Abstract
AIM
To review data on the impact of the COVID-19 pandemic on interventional radiology (IR) services.
MATERIALS AND METHODS
A systematic review of the available studies was performed according to the PRISMA guidelines.
RESULTS
A total of 14 studies met the inclusion criteria. IR caseload reduced between 16.8–80%, with elective activity affected more than emergency work. Trainees also experienced a 11–51.9% reduction in case volumes and many were redeployed to critical care. IR departments re-organised operations and personnel, and many continued to offer 24/7 services and support critical care areas through redeployment of staff. The majority of studies report no significant issues with the availability of personal protective equipment and that local or national governing body or radiology society guidelines were followed.
CONCLUSION
The COVID-19 pandemic reduced case volumes and training opportunities. IR departments showed flexibility in service delivery. The lessons learned offer novel insights into how services and training can be reorganised to ensure that IR continues to thrive.
Introduction
The COVID-19 pandemic started in Wuhan, China, in December 2019 and was declared a public health emergency by the World Health Organization on 30 January 2020. To date, there have been 100 million cases worldwide and this number continues to grow. In many countries, the course of the pandemic has been protracted with multiple waves of infection. The impact of the pandemic on healthcare has been enormous, with all aspects of healthcare delivery being affected, including service delivery and training.1 , 2
Interventional radiology (IR) is a unique specialty that requires both diagnostic imaging and procedures. The pandemic has resulted in a reduction in diagnostic imaging as a whole, with one study reporting a case volume reduction of 12–28% in 2020 compared to the equivalent period in 2019.3 Additionally, the delivery of procedural services has also been impacted by the pandemic.4 A few reports have been published in the literature quantifying the local change of case volume and other aspects of IR service; however, comparisons among institutes in different settings and geographic locations are not available.
The COVID-19 pandemic has also adversely affected IR training. The cancellation of both urgent and elective procedures has meant a severe reduction in training opportunities. The pandemic has already lasted 1 year, which represents a significant proportion of an interventional radiologist's training time given that the length of IR-specific training typically ranges from 1–3 years.5 It is clear that although training continues to be affected, innovative solutions will be required to ensure that the impact on trainee education is as limited as possible.
The aim of this review was to summarise the existing literature with quantifiable data on the impact that the COVID-19 pandemic has had on IR services and training around the world.
Materials and methods
This systematic review was conducted according to the 2009 Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. A literature search of the PubMed databases was performed by using the following key terms “interventional radiology” AND “COVID-19”, with a combination of “impact” “service” “training” “education” “survey”, for publications between 1 January 2020 and 15 January 2021. There were no language limitations in our search.
Studies with the following characteristics were included in the analysis: prospective or retrospective studies; qualitative surveys; and studies reporting on the effect of COVID-19 on vascular and non-vascular IR. Case reports and publications on interventional neuroradiology, opinions or commentaries without quantitative data, policies, and guidelines were excluded. The quality of studies was assessed using the Methodological Index for Non-Randomised Studies (MINORS)6 (Electronic Supplementary Material Table S1). Data regarding the location, period and duration of data collection, effect on IR-related caseload, training, and staffing were extracted.
