
- SOD
superoxide dismutase
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
The authors declare that there are no sources of funding to be acknowledged.
References
- 1.Delatycki M.B. and Bidichandani S.I. (2019) Friedreich ataxia- pathogenesis and implications for therapies. Neurobiol. Dis. 132, 104606 10.1016/j.nbd.2019.104606 [DOI] [PubMed] [Google Scholar]
- 2.Tai G., Corben L.A., Yiu E.M., Milne S.C. and Delatycki M.B. (2018) Progress in the treatment of Friedreich ataxia. Neurol. Neurochir. Pol. 52, 129–139 10.1016/j.pjnns.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 3.Babady N.E., Carelle N., Wells R.D.et al. (2007) Advancements in the pathophysiology of Friedreich’s Ataxia and new prospects for treatments. Mol. Genet. Metab. 92, 23–35 10.1016/j.ymgme.2007.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Campuzano V., Montermini L., Moltò M.D.et al. (1996) Friedreich’s ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science 271, 1423–1427 10.1126/science.271.5254.1423 [DOI] [PubMed] [Google Scholar]
- 5.Dürr A., Cossee M., Agid Y.et al. (1996) Clinical and genetic abnormalities in patients with Friedreich’s ataxia. N. Engl. J. Med. 335, 1169–1175 10.1056/NEJM199610173351601 [DOI] [PubMed] [Google Scholar]
- 6.Rodden L.N., Chutake Y.K., Gilliam K.et al. (2021) Methylated and unmethylated epialleles support variegated epigenetic silencing in Friedreich ataxia. Hum. Mol. Genet. 29, 3818–3829 10.1093/hmg/ddaa267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCormack M.L., Guttmann R.P., Schumann M.et al. (2000) Frataxin point mutations in two patients with Friedreich’s ataxia and unusual clinical features. J. Neurol. Neurosurg. Psychiatry 68, 661–664 10.1136/jnnp.68.5.661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galea C.A., Huq A., Lockhart P.J.et al. (2016) Compound heterozygous FXN mutations and clinical outcome in friedreich ataxia. Ann. Neurol. 79, 485–495 10.1002/ana.24595 [DOI] [PubMed] [Google Scholar]
- 9.Cossée M., Dürr A., Schmitt M.et al. (1999) Friedreich’s ataxia: point mutations and clinical presentation of compound heterozygotes. Ann. Neurol. 45, 200–206 [DOI] [PubMed] [Google Scholar]
- 10.Tsai C.L. and Barondeau D.P. (2010) Human frataxin is an allosteric switch that activates the Fe-S cluster biosynthetic complex. Biochemistry 49, 9132–9139 10.1021/bi1013062 [DOI] [PubMed] [Google Scholar]
- 11.Schmucker S., Martelli A., Colin F.et al. (2011) Mammalian frataxin: an essential function for cellular viability through an interaction with a preformed ISCU/NFS1/ISD11 iron-sulfur assembly complex. PLoS ONE 6, e16199 10.1371/journal.pone.0016199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Colin F., Martelli A., Clemancey M.et al. (2013) Mammalian frataxin controls sulfur production and iron entry during de novo Fe4S4 cluster assembly. J. Am. Chem. Soc. 135, 733–740 10.1021/ja308736e [DOI] [PubMed] [Google Scholar]
- 13.Lill R. (2020) From the discovery to molecular understanding of cellular iron-sulfur protein biogenesis. Biol. Chem. 401, 855–876 10.1515/hsz-2020-0117 [DOI] [PubMed] [Google Scholar]
- 14.Rötig A., de Lonlay P., Chretien D.et al. (1997) Aconitase and mitochondrial iron-sulphur protein deficiency in Friedreich ataxia. Nat. Genet. 17, 215–217 10.1038/ng1097-215 [DOI] [PubMed] [Google Scholar]
