Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has greatly affected daily life. COVID-19 often causes asymptomatic or mild disease in children; however, delayed routine childhood immunization is a concern, as it could increase the risk of vaccine-preventable disease. No study has evaluated the status of childhood vaccinations in Japan during the COVID-19 pandemic.
Methods
This retrospective observational study evaluated the number of vaccine doses administered to children in 4 Japanese cities (2 cities in the Tokyo metropolitan area and 2 cities far from Tokyo) during the period from 2016 to 2020. Vaccine doses administered between January and September 2020 during the COVID-19 pandemic were compared, by month, with those given during 2016–2019. Age-stratified demographic data were collected to determine whether factors other than change in the child population over time affected vaccination trends.
Results
In all cities the decrease in vaccine doses administered was most apparent in March and April 2020, i.e., just before or coincident with the declaration of a nationwide COVID-19 emergency on April 7, 2020. The decrease started as early as February in the Tokyo metropolitan area. As child age increased, the decrease became more apparent. Before the lift of national emergency on May 25, catch-up of the vaccination was observed in all age groups in all cities. Vaccine doses persistently increased in older age groups but not in infants. The overall vaccination trends did not differ significantly among the 4 cities.
Conclusions
The COVID-19 pandemic significantly affected routine childhood immunization in Japan. Thus, a nationwide electronic surveillance system and announcements for guardians to encourage timely routine immunization are warranted.
Keywords: Routine immunization, Vaccination, Infants, Children, COVID-19, Pandemic
Abbreviations: BCG, Bacille de Calmette et Guérin; COIID, Committee on Immunization and Infectious Diseases; COVID-19, coronavirus disease 2019; DTaP-IPV, diphtheria tetanus acellular pertussis and inactivated polio; DT, diphtheria-tetanus; HepB, hepatitis B virus; Hib, Haemophilus influenzae type b; JE, Japanese encephalitis; JPS, Japan Pediatric Society; MR, measles and rubella; NIP, national immunization program; PCV13, 13-valent pneumococcal conjugate vaccine; VZV, varicella-zoster virus
1. Introduction
The SARS-CoV-2 was isolated on January 7, 2020 in China [1], and the first Japanese patient with coronavirus disease 2019 (COVID-19) was confirmed on January 15, 2020 in Kanagawa Prefecture in the Tokyo metropolitan area [2]. COVID-19 later rapidly spread throughout Japan, and the first pediatric patient with COVID-19 was confirmed in February in Hokkaido, the northernmost large island of Japan [3]. A national emergency was declared on April 7, 2020 for 7 prefectures, including Tokyo and other large cities, and was extended to the entire country on April 16, 2020. The emergency was lifted on May 14 for 39 prefectures, and on May 25, 2020 for the remaining 8 prefectures, which included Tokyo and other large cities. During the COVID-19 pandemic the public has been asked to refrain from nonessential outings, to limit potential sick contacts. Clinics and hospitals have delayed nonessential and nonurgent practices, including regular outpatient visits and elective surgery. The pandemic has forced changes to management of pediatric cancer [4] and allergic diseases, including asthma [5], [6]. Since the beginning of the pandemic, fewer pediatric patients have been presenting at emergency departments [7], which reflects decreases in admissions attributable to infections by viruses [8] and bacteria [9]. This decrease in infections is due to the absence of opportunities for pathogen transmission by droplets or personal contact. However, the reduction in admissions has had detrimental consequences, including increases in appendiceal perforation [10], delays in intervention for severe infectious diseases [8], and increased mortality [11]. The delay in access is mainly attributable to guardians’ concerns regarding possible COVID-19 infection when visiting clinics or hospitals [8], [11].
To maximize protection from vaccine-preventable diseases, timely vaccination is important in routine childhood immunization [12]. However, guardians’ fear of COVID-19 infection has delayed routine childhood immunization in several countries, including the United States [13], [14], [15], [16], United Kingdom [17], Netherlands [18], Singapore [19], and Pakistan [20]. The Committee on Immunization and Infectious Diseases (COIID) of the Japan Pediatric Society (JPS) thus announced to the public on May 1, 2020 that routine childhood immunization is essential and urgent [21] and released data on vaccine dose decreases in February and March 2020 for children aged 1 year or older in Kawasaki City, in the Tokyo metropolitan area [22]. Routine childhood immunization must remain a priority of pandemic response, even during stay-at-home periods [23], to ensure that Japan does not backtrack from recent progress in the Japanese national immunization program (NIP) [24]. Because data on the delay in routine childhood immunization in Japan are scarce, we surveyed the status of child vaccinations in 4 cities in Japan during the 2020 COVID-19 pandemic.
