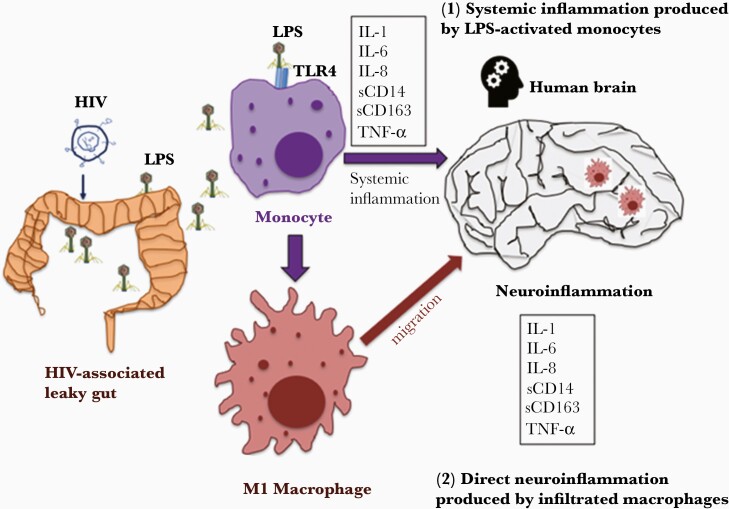
Figure 3.
The mechanisms of plasma lipopolysaccharide (LPS)–mediated neuroinflammation in human immunodeficiency virus (HIV) disease. HIV infection is associated with a comprised mucosal barrier (eg, gut), which results in systemic microbial translocation (eg, bacterial LPS). There are at least 2 potential mechanisms accounting for plasma LPS-mediated neuroinflammation in HIV: (1) increased circulating microbial LPS persistently activates monocytes to produce proinflammatory cytokines in the circulation, which affect the brain as well; (2) increased circulating microbial LPS persistently activates monocytes to differentiate to M1 macrophages, which migrate to tissue sites such as brain and mediate neuroinflammation. Abbreviations: HIV, human immunodeficiency virus; IL, interleukin; LPS, lipopolysaccharide; sCD14, soluble CD14; sCD163, soluble CD163; TLR, Toll-like receptor; TNF, tumor necrosis factor.