- 15.Erb M., Hoffmann-Enger B., Deppe H.et al. (2012) Features of idebenone and related short-chain quinones that rescue ATP levels under conditions of impaired mitochondrial complex I. PLoS ONE 7, e36153 10.1371/journal.pone.0036153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bradley J.L., Blake J.C., Chamberlain S., Thomas P.K., Cooper J.M. and Schapira A.H. (2000) Clinical, biochemical and molecular genetic correlations in Friedreich’s ataxia. Hum. Mol. Genet. 9, 275–282 10.1093/hmg/9.2.275 [DOI] [PubMed] [Google Scholar]
- 17.DeBrosse C., Nanga R.P.R., Wilson N.et al. (2016) Muscle oxidative phosphorylation quantitation using creatine chemical exchange saturation transfer (CrCEST) MRI in mitochondrial disorders. JCI Insight 1, e88207 10.1172/jci.insight.88207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lodi R., Hart P.E., Rajagopalan B.et al. (2001) Antioxidant treatment improves in vivo cardiac and skeletal muscle bioenergetics in patients with Friedreich’s ataxia. Ann. Neurol. 49, 590–596 10.1002/ana.1001 [DOI] [PubMed] [Google Scholar]
- 19.Lodi R., Cooper J.M., Bradley J.L.et al. (1999) Deficit of in vivo mitochondrial ATP production in patients with Friedreich ataxia. Proc. Natl. Acad. Sci. U.S.A. 96, 11492–11495 10.1073/pnas.96.20.11492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark E., Johnson J., Dong Y.N.et al. (2018) Role of frataxin protein deficiency and metabolic dysfunction in Friedreich ataxia, and autosomal recessive mitochondrial disease. Neuronal Signal. 2, NS20180060 10.1042/NS20180060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marmolino D., Manto M., Acquaviva F.et al. (2010) PGC-1alpha down-regulation affects the antioxidant response in Friedreich’s ataxia. PLoS ONE 5, e10025 10.1371/journal.pone.0010025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shan Y., Schoenfeld R.A., Hayashi G.et al. (2013) Frataxin deficiency leads to defects in expression of antioxidants and Nrf2 expression in dorsal root ganglia of the Friedreich’s ataxia YG8R mouse model. Antioxid. Redox Signal. 19, 1481–1493 10.1089/ars.2012.4537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li K. (2019) Iron pathophysiology in Friedreich’s ataxia. Adv. Exp. Med. Biol. 1173, 125–143 10.1007/978-981-13-9589-5_7 [DOI] [PubMed] [Google Scholar]
- 24.Chiang S., Huang M.L.H., Park K.C. and Richardson D.R. (2020) Antioxidant defense mechanisms and its dysfunctional regulation in the mitochondrial disease, Friedreich’s ataxia. Free Radic. Biol. Med. 159, 177–188 10.1016/j.freeradbiomed.2020.07.019 [DOI] [PubMed] [Google Scholar]
- 25.Wilson R.B., Lynch D.R., Farmer J.M., Brooks D.G. and Fischbeck K.H. (2000) Increased serum transferrin receptor concentrations in Friedreich ataxia. Ann. Neurol. 47, 659–661 [DOI] [PubMed] [Google Scholar]
- 26.Wilson R.B., Lynch D.R. and Fischbeck K.H. (1998) Normal serum iron and ferritin concentrations in patients with Friedreich’s ataxia. Ann. Neurol. 44, 132–134 10.1002/ana.410440121 [DOI] [PubMed] [Google Scholar]
- 27.Alsina D., Purroy R., Ros J. and Tamarit J. (2018) Iron in Friedreich ataxia, a central role in the pathophysiology or an epiphenomenon? Pharmaceuticals (Basel) 11, 89 10.3390/ph11030089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ward P.G.D., Harding I.H., Close T.G.et al. (2019) Longitudinal evaluation of iron concentration and atrophy in the dentate nuclei in friedreich ataxia. Mov. Disord. 34, 335–343 10.1002/mds.27606 [DOI] [PubMed] [Google Scholar]