2. Materials and Methods
2.1. Study population and locations
This retrospective observational study surveyed vaccine doses administered to children in 2 cities in and 2 cities distant from the Tokyo metropolitan area. The former include Kawasaki City, in Kanagawa Prefecture (population, 1,530,000 in 2020), and Fuchu City in Tokyo (population, 260,000 in 2020), located in the Tokyo metropolitan area. The latter includes Niigata City (population, 800,000 in 2020), located in the northern area of the main island and the capital of Niigata Prefecture, and Nagasaki City (population, 420,000 in 2020), located on the southern island of Kyushu and the capital of Nagasaki Prefecture (Supplementary Fig. 1). We selected these 4 cities because data were available for these cities from COIID members of the JPS.
To determine whether vaccination trends were affected by factors other than change in the child population over time, age-stratified demographic data were collected by using official publications on the websites of the municipal offices for each city. Demographic data for January during the study years were used to determine the population in the corresponding year in Niigata [25] and Fuchu [26]. Because age-stratified demographic data were not published for other months, demographic data for October from the national census during the study years were used to determine the populations in the following year in Kawasaki [27] and Nagasaki [28].
2.2. Vaccine records
Data on vaccination in the Japanese NIP between January and September during the years 2016–2020 were collected from various sources, including the Kawasaki and Niigata health centers, the Nagasaki municipal office, and the Fuchu City Medical Association. The vaccines evaluated in this study were the hepatitis B virus (HepB), Bacille de Calmette et Guérin (BCG), measles and rubella (MR), varicella-zoster virus (VZV), Japanese encephalitis (JE), and diphtheria-tetanus (DT) vaccines. These vaccines were carried out in the same manner, no mass immunization was done in the 4 cities.
In the Japanese NIP, the 3 doses of the HepB vaccine are recommended at 2, 3, and 7–8 months, and the BCG vaccine is recommended at 5–7 months. The first dose (MR1) and second dose of the MR (MR2) vaccine are recommended at age 1 year and 5–6 years, respectively. The first and second doses of VZV (VZV1/2) are recommended at age 1 year (age 2 years, at the latest), with an interval of 6–12 months (at least 3 months). The primary series of 3 doses of the JE vaccine (JE1–3) are recommended at age 3–4 years, with a booster dose (JE4) at age 9–12 years. The DT vaccine is recommended at age 11–12 years.
Because we were unable to distinguish between the primary series and booster dose of vaccines in the data from Niigata and Fuchu, a few vaccines in the NIP, including the Haemophilus influenzae type b (Hib) vaccine, 13-valent pneumococcal conjugate vaccine (PCV13), and diphtheria, tetanus, acellular pertussis, and inactivated polio (DTaP-IPV) vaccine, were not evaluated. Rotavirus vaccines, which were included in the NIP in October 2020, were also removed. Additionally, human papillomavirus vaccines were not analyzed because of the temporary withdrawal of the active recommendation for these vaccines by the Japanese government from 2013 [24]. Mumps and influenza vaccines, which are not in the NIP and are categorized as voluntary vaccines, were also not included.
2.3. Statistical analysis
The change in child population was calculated by comparing the population in 2020 with the average population during 2016–2019 for each age category. The change in percentage of the population was considered as a reference value to determine whether the change in vaccine doses was different from the change in the population.
The numbers of vaccine doses administered in 2020 were compared with the average numbers of vaccine doses for 2016 through 2019, by month. The proportional change was expressed as a percentage (i.e., vaccine dose administered in 2020 divided by the average vaccine dose for 2016–2019 × 100(%)). Because HepB vaccine was added to the NIP in October 2020, we calculated the average vaccine doses used between 2017 and 2019, for comparison. In addition, some data for 2016 were unavailable, namely, data for the BCG vaccine in January and February in Kawasaki; for the MR1, MR2, JE1-3, and JE4 vaccines in Nagasaki and Fuchu; and for the BCG, VZV1/2, and DT vaccines between January and March in Fuchu. In such cases, we used the data for 2017–2019 for comparison.
2.4. Ethics approval
This study was approved by the Ethics Committee of Niigata University (2020–0394).