Results
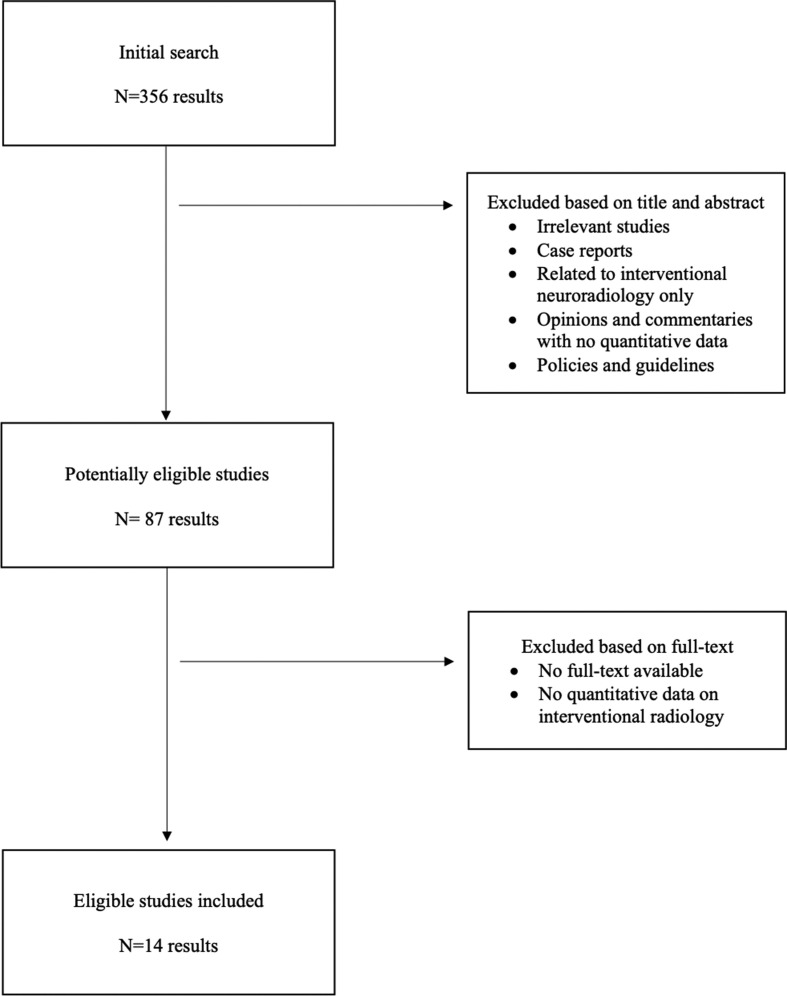
Of the 356 studies identified, 14 studies met the inclusion criteria (Fig 1 ). Four studies were qualitative surveys and 10 retrospective, observational studies. Eight studies were from the USA, three from the UK, and one each from Italy, Canada, and China. Total MINORS scores of included studies ranged from 4–12, with the majority (n=8) of studies scoring 12 (out of 24 for comparative studies; Electronic Supplementary Material Table S1).
Figure 1.
Flow chart demonstrating the search strategy for this study.
Personal protective equipment (PPE) is a major factor in order to protect staff from the virus. The majority of studies did not report any gross issues with the availability of PPE and the majority reported following the guidelines of the local or national governing body or radiology society. Regarding testing for asymptomatic infected staff, only one study7 reported that widespread hospital testing for COVID-19 was not available routinely during the first wave.
Depending on the study period, geographic location, and hospital setting, the impact on case volumes varied markedly. This is also reflected in national surveys with responders from various healthcare settings. Thirteen studies reported changes in overall case volume, 11 of which provided the breakdown data on urgent versus elective, modality-based or interventional oncology caseloads. Overall, the majority of studies reported case volume reduction between 16.8% and 62% with only two studies reporting overall caseload volume reductions of >80%.8 , 9 Of note, although most studies reported marked reduction in urgent IR activity, Zhong et al. 10 reported a 0.5% drop in urgent IR workload with pooled data from six UK centres. Elective and outpatient IR cases appeared to be the most affected by the pandemic as the majority of studies reported reduction in volumes that ranged from 29.6% to 100%. Due to differences in category definition, healthcare settings, national/local policy and study periods, direct comparisons among these studies were not possible; however, one notable trend was to preserve interventional oncology capacity by modifying workflow, applying other peri-procedural precautions and utilising day/outpatient facilities.7 , 11, 12, 13
Three studies mentioned provision of COVID-19-specific services, including establishing a portable central line team and increased image-guided gastrostomy9 , 10 , 12 , 13; however, these were not well quantified. Other IR clinical activities, most notably outpatient clinics and multidisciplinary meetings (MDMs), were also affected with three studies describing the adoption of virtual consultation and meetings to minimise exposure and provide continuous care.14 , 15
Redeployment was detailed in three studies focusing on different staff groups including IR fellows,16 allied healthcare professionals,13 and all imaging staff,17 and this ranged from 16 to 56% depending on local demand. Other changes in staffing included creating intensive care unit (ICU)-based IR teams to offer local support,13 changing normal day-to-day practice to allow 24/7 service to continue,9 , 11 splitting into two or more teams working on alternate weeks to ensure that if one team becomes infected there is a backup team.15
The impact on IR training was assessed in four studies with case volume reduction for the trainees ranging from 11–51.9%,14, 15, 16 whereas in one study all IR trainees were redeployed to ICU.12 As compensation for the reduction in practical training, many centres reported increasing the number of online teaching sessions.9 , 14 In addition to case volume reduction parallel to the overall service reduction, trainees also faced other issues such as examination cancellations post cancellation, and job deferral which have future implications.15 , 16 No studies provided quantitative data on the reduced opportunities for medical students or juniors doctors prior to IR training. Similarly, no studies provided quantified data on strategies used to counteract the impact on training, e.g., virtual tutorials/conferences, practical skills simulation, etc.