- 29.Harding I.H., Raniga P., Delatycki M.B.et al. (2016) Tissue atrophy and elevated iron concentration in the extrapyramidal motor system in Friedreich ataxia, the IMAGE-FRDA study. J. Neurol. Neurosurg. Psychiatry 87, 1261–1263 10.1136/jnnp-2015-312665 [DOI] [PubMed] [Google Scholar]
- 30.Myers L.M., Lynch D.R., Farmer J.M., Friedman L.S., Lawson J.A. and Wilson R.B. (2008) Urinary isoprostanes in Friedreich ataxia: lack of correlation with disease features. Mov. Disord. 23, 1920–1922 10.1002/mds.22038 [DOI] [PubMed] [Google Scholar]
- 31.Elincx-Benizri S., Glik A., Merkel D.et al. (2016) Clinical experience with deferiprone treatment for Friedreich ataxia. J. Child Neurol. 31, 1036–1040 10.1177/0883073816636087 [DOI] [PubMed] [Google Scholar]
- 32.La Rosa P., Petrillo S., Fiorenza M.T., Bertini E.S. and Piemonte F. (2020) Ferroptosis in Friedreich’s ataxia, a metal-induced neurodegenerative disease. Biomolecules 10, 1551 10.3390/biom10111551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cotticelli M.G., Xia S., Lin D.et al. (2019) Ferroptosis as a novel therapeutic target for Friedreich’s ataxia. J. Pharmacol. Exp. Ther. 369, 47–54 10.1124/jpet.118.252759 [DOI] [PubMed] [Google Scholar]
- 34.Turchi R., Faraonio R., Lettieri-Barbato D. and Aquilano K. (2020) An overview of the ferroptosis hallmarks in Friedreich’s ataxia. Biomolecules 10, 1489 10.3390/biom10111489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cotticelli M.G., Forestieri R., Xia S.et al. (2020) Identification of a novel oleic acid analog with protective effects in multiple cellular models of Friedreich ataxia. ACS Chem. Neurosci. 11, 2535–2542 10.1021/acschemneuro.0c00323 [DOI] [PubMed] [Google Scholar]
- 36.Liu J., Bandyopadhyay I., Zheng L., Khdour O.M. and Hecht S.M. (2020) Antiferroptotic Activity of phenothiazine analogues, a novel therapeutic strategy for oxidative stress related disease. ACS Med. Chem. Lett. 11, 2165–2173 10.1021/acsmedchemlett.0c00293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cotticelli M.G., Crabbe A.M., Wilson R.B. and Shchepinov M.S. (2013) Insights into the role of oxidative stress in the pathology of Friedreich ataxia using peroxidation resistant polyunsaturated fatty acids. Redox Biol. 1, 398–404 10.1016/j.redox.2013.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zesiewicz T., Heerinckx F., De Jager R.et al. (2018) Randomized, clinical trial of RT001, early signals of efficacy in Friedreich’s ataxia. Mov. Disord. 33, 1000–1005 10.1002/mds.27353 [DOI] [PubMed] [Google Scholar]
- 39.Zesiewicz T., Salemi J.L., Perlman S.et al. (2018) Double-blind, randomized and controlled trial of EPI-743 in Friedreich’s ataxia. Neurodegener. Dis. Manag. 8, 233–242 10.2217/nmt-2018-0013 [DOI] [PubMed] [Google Scholar]
- 40.Sandi C., Sandi M., Jassal H.et al. (2014) Generation and characterisation of Friedreich ataxia YG8R mouse fibroblast and neural stem cell models. PLoS ONE 9, e89488 10.1371/journal.pone.0089488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tozzi G., Nuccetelli M., Lo Bello M.et al. (2002) Antioxidant enzymes in blood of patients with Friedreich’s ataxia. Arch. Dis. Child. 86, 376–379 10.1136/adc.86.5.376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiralerspong S., Ge B., Hudson T.J. and Pandolfo M. (2001) Manganese superoxide dismutase induction by iron is impaired in Friedreich ataxia cells. FEBS Lett. 509, 101–105 10.1016/S0014-5793(01)03140-4 [DOI] [PubMed] [Google Scholar]