3. Results
3.1. Changes in the child populations of the 4 study sites from 2016–2019 to 2020
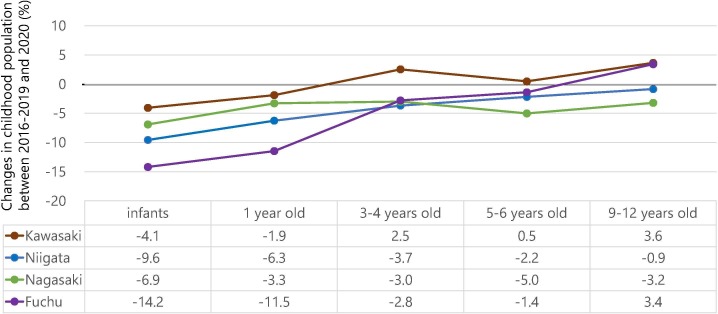
The number of children aged 15 years or younger and the general population in 2020 were 201,462 (13.2%) and 1,530,457, respectively, in Kawasaki, 101,083 (12.8%) and 788,053 in Niigata, 50,650 (12.3%) and 411,421 in Nagasaki, and 36,451 (14.0%) and 260,232 in Fuchu. Percentage change in each age category in 2020 as compared with the average during 2016–2019 is shown in Fig. 1 . Except for an increase in children aged 3 years or older in Kawasaki and those aged 9–12 years in Fuchu, the overall population of children decreased. However, the extent of the reduction decreased as age increased. The decrease was the most prominent in infants: −4.1% in Kawasaki, −9.6% in Niigata, −6.9% in Nagasaki, and −14.2% in Fuchu.
Fig. 1.
Changes in the child populations of the 4 study sites from 2016–2019 to 2020. Change in child population was calculated by comparing the child population in 2020 with the average child population during 2016–2019 for each age category.
3.2. Changes in vaccine doses administered during 2016–2019 and 2020
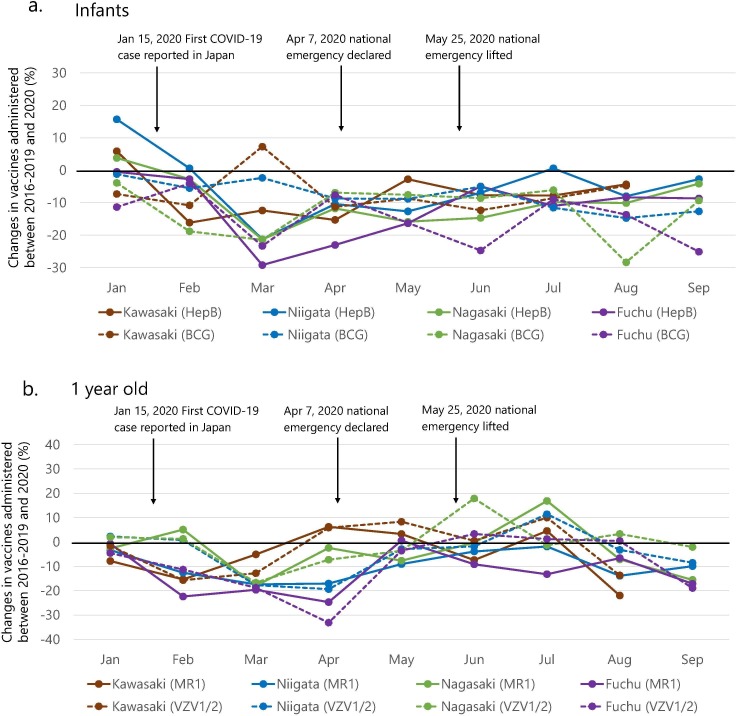
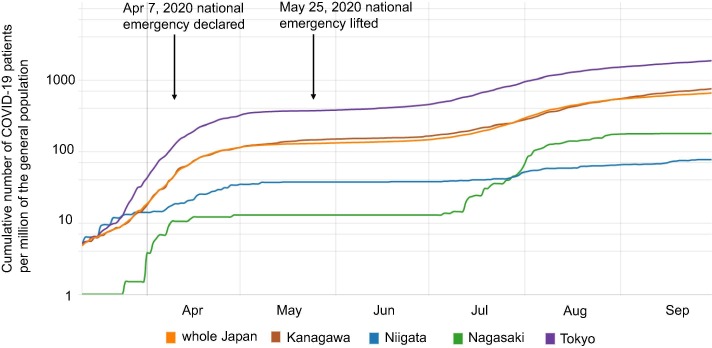
The numbers of vaccine doses administered during the study period at the 4 sites were 197,068 for HepB vaccine, 82,043 for BCG vaccine, 84,785 for MR1 vaccine, 166,697 for VZV1/2 vaccine, 252,037 for JE1-3 vaccine, 98,304 for MR2 vaccine, 106,669 for JE4 vaccine, and 72,143 for DT vaccine. Vaccination trends during the study periods, by age and city, are shown in Fig. 2 . The age of children was classified as infancy, which includes the HepB and BCG vaccines (Fig. 2a), age 1 year, including the MR1 and VZV1/2 vaccines (Fig. 2b), age 3–4 years, including the JE1-3 vaccine (Fig. 2c), age 5–6 years, including the MR2 vaccine (Fig. 2d), and age 9–12 years, including the DT and JE4 vaccines (Fig. 2e). As age increased, the degree of the reduction was more apparent. Before the lifting of the national emergency, vaccination catch-up started in all age groups. An exception to this was Kawasaki, where catch-up started as early as April, the month the national emergency was declared.