Discussion
The COVID-19 pandemic has disrupted healthcare on an unprecedented scale. The present study identified studies with quantifying data on the impact on IR services in multiple domains, especially regarding service provision and training.
The availability of PPE was a major concern during the early stages of the pandemic, with many healthcare staff reporting shortages.18 None of the studies provided quantitative data on the availability of PPE, although no major issues on the availability of PPE were reported. A significant reduction in IR case volume across the globe was observed, depending on the timing of local surge and service reorganisation of individual institutes, with elective and outpatient IR work being the worst affected. This is in keeping with national survey results from several countries, as well as the authors' own experiences. Some reported that the volume of time-sensitive oncological cases were maintained or reduced to a lesser degree compared with other IR activities.11 , 12 , 14 Additionally, it was shown that the impact on IR services was less than that on surgical and medical procedures (such as endoscopy and coronary catheterisation), which traditionally have considerable practice overlap.12 , 19 These are due to the minimally invasive nature of IR and the lower likelihood of potentially aerosolising procedures. It could also be attributed to IRs rapid reconfiguration of the departmental workflow to accommodate patients at low and high risk of COVID-197 , 8 , 11 and, particularly, by utilising outpatient/day-case facilities efficiently.13 Some of these procedures, such as tumour embolisation, may have been performed as inpatient cases in the UK in the pre-COVID era. Successful practice adaptations during the pandemic can potentially provide templates for post-COVID era IR practice modification with a stronger emphasis on dedicated outpatient IR pathways, staffing, and facilities.
The literature also demonstrated a comparatively lower reduction in IR volumes compared to many diagnostic radiology subspecialties/modalities.3 , 17 With regards to urgent IR procedures, the UK and Canadian national surveys9 , 15 showed a high proportion of departments experiencing volume reduction. Zhong et al. 10 presented interesting data from six UK centres showing three experiencing a 38–145% increase, the other three a 25–80% decrease, and overall, a 0.5% caseload reduction. The increased demand may be attributed to the adaptability of IR, particularly by providing line services and bedside procedures to support critical care services.9 , 10
IR departments experienced organisational changes, both in terms of personnel and operations. Some IR departments experienced staff redeployment and shortage, involving IR trainees, nurses, radiographers, and other allied healthcare professionals, which is likely to recur in future surges. Redeployed IR trainees could add value to ICU and ward settings with their procedural as well as interpretation skills; IR nursing staff, particularly those with prior critical care training, could alleviate staff shortages. For those who remained in IR services, rotas were restructured to allow for the increased sickness leave, for example, by splitting personnel up into multiple teams.15 Operational changes included implementing enhanced cleaning protocols, designating COVID-19 rooms and optimising patient flow in the department to take into account social distancing and infection control measures.7 , 8 Overall, proactive re-organisation of IR services has allowed continuation of essential IR services as well as supporting critical care. Staffing support to IR departments should be considered in light the adaptability of IR to share the workload with other specialties and to maintain the provision of a broad range treatments during the crisis. In future surges, a careful balance should be struck between efficient IR staff redeployment and sustainable IR service provision at healthcare system levels.
Training of IR trainee was affected primarily by reduced case volume, parallel to global caseload reduction. From a practical aspect, a limited number of trainers, as well as the narrower scope of procedural variety, has also been highlighted as an additional domain of training impact.14 These issues are not unique to IR and are also experienced by surgical and other medical procedural specialties. In particular, the training of surgeons and endoscopists were also disrupted in similar ways.20, 21, 22, 23, 24 A simulation-based curriculum25 could supplement practical skills training and maintenance of existing procedural skills. Multiple studies have shown that there is a role of simulation training in both the acquisition of endovascular skills for new learners, as well as learning for more experienced operators26; however, it is not able to completely replace procedural training in real cases. In addition to simulation, a survey among ophthalmology trainees24 showed that web-based real-time case presentations for clinical training and discussion of edited surgical videos for procedural training are the most desired training supplementation, with potential to be adapted for IR training. Uniquely for IR trainees, the diagnostic and multidisciplinary collaboration aspects of IR training could be suitably supplemented by virtual didactic teaching and MDMs. Furthermore, parallel to IR trainees' experience, medical students' and pre-specialty trainee doctors' exposure to IR has also reduced. Although there are no quantifying data on this, the present authors have observed prolonged access reduction or restriction to IR by medical students and non-IR trainee doctors locally due to infection-control requirements.