- 43.Petrillo S., Piermarini E., Pastore A.et al. (2017) Nrf2-inducers counteract neurodegeneration in Frataxin-silenced motor neurons, disclosing new therapeutic targets for Friedreich’s ataxia. Int. J. Mol. Sci. 18, 2173 10.3390/ijms18102173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Anzovino A., Chiang S., Brown B.E., Hawkins C.L., Richardson D.R. and Huang M.L. (2017) Molecular alterations in a mouse cardiac model of Friedreich ataxia, an impaired Nrf2 response mediated via upregulation of Keap1 and activation of the Gsk3β axis. Am. J. Pathol. 187, 2858–2875 10.1016/j.ajpath.2017.08.021 [DOI] [PubMed] [Google Scholar]
- 45.La Rosa P., Russo M., D’Amico J.et al. (2019) Nrf2 induction re-establishes a proper neuronal differentiation program in Friedreich’s ataxia neural stem cells. Front. Cell. Neurosci. 13, 356 10.3389/fncel.2019.00356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abeti R., Baccaro A., Esteras N. and Giunti P. (2018) Novel Nrf2-inducer prevents mitochondrial defects and oxidative stress in Friedreich’s ataxia models. Front. Cell. Neurosci. 12, 188 10.3389/fncel.2018.00188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Petrillo S., D’Amico J., La Rosa P., Bertini E.S. and Piemonte F. (2019) Targeting NRF2 for the treatment of Friedreich’s ataxia: a comparison among drugs. Int. J. Mol. Sci. 20, 5211 10.3390/ijms20205211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Silva-Palacios A., Ostolga-Chavarría M., Zazueta C. and Königsberg M. (2018) Nrf2: Molecular and epigenetic regulation during aging. Ageing Res. Rev. 47, 31–40 10.1016/j.arr.2018.06.003 [DOI] [PubMed] [Google Scholar]
- 49.Sahdeo S., Scott B.D., McMackin M.Z.et al. (2014) Dyclonine rescues frataxin deficiency in animal models and buccal cells of patients with Friedreich’s ataxia. Hum. Mol. Genet. 23, 6848–6862 10.1093/hmg/ddu408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lynch D.R., Farmer J., Hauser L.et al. (2018) Safety, pharmacodynamics, and potential benefit of omaveloxolone in Friedreich ataxia. Ann. Clin. Transl. Neurol. 6, 15–26 10.1002/acn3.660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.La Rosa P., Petrillo S., Turchi R.et al. (2021) The Nrf2 induction prevents ferroptosis in Friedreich’s ataxia. Redox Biol. 38, 101791 10.1016/j.redox.2020.101791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lynch D.R., Chin M.P., Delatycki M.B.et al. (2021) Safety and efficacy of omaveloxolone in Friedreich Ataxia (MOXIe Study). Ann. Neurol. 89, 212–225 10.1002/ana.25934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lynch D.R. and Johnson J. (2021) Omaveloxolone: potential new agent for Friedreich ataxia. Neurodegener. Dis. Manag. 11(2), 91–98 10.2217/nmt-2020-0057 [DOI] [PubMed] [Google Scholar]
- 54.Johnson J., Mercado-Ayon E., Mercado-Ayon Y.et al. (2020) Mitochondrial dysfunction in the development and progression of neurodegenerative diseases. Arch. Biochem. Biophys. 28, 108698. [DOI] [PubMed] [Google Scholar]
- 55.Lynch D.R., Willi S.M., Wilson R.B.et al. (2012) A0001 in Friedreich ataxia, biochemical characterization and effects in a clinical trial. Mov. Disord. 27, 1026–1033 10.1002/mds.25058 [DOI] [PubMed] [Google Scholar]
- 56.Meier T., Perlman S.L., Rummey C., Coppard N.J. and Lynch D.R. (2012) Assessment of neurological efficacy of idebenone in pediatric patients with Friedreich’s ataxia, data from a 6-month controlled study followed by a 12-month open-label extension study. J. Neurol. 259, 284–291 10.1007/s00415-011-6174-y [DOI] [PubMed] [Google Scholar]