Fig. 2.
Changes in childhood vaccination in the 4 cities in January and September from 2016–2019 to 2020. Change in childhood vaccination was calculated by comparing the number of vaccine doses in 2020 with the average number of vaccine doses during 2016–2019 for each month (until August in Kawasaki). The vaccines for each age category were (a) HepB (solid lines) and BCG (dotted lines) for infancy, (b) MR1 (solid lines) and VZV1/2 (dotted lines) for age 1 year, (c) JE1-3 for age 3–4 years, (d) MR2 for age 5–6 years, (e) JE4 (solid lines) and DT (dotted lines) for age 9–12 years. Abbreviations: COVID-19, coronavirus disease 2019; HepB, hepatitis B virus vaccine; BCG, Bacille de Calmette et Guérin vaccine; MR1, first dose of measles and rubella vaccine; VZV1/2, first dose and second dose of varicella-zoster virus vaccine; JE1-3, primary series of 3 doses of Japanese encephalitis vaccine; MR2, second dose of measles and rubella vaccine; JE4, booster dose of Japanese encephalitis vaccine; DT, diphtheria-tetanus vaccine.
Furthermore, the number of vaccine doses significantly increased in older age groups. The range of change in DT and the JE4 vaccines was the largest in children aged 9–12 years (Fig. 2e). All other age groups (Fig. 2b–e) except infants (Fig. 2a), exhibited similar changes; the changes have been below zero since March, except for a 7.3% increase for the BCG vaccine, in March in Kawasaki, and a 0.6% increase for the HepB vaccine, in July in Niigata. The degree of change has been stable over time.
Regarding measles-containing vaccines, the increase in the number of doses administered, in relation to population change, after March, was small for the MR1 vaccine (Fig. 2b), namely, the increase was limited during April, May, and July in Kawasaki; during June and July in Niigata; during April, June, and July in Nagasaki; and during May, June, and August in Fuchu. The periods of increase were longer for the MR2 vaccine and took place between April and August in Kawasaki, between May and August in Niigata, between April and August in Nagasaki, and between May and September in Fuchu (Fig. 2d).
4. Discussion
This study revealed trends in childhood vaccination in Japan during the COVID-19 pandemic. Although the number of vaccine doses administered decreased in March and April 2020 in all age groups, vaccine catch-up was observed later and was more frequent in older age groups. The trends were similar for the 4 geographically distant cities. Maintaining sufficient vaccination coverage is crucial in avoiding a resurgence of vaccine-preventable diseases.
Regarding HepB vaccine in infants, after a considerable decrease in March 2020, no reduction in vaccinations was apparent later (June to September 2020) in the study. With regard to BCG vaccine in infants, there was no considerable catch-up or increase in vaccination as observed in other vaccines in older age groups except for the peak in March in Kawasaki (Fig. 2a). In the United States, similar to the current study, older children demonstrated more apparent decrease in vaccination than younger children [13], [14]. In contrast, the catch-up vaccination was more apparent in children aged ≤24 months than older children [14]. The pandemic had a differential effect on vaccination practice for infants and older children, which probably reflects the feelings of guardians. Those caring for infants in Japan might be more cautious because of the immaturity of their children and more concerned about contracting COVID-19 when going outside for vaccinations.