It is probable that IR trainee recruitment would be affected in the near term, particularly when clinical exposure is a key determinant for IR career choices.27 Virtual education platforms that incorporate simulation, live-streamed, or recorded cases, as well as didactic teaching, could increase prospective trainees' exposure to IR. Indeed, virtual platforms are now widely adapted for patient consultations and MDMs.15 This can be an effective way to reduce unnecessary travel and physical contact for both patients and health professionals. Remote access to MDMs is also a valuable education resource for more junior IR and diagnostic radiology trainees. In contrast, Norbash et al. 28 warned that, although “tele-reporting” minimises radiologists' infection risks at work, it may have long-term impact on relationships with trainees as well as other radiology colleagues and referrers.
The present study had several limitations. This was a retrospective study investigating data that were published, potentially introducing a selection bias. The majority of the studies were from the North America, with only four studies from Europe, and one from Asia and, as a result, the data presented in this study might not fully reflect the situation elsewhere. Furthermore, the IR case mix regarding emergency versus elective priority and procedures differed among countries and departments; this was not investigated further in the present study, as the data published did not allow for this. The relatively low MINORS scores of the studies reflect their methodological quality and high risk of bias; this was largely expected due to their retrospective nature, lack of follow-up, and the use of historical data.
In conclusion, the COVID-19 pandemic had a significant impact on the practice of IR by reducing case volumes and training opportunities. Generally, IR departments showed their ability to adapt and effectively mitigate the impact of the pandemic. The lessons learned offer novel insights into how services can be reorganised and training supplemented, in order to ensure that IR continues to thrive during and after the crisis.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.crad.2021.05.001.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Propper C., Stoye G., Zaranko B. The wider impacts of the coronavirus pandemic on the NHS. Fisc Stud. 2020 Jun 26;41(2):345–356. doi: 10.1111/1475-5890.12227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edigin E., Eseaton P.O., Shaka H. Impact of COVID-19 pandemic on medical postgraduate training in the United States. Med Educ Online. 2020 Jan 1;25(1):1774318. doi: 10.1080/10872981.2020.1774318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naidich J.J., Boltyenkov A., Wang J.J. Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J Am Coll Radiol. 2020 Jul 1;17(7):865–872. doi: 10.1016/j.jacr.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Søreide K., Hallet J., Matthews J.B. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020 Sep;107(10):1250–1261. doi: 10.1002/bjs.11670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mandal I., Minocha A., Yeung J. Interventional radiology training: a comparison of 5 English-speaking countries. Br J Radiol. 2020 Jan;93(1105):20190340. doi: 10.1259/bjr.20190340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slim K., Nini E., Forestier D. Methodological index for non-randomised studies (Minors): development and validation of a new instrument. ANZ J Surg. 2003 Sep 1;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 7.Rajakulasingam R., Da Silva E.J., Azzopardi C. Standard operating procedure of image-guided intervention during the COVID-19 pandemic: a combined tertiary musculoskeletal oncology centre experience. Clin Radiol. 2020 Oct 1;75(10):794.e19–794.e26. doi: 10.1016/j.crad.2020.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu H.D., Zeng C.H., Lu J. COVID-19: what should interventional radiologists know and what can they do? J Vasc Interv Radiol. 2020;31:876–881. doi: 10.1016/j.jvir.2020.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rostampour S., Cleveland T., White H. Response of UK interventional radiologists to the COVID-19 pandemic – survey findings. CVIR Endovasc. 2020 Jun 26;3(1):41. doi: 10.1186/s42155-020-00133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhong J., Datta A., Gordon T. The impact of COVID-19 on interventional radiology services in the UK. Cardiovasc Intervent Radiol. 