- 57.Lagedrost S.J., Sutton M.S., Cohen M.S.et al. (2011) Idebenone in Friedreich ataxia cardiomyopathy-results from a 6-month phase III study (IONIA). Am. Heart J. 161, 639–645 10.1016/j.ahj.2010.10.038 [DOI] [PubMed] [Google Scholar]
- 58.Lynch D.R., Perlman S.L. and Meier T. (2010) A phase 3, double-blind, placebo-controlled trial of idebenone in friedreich ataxia. Arch. Neurol. 67, 941–947 10.1001/archneurol.2010.168 [DOI] [PubMed] [Google Scholar]
- 59.Seco-Cervera M., González-Cabo P., Pallardó F.V., Romá-Mateo C. and García-Giménez J.L. (2020) Thioredoxin and Glutaredoxin systems as potential targets for the development of new treatments in Friedreich’s Ataxia. Antioxidants (Basel) 9, 1257 10.3390/antiox9121257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Edenharter O., Schneuwly S. and Navarro J.A. (2018) Mitofusin-dependent ER stress triggers glial dysfunction and nervous system degeneration in a Drosophila Model of Friedreich’s ataxia. Front. Mol. Neurosci. 11, 38 10.3389/fnmol.2018.00038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jasoliya M.J., McMackin M.Z., Henderson C.K., Perlman S.L. and Cortopassi G.A. (2017) Frataxin deficiency impairs mitochondrial biogenesis in cells, mice and humans. Hum. Mol. Genet. 26, 2627–2633 10.1093/hmg/ddx141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.García-Giménez J.L., Gimeno A., Gonzalez-Cabo P.et al. (2011) Differential expression of PGC-1α and metabolic sensors suggest age-dependent induction of mitochondrial biogenesis in Friedreich ataxia fibroblasts. PLoS ONE 6, e20666 10.1371/journal.pone.0020666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Coppola G., Burnett R., Perlman S.et al. (2011) A gene expression phenotype in lymphocytes from Friedreich ataxia patients. Ann. Neurol. 70, 790–804 10.1002/ana.22526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lin H., Magrane J., Rattelle A.et al. (2017) Early cerebellar deficits in mitochondrial biogenesis and respiratory chain complexes in the KIKO mouse model of Friedreich ataxia. Dis. Model Mech. 10, 1343–1352 10.1242/dmm.030502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Coppola G., Marmolino D., Lu D.et al. (2009) Functional genomic analysis of frataxin deficiency reveals tissue-specific alterations and identifies the PPAR gamma pathway as a therapeutic target in Friedreich’s ataxia. Hum. Mol. Genet. 18, 2452–2461 10.1093/hmg/ddp183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Riehle C. and Abel E.D. (2012) PGC-1 proteins and heart failure. Trends Cardiovasc. Med. 22, 98–105 10.1016/j.tcm.2012.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kearney M., Orrell R.W., Fahey M., Brassington R. and Pandolfo M. (2016) Pharmacological treatments for Friedreich ataxia. Cochrane Database Syst. Rev., CD007791 10.1002/14651858.CD007791.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rodríguez-Pascau L., Britti E., Calap-Quintana P.et al. (2021) PPAR gamma agonist leriglitazone improves frataxin-loss impairments in cellular and animal models of Friedreich Ataxia. Neurobiol. Dis. 148, 105162 10.1016/j.nbd.2020.105162 [DOI] [PubMed] [Google Scholar]