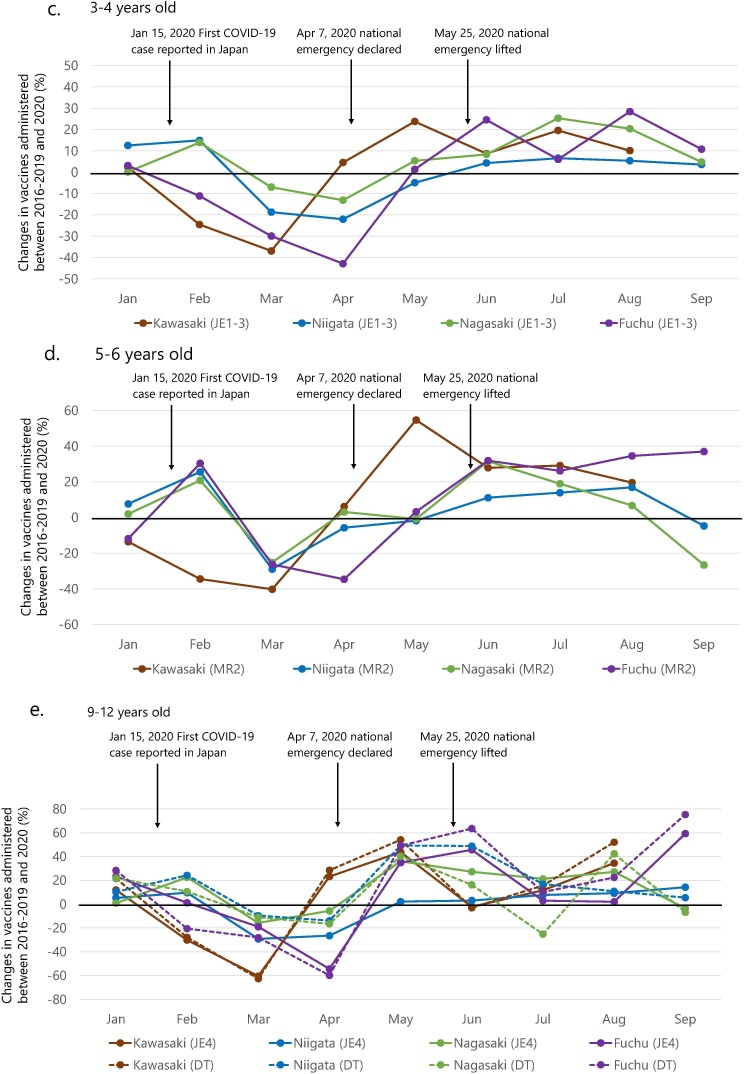
The similarity of vaccination trends for the 4 sites contrasted with the differences in the numbers of COVID-19 patients for the respective prefectures (Fig. 3 ). Trends in the number of COVID-19 patients per million of the general population in each prefecture and all of Japan were visualized by using a graphing website for COVID-19 [29]. As of September 30, 2020, the cumulative number of COVID-19 patients, per million general population, was 653.87 in all of Japan. However, the rate differed significantly for the 4 sites: it was high in the Tokyo metropolitan area, e.g., in Kanagawa Prefecture (749.95) and Tokyo (1848.43), and low in Niigata Prefecture (76.47) and Nagasaki Prefecture (177.84). Overall, the decrease in vaccine doses administered was most apparent in March and April 2020, just before or coincident with the declaration of the COVID-19 national emergency. In Kawasaki and Fuchu, the decrease started as early as February. However, subsequent changes in the number of vaccine doses administered in each site were not much affected by the COVID-19 situation. For example, a case surge in Nagasaki in July (Fig. 3), caused by a nosocomial outbreak in a large hospital, did not change the number of doses administered for most vaccines given during that period, although there was a decrease in DT vaccine doses (−25.2%) in Nagasaki in July 2020. If there had been a significant community outbreak, the situation might have been different. The dissemination of information and resources from governments and the media might have had a larger impact than local pandemic conditions on vaccination behavior. In Kawasaki and Fuchu, the decrease in childhood vaccinations occurred earlier than in the other 2 cities, possibly because the COVID-19 expansion started in the Tokyo metropolitan area.
Fig. 3.