2021 Jan 1;44(1):134–140. doi: 10.1007/s00270-020-02692-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iezzi R., Valente I., Cina A. Longitudinal study of interventional radiology activity in a large metropolitan Italian tertiary care hospital: how the COVID-19 pandemic emergency has changed our activity. Eur Radiol. 2020 Dec 1;30(12):6940–6949. doi: 10.1007/s00330-020-07041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manna S., Voutsinas N., Maron S.Z. Leveraging IR’s adaptability during COVID-19: a multicenter single urban health system experience. J Vasc Interv Radiol. 2020;31:1192–1194. doi: 10.1016/j.jvir.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cahalane A.M., Cui J., Sheridan R.M. Changes in interventional radiology practice in a tertiary academic center in the United States during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020 Jul 1;17(7):873–877. doi: 10.1016/j.jacr.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gabr A.M., Li N., Schenning R.C. Diagnostic and interventional radiology case volume and education in the age of pandemics: impact analysis and potential future directions. Acad Radiol. 2020 Oct 1;27(10):1481–1488. doi: 10.1016/j.acra.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel N.R., El-Karim G.A., Mujoomdar A. Overall impact of the COVID-19 pandemic on interventional radiology services: a Canadian perspective. Can Assoc Radiol J. 2020 Aug 30 doi: 10.1177/0846537120951960. 846537120951960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiao N., Gordon A.C., Thornburg B. Impact of COVID-19 on IR fellowship. J Vasc Interv Radiol. 2020 Sep;31(9):1492–1494. doi: 10.1016/j.jvir.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi J., Giess C.S., Martin T. Radiology workload changes during the COVID-19 pandemic: implications for staff redeployment. Acad Radiol. 2021 Jan 1;28(1):1–7. doi: 10.1016/j.acra.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woolley K., Smith R., Arumugam S. Personal protective equipment (PPE) guidelines, adaptations and lessons during the COVID-19 pandemic. Ethics Med Publ Heal. 2020 Jul 1;14:100546. doi: 10.1016/j.jemep.2020.100546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel M.V., Ahmed O., Hennemeyer C. IR is an operational and financial hedge for hospitals during COVID-19. J Vasc Interv Radiol. 2020;31:1724–1726. doi: 10.1016/j.jvir.2020.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pawlak K.M., Kral J., Khan R. Impact of COVID-19 on endoscopy trainees: an international survey. Gastrointest Endosc. 2020 Oct;92(4):925–935. doi: 10.1016/j.gie.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marasco G., Nardone O.M., Maida M. Impact of COVID-19 outbreak on clinical practice and training of young gastroenterologists: a European survey. Dig Liver Dis. 2020 Dec;52(12):1396–1402. doi: 10.1016/j.dld.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siau K., Iacucci M., Dunckley P. The impact of COVID-19 on gastrointestinal endoscopy training in the United Kingdom. Gastroenterology. 2020 Oct;159(4):1582–1585.e3. doi: 10.1053/j.gastro.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hau H.-M., Weitz J., Bork U. Impact of the COVID-19 pandemic on student and resident teaching and training in surgical oncology. J Clin Med. 2020 Oct 26;9(11):3431. doi: 10.3390/jcm9113431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrara M., Romano V., Steel D.H. Reshaping ophthalmology training after COVID-19 pandemic. Eye. 2020 Nov 1;34(11):2089–2097. doi: 10.1038/s41433-020-1061-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kesselman A., Lamparello N.A., Malhotra A. Endovascular simulation as a supplemental training tool during the COVID-19 national emergency. Clin Imag. 2020 Nov 1;67:72–73. doi: 10.1016/j.clinimag.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mandal I., Ojha U. Training in interventional radiology: a simulation-based approach. J Med Educ Curric Dev. 2020 Jan 13;7 doi: 10.1177/2382120520912744. 238212052091274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu Y., Pervez A., Theodoulou I. Future interventional radiologists and where to find them—insights from five UK interventional radiology symposia for junior doctors and medical students. Cardiovasc Intervent Radiol. 2021 Feb 1;44(2):300–307. doi: 10.1007/s00270-020-02655-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Norbash A.M., Van Moore A., Recht M.P. Early-stage radiology volume effects and considerations with the coronavirus disease 2019 (COVID-19) pandemic: adaptations, risks, and lessons learned. J Am Coll Radiol. 2020 Sep 1;17(9):1086–1095. doi: 10.1016/j.jacr.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.