- 69.Chavez J.D., Tang X., Campbell M.D.et al. (2020) Mitochondrial protein interaction landscape of SS-31. Proc. Natl. Acad. Sci. U.S.A. 117, 15363–15373 10.1073/pnas.2002250117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mitchell W., Ng E.A., Tamucci J.D.et al. (2020) The mitochondria-targeted peptide SS-31 binds lipid bilayers and modulates surface electrostatics as a key component of its mechanism of action. J. Biol. Chem. 295, 7452–7469 10.1074/jbc.RA119.012094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Szeto H.H. (2014) First-in-class cardiolipin-protective compound as a therapeutic agent to restore mitochondrial bioenergetics. Br. J. Pharmacol. 171, 2029–2050 10.1111/bph.12461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhao H., Li H., Hao S.et al. (2017) Peptide SS-31 upregulates frataxin expression and improves the quality of mitochondria: implications in the treatment of Friedreich ataxia. Sci. Rep. 7, 9840 10.1038/s41598-017-10320-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Johnson J., Mercado-Ayón E., Clark E., Lynch D.R. and Lin H. (2021) Drp1-dependent peptides reverse mitochondrial fragmentation, a homeostatic response in Friedreich ataxia. Pharmacol. Res. Pers. 9(3), e00755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li Y., Lou W., Grevel A.et al. (2020) Cardiolipin-deficient cells have decreased levels of the iron-sulfur biogenesis protein frataxin. J. Biol. Chem. 295, 11928–11937 10.1074/jbc.RA120.013960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Weng L., Laboureur L., Wang Q.et al. (2020) Extra-mitochondrial mouse frataxin and its implications for mouse models of Friedreich’s ataxia. Sci. Rep. 10, 15788 10.1038/s41598-020-72884-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Guo L., Wang Q., Weng L.et al. (2018) Characterization of a new N-terminally acetylated extra-mitochondrial isoform of frataxin in human erythrocytes. Sci. Rep. 8, 17043 10.1038/s41598-018-35346-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Acquaviva F., De Biase I., Nezi L.et al. (2005) Extra-mitochondrial localisation of frataxin and its association with IscU1 during enterocyte-like differentiation of the human colon adenocarcinoma cell line Caco-2. J. Cell Sci. 118, 3917–3924 10.1242/jcs.02516 [DOI] [PubMed] [Google Scholar]
- 78.Clay A., Hearle P., Schadt K. and Lynch D.R. (2019) New developments in pharmacotherapy for Friedreich ataxia. Expert Opin. Pharmacother. 20, 1855–1867 10.1080/14656566.2019.1639671 [DOI] [PubMed] [Google Scholar]
- 79.Yousaf T., Dervenoulas G. and Politis M. (2018) Advances in MRI methodology. Int. Rev. Neurobiol. 141, 31–76 10.1016/bs.irn.2018.08.008 [DOI] [PubMed] [Google Scholar]
- 80.Meijer F.J.A. and Goraj B. (2014) Brain MRI in Parkinson’s disease. Front. Biosci. (Elite Ed.) 6, 360–369 10.2741/e711 [DOI] [PubMed] [Google Scholar]
- 81.Rezende T.J.R., Martinez A.R.M., Faber I.et al. (2017) Structural signature of classical versus late-onset friedreich's ataxia by Multimodality brain MRI. Hum. Brain Mapp. 38, 4157–4168 10.1002/hbm.23655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Selvadurai L.P., Corben L.A., Delatycki M.B.et al. (2020) Multiple mechanisms underpin cerebral and cerebellar white matter deficits in Friedreich ataxia: The IMAGE-FRDA study. Hum. Brain Mapp. 41, 1920–1933 10.1002/hbm.24921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cocozza S., Costabile T., Pontillo G.et al. (2020) Cerebellum and cognition in Friedreich ataxia, a voxel-based morphometry and volumetric MRI study. J. Neurol. 267, 350–358 10.1007/s00415-019-09582-9 [DOI] [PubMed] [Google Scholar]