Trends in the numbers of COVID-19 patients from March to September in 2020 in each prefecture of the 4 study sites and in Japan. Line graphs were created by using a web-based tool for COVID-19 [29] with the display range set between January 13 and September 30. The cumulative number of COVID-19 patients in Kanagawa Prefecture, where Kawasaki City is located; Niigata Prefecture, where Niigata City is located; Nagasaki Prefecture, where Nagasaki City is located; Tokyo, where Fuchu City is located; and all of Japan are shown per million general population. Abbreviations: COVID-19, coronavirus disease 2019.
Vaccine catch-up preceded the lifting of the national emergency against COVID-19 (Fig. 2). After the statement by the COIID of the JPS that routine childhood immunization is essential and urgent [21], groups and organizations such as pediatricians, medical associations, municipal offices, and the Ministry of Health, Labour and Welfare promoted vaccination catch-up campaigns. The Netherlands successfully encouraged catch-up vaccination for the first measles, mumps, and rubella vaccine, routinely scheduled at 14 months of age, although the effort was not completely successful [18]. The keys to maintaining routine childhood immunization during the COVID-19 pandemic include communication, to keep guardians informed of the continuation of vaccination services, and provision of timely vaccinations and anti–COVID-19 measures at clinics and hospitals where guardians present their children for vaccination [30].
MR2 vaccine uptake has increased since June 2020 (Fig. 2d), perhaps because of the above vaccination catch-up campaigns and an emphasis on herd immunity against measles. The number of measles cases dramatically decreased in Japan from 186 in 2017, 279 in 2018, and 744 in 2019 to only 13 in 2020 [31], most likely because of limited cross-border travel in response to the COVID-19 pandemic. International importation of the measles virus has been the main cause of the few sporadic measles outbreaks in Japan since its elimination [24], [32], [33]. Continuous attention should be paid to maintain high vaccination rates for the future recommencement of cross-border travel, because of the decrease in MR2 vaccination rates in September in Niigata and Nagasaki. A decrease was also observed in the MR1 vaccine in all 4 cities at the end of the study period (Fig. 2b).
This study has limitations that warrant mention. First, we were unable to calculate vaccination coverage rates because our data did not include the numbers of eligible vaccinees by month in each city. A nationwide electronic record system to capture vaccine doses administered and the number of eligible vaccinees is needed. Second, a sub-analysis of infants was not possible because the data on the Hib, PCV13, and DTaP-IPV vaccines did not include the number of vaccine doses administered each time. Last, we investigated only 4 cities—2 in the Tokyo metropolitan area and 2 far from Tokyo. Other areas might have different patterns of change in vaccines administered to children, especially rural areas where COVID-19 had less impact than in the 4 cities studied.
In conclusion, the COVID-19 pandemic affected routine childhood immunization in Japan. Despite the development of COVID-19 vaccines, the future effects of the pandemic are unpredictable because the duration of the effects of the new vaccines and their effectiveness against SARS-CoV-2 variants are unknown [34]. The threat to vaccination coverage might therefore continue or reemerge. A nationwide surveillance system should be established to monitor vaccine uptake using electronic records. In addition, educational activities should be provided to guardians, to encourage timely routine immunization.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
The authors are grateful to the health centers of Kawasaki City and Niigata City, the municipal office of Nagasaki City, and the Fuchu City Medical Association, which provided vaccination data. The authors are also grateful for the support of the Committee on Immunization of the Medical Association of Niigata City, the Medical Associations of Kawasaki, Nagasaki, and Fuchu, the member of the Committee on Immunization and Infectious Diseases of the Japan Pediatric Society.
Author contributions
TK, KT, HM, and AS designed the study. YA, TK, HS, and HM collected the data. YA and AS analyzed the data from the 4 cities and drafted the manuscript. TK, HS, KT, and HM critically reviewed the manuscript. All authors approved the final version of the manuscript.
Funding
This study received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.05.050.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.World Health Organization. Novel Coronavirus-China, https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/; 2020 [accessed 7 February 2021].
- 2.The Ministry of Health, Labour and Welfare. The first confirmation of a patient with pneumonia by novel coronavirus, https://www.mhlw.go.jp/stf/newpage_08906.html; 2020 [accessed 7 February 2021].