- 84.Dogan I., Romanzetti S., Didszun C.et al. (2019) Structural characteristics of the central nervous system in Friedreich ataxia: an in vivo spinal cord and brain MRI study. J. Neurol. Neurosurg. Psychiatry 90, 615–617 10.1136/jnnp-2018-318422 [DOI] [PubMed] [Google Scholar]
- 85.Selvadurai L.P., Harding I.H., Corben L.A.et al. (2016) Cerebral and cerebellar grey matter atrophy in Friedreich ataxia: the IMAGE-FRDA study. J. Neurol. 263, 2215–2223 10.1007/s00415-016-8252-7 [DOI] [PubMed] [Google Scholar]
- 86.Harding I.H., Raniga P., Delatycki M.B.et al. (2016) Tissue atrophy and elevated iron concentration in the extrapyramidal motor system in Friedreich ataxia: the IMAGE-FRDA study. J. Neurol. Neurosurg. Psychiatry 87, 1261–1263 10.1136/jnnp-2015-312665 [DOI] [PubMed] [Google Scholar]
- 87.Rezende T.J., Silva C.B., Yassuda C.L.et al. (2016) Longitudinal magnetic resonance imaging study shows progressive pyramidal and callosal damage in Friedreich’s ataxia. Mov. Disord. 31, 70–78 10.1002/mds.26436 [DOI] [PubMed] [Google Scholar]
- 88.Iltis I., Hutter D., Bushara K.O.et al. (2010) (1)H MR spectroscopy in Friedreich’s ataxia and ataxia with oculomotor apraxia type 2. Brain Res. 1358, 200–210 10.1016/j.brainres.2010.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Thomas G.E.C., Leyland L.A., Schrag A.-E.et al. (2020) Brain iron deposition is linked with cognitive severity in Parkinson's disease. J. Neurol. Neurosurg. Psychiatry 91, 418–425 10.1136/jnnp-2019-322042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ward P.G.D., Harding I.H., Close T.G.et al. (2019) Longitudinal evaluation of iron concentration and atrophy in the dentate nuclei in friedreich ataxia. Mov. Disord. 34, 335–343 10.1002/mds.27606 [DOI] [PubMed] [Google Scholar]
- 91.Minoryx Therapeutics (2020) Minoryx’s clinical candidate leriglitazone shows clinical benefit in a proof of concept Phase 2 study in Friedreich´s ataxia.. https://www.minoryx.com/media/minoryx%E2%80%99s_clinical_candidate_leriglitazone_shows_clinical_benefit_in_a_proof_of_concept_phase_2_study_in_friedreichs_ataxia/ [Google Scholar]
- 92.Huang D., Liu D., Yin J., Qian T., Shrestha S. and Ni H. (2017) Glutamate-glutamine and GABA in brain of normal aged and patients with cognitive impairment. Eur. Radiol. 27, 2698–2705 10.1007/s00330-016-4669-8 [DOI] [PubMed] [Google Scholar]
- 93.Wenneberg C., Glenthøj B.Y., Hjorthøj C.et al. (2020) Cerebral glutamate and GABA levels in high-risk of psychosis states: a focused review and meta-analysis of 1H-MRS studies. Schizophr. Res. 215, 38–48 10.1016/j.schres.2019.10.050 [DOI] [PubMed] [Google Scholar]
- 94.Horder J., Petrinovic M.M., Mendez M.A.et al. (2018) Glutamate and GABA in autism spectrum disorder-a translational magnetic resonance spectroscopy study in man and rodent models. Transl. Psychiatry 8, 106 10.1038/s41398-018-0155-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Delatycki M.B. and Bidichandani S.I. (2019) Friedreich ataxia- pathogenesis and implications for therapies. Neurobiol. Dis. 132, 104606 10.1016/j.nbd.2019.104606 [DOI] [PubMed] [Google Scholar]