- 3.Kakuya F., Okubo H., Fujiyasu H., Wakabayashi I., Syouji M., Kinebuchi T. The first pediatric patients with coronavirus disease 2019 (COVID-19) in Japan: risk of co-infection with other respiratory viruses. Jpn J Infect Dis. 2020;73:377–380. doi: 10.7883/yoken.JJID.2020.181. [DOI] [PubMed] [Google Scholar]
- 4.Bouffet E., Challinor J., Sullivan M., Biondi A., Rodriguez-Galindo C., Pritchard-Jones K. Early advice on managing children with cancer during the COVID-19 pandemic and a call for sharing experiences. Pediatr Blood Cancer. 2020;67 doi: 10.1002/pbc.28327. [DOI] [PubMed] [Google Scholar]
- 5.Abrams E.M., Szefler S.J. Managing asthma during coronavirus disease-2019: an example for other chronic conditions in children and adolescents. J Pediatr. 2020;222:221–226. doi: 10.1016/j.jpeds.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brough H.A., Kalayci O., Sediva A., Untersmayr E., Munblit D., Rodriguez Del Rio P., et al. Managing childhood allergies and immunodeficiencies during respiratory virus epidemics - The 2020 COVID-19 pandemic: a statement from the EAACI-section on pediatrics. Pediatr Allergy Immunol. 2020;31:442–448. doi: 10.1111/pai.13262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Isba R., Edge R., Jenner R., Broughton E., Francis N., Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105:704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 8.Kadambari S., Abo Y.N., Phuong L.K., Osowicki J., Bryant P.A. Decrease in infection-related hospital admissions during COVID-19: why are parents avoiding the doctor? Pediatr Infect Dis J. 2020;39:e385–e386. doi: 10.1097/inf.0000000000002870. [DOI] [PubMed] [Google Scholar]
- 9.Gavish R., Krause I., Goldberg L., Bilavsky E., Kadmon G., Livni G., et al. A drop in number of hospitalizations among children with bacterial infections during the COVID-19 pandemic. Pediatr Infect Dis J. 2021;40:e39–e41. doi: 10.1097/inf.0000000000002963. [DOI] [PubMed] [Google Scholar]
- 10.Place R., Lee J., Howell J. Rate of pediatric appendiceal perforation at a children's hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.27948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4:e10–e11. doi: 10.1016/s2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hargreaves A.L., Nowak G., Frew P., Hinman A.R., Orenstein W.A., Mendel J., et al. Adherence to timely vaccinations in the United States. Pediatrics. 2020;145 doi: 10.1542/peds.2019-0783. [DOI] [PubMed] [Google Scholar]
- 13.O'Leary ST, Trefren L, Roth H, Moss A, Severson R, Kempe A. Number of childhood and adolescent vaccinations administered before and after the COVID-19 outbreak in Colorado. JAMA Pediatr. 2020, in press. 10.1001/jamapediatrics.2020.4733. [DOI] [PMC free article] [PubMed]
- 14.Santoli J.M., Lindley M.C., DeSilva M.B., Kharbanda E.O., Daley M.F., Galloway L., et al. Effects of the COVID-19 pandemic on routine pediatric vaccine ordering and administration - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:591–593. doi: 10.15585/mmwr.mm6919e2. [DOI] [PubMed] [Google Scholar]
- 15.Bramer C.A., Kimmins L.M., Swanson R., Kuo J., Vranesich P., Jacques-Carroll L.A., et al. Decline in child vaccination coverage during the COVID-19 pandemic - Michigan care improvement registry, May 2016-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69:630–631. doi: 10.15585/mmwr.mm6920e1. [DOI] [PubMed] [Google Scholar]
- 16.Bode S.M., Gowda C., Mangini M., Kemper A.R. COVID-19 and primary measles vaccination rates in a large primary care network. Pediatrics. 2021;147 doi: 10.1542/peds.2020-035576. [DOI] [PubMed] [Google Scholar]
- 17.McDonald H.I., Tessier E., White J.M., Woodruff M., Knowles C., Bates C., et al. Early impact of the coronavirus disease (COVID-19) pandemic and physical distancing measures on routine childhood vaccinations in England, January to April 2020. Euro Surveill. 2020;25:2000848. doi: 10.2807/1560-7917.Es.2020.25.19.2000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Middeldorp M., van Lier A., van der Maas N., Veldhuijzen I., Freudenburg W., van Sorge N.M., et al. Short term impact of the COVID-19 pandemic on incidence of vaccine preventable diseases and participation in routine infant vaccinations in the Netherlands in the period March-September 2020. Vaccine. 2021;39:1039–1043. doi: 10.1016/j.vaccine.2020.12.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhong Y., Clapham H.E., Aishworiya R., Chua Y.X., Mathews J., Ong M., et al. Childhood vaccinations: hidden impact of COVID-19 on children in Singapore. Vaccine. 2021;39:780–785. doi: 10.1016/j.vaccine.2020.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandir S., Siddiqi D.A., Mehmood M., Setayesh H., Siddique M., Mirza A., et al. Impact of COVID-19 pandemic response on uptake of routine immunizations in Sindh, Pakistan: an analysis of provincial electronic immunization registry data. Vaccine. 2020;38:7146–7155. doi: 10.1016/j.vaccine.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Committee on Immunization and Infectious Diseases, Japan Pediatric Society. Q&A on novel coronavirus infection, http://www.jpeds.or.jp/modules/activity/index.php?content_id=326; 2020 [accessed 19 February 2021].