- 96.Koeppen A.H., Ramirez L., Becker A.B., Feustel P.J. and Mazurkiewicz J.E. (2015) Friedreich Ataxia: failure of GABA-ergic and glycinergic synaptic transmission in the dentate nucleus. J. Neuropathol. Exp. Neurol. 74, 166–176 10.1097/NEN.0000000000000160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Choi C., Zhao C., Dimitrov I.et al. (2009) Measurement of glutathione in human brain at 3T using an improved double quantum filter in vivo. J. Magn. Reson. 198, 160–166 10.1016/j.jmr.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gonen O.M., Moffat B.A., Desmond P.M., Lui E., Kwan P. and O’Brien T.J. (2020) Seven-tesla quantitative magnetic resonance spectroscopy of glutamate, γ-aminobutyric acid, and glutathione in the posterior cingulate cortex/precuneus in patients with epilepsy. Epilepsia 61, 2785–2794 10.1111/epi.16731 [DOI] [PubMed] [Google Scholar]
- 99.Straub S., Mangesius S., Emmerich J.et al. (2020) Toward quantitative neuroimaging biomarkers for Friedreich’s ataxia at 7 Tesla: susceptibility mapping, diffusion imaging, R2 and R1 relaxometry. J. Neurosci. Res. 98, 2219–2231 10.1002/jnr.24701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang X. and Gao F. (2015) Imaging mitochondrial reactive oxygen species with fluorescent probes: current applications and challenges. Free Radic. Res. 49, 374–382 10.3109/10715762.2015.1014813 [DOI] [PubMed] [Google Scholar]
- 101.Wu L., Sedgwick A.C., Sun X., Bull S.D., He X.-P. and James T.D. (2019) Reaction-based fluorescent probes for the detection and imaging of reactive oxygen, nitrogen, and sulfur species. Acc. Chem. Res. 52, 2582–2597 10.1021/acs.accounts.9b00302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Maulucci G., Bačić G., Bridal L.et al. (2016) Imaging reactive oxygen species-induced modifications in living systems antioxid redox signal. Antioxid. Redox Signal. 24, 939–958 10.1089/ars.2015.6415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lynch D.R., Lech G., Farmer J.M.et al. (2002) Near infrared muscle spectroscopy in patients with Friedreich’s ataxia. Muscle Nerve 25, 664–673 10.1002/mus.10077 [DOI] [PubMed] [Google Scholar]
- 104.Rajendran H., Dane E., Conley J. and Tantama M. (2016) Imaging adenosine triphosphate (ATP). Biol. Bull. 231, 73–84 10.1086/689592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lobas M.A., Tao R., Nagai J.et al. (2019) A genetically encoded single-wavelength sensor for imaging cytosolic and cell surface ATP. Nat. Commun. 10, 711 10.1038/s41467-019-08441-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Takaine M., Ueno M., Kitamura K., Imamura H. and Yoshida S. (2019) Reliable imaging of ATP in living budding and fission yeast. J. Cell Sci. 132, jcs230649 10.1242/jcs.230649 [DOI] [PubMed] [Google Scholar]
- 107.Chung B.T., Chen H.-Y., Gordon J.et al. (2019) First hyperpolarized [2-13 C] pyruvate MR studies of human brain metabolism. J. Magn. Reson. 309, 106617 10.1016/j.jmr.2019.106617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Marin-Valencia I., Cho S.K., Rakheja D.et al. (2012) Glucose metabolism via the pentose phosphate pathway, glycolysis and Krebs cycle in an orthotopic mouse model of human brain tumors. NMR Biomed. 25, 1177–1186 10.1002/nbm.2787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cavallari E., Carrera C., Aime S. and Reineri F. (2018) Studies to enhance the hyperpolarization level in PHIP-SAH-produced C13-pyruvate. J. Magn. Reson. 289, 12–17 10.1016/j.jmr.2018.01.019 [DOI] [PubMed] [Google Scholar]
- 110.Worth A.J., Basu S.S., Deutsch E.C.et al. (2015) Stable isotopes and LC-MS for monitoring metabolic disturbances in Friedreich’s ataxia platelets. Bioanalysis 7, 1843–1855 10.4155/bio.15.118 [DOI] [PMC free article] [PubMed] [Google Scholar]