- 22.The Committee on Immunization and Infectious Diseases of Japan Pediatric Society. Childhood vaccination during COVID-19 pandemic; Kawasaki City, Kanagawa Prefecture, http://www.jpeds.or.jp/uploads/files/20200617_yobosesshu.pdf; 2020 [accessed 7 February 2021].
- 23.Saxena S., Skirrow H., Bedford H. Routine vaccination during covid-19 pandemic response. BMJ. 2020;369 doi: 10.1136/bmj.m2392. [DOI] [PubMed] [Google Scholar]
- 24.Saitoh A., Okabe N. Progress and challenges for the Japanese immunization program: beyond the “vaccine gap”. Vaccine. 2018;36:4582–4588. doi: 10.1016/j.vaccine.2018.01.092. [DOI] [PubMed] [Google Scholar]
- 25.Niigata City, Niigata Prefecture. Population based on Residential Basic Book, https://www.city.niigata.lg.jp/smph/shisei/gaiyo/profile/00_01jinkou/kihon_nenrei/index.html; 2021 [accessed 10 February 2021].
- 26.Fuchu City, Tokyo. Population based on Residential Basic Book, https://www.city.fuchu.tokyo.jp/gyosei/toke/jyukijinko/jinko.html; 2021 [accessed 10 February 2021].
- 27.Kawasaki City, Kanagawa Prefecture. Population based on national census, https://www.city.kawasaki.jp/shisei/category/51-4-3-2-0-0-0-0-0-0.html; 2021 [accessed 12 February 2021].
- 28.Nagasaki City, Nagasaki Prefecture. Population based on national census, https://www.city.nagasaki.lg.jp/syokai/750000/752000/p023439.html; 2021 [accessed 10 February 2021].
- 29.Idogawa M., Tange S., Nakase H., Tokino T. Interactive web-based graphs of coronavirus disease 2019 cases and deaths per population by country. Clin Infect Dis. 2020;71:902–903. doi: 10.1093/cid/ciaa500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bell S., Clarke R., Paterson P., Mounier-Jack S. Parents' and guardians' views and experiences of accessing routine childhood vaccinations during the coronavirus (COVID-19) pandemic: a mixed methods study in England. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0244049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Institute of Infectious Diseases, Japan; Infectious Agents Surveillance Report. The isolation and detection of measles virus as of February 4, 2021. https://www.niid.go.jp/niid/ja/iasr-measles.html; 2021 [accessed 5 February 2021].
- 32.Kobayashi A., Shimada T., Tanaka-Taya K., Kanai M., Okuno H., Kinoshita M., et al. Epidemiology of a workplace measles outbreak dominated by modified measles cases at Kansai international airport, Japan, during august-september 2016. Vaccine. 2020;38:4996–5001. doi: 10.1016/j.vaccine.2020.05.067. [DOI] [PubMed] [Google Scholar]
- 33.Kuba Y., Kyan H., Iha Y., Kato T., Oyama M., Miyahira M., et al. Emergent measles-containing vaccination recommendation for aged 6–11 months and detection of vaccine-associated measles during a large measles outbreak in Okinawa, Japan, in 2018. Vaccine. 2020;38:2361–2367. doi: 10.1016/j.vaccine.2020.01.067. [DOI] [PubMed] [Google Scholar]
- 34.Moore JP, Offit PA. SARS-CoV-2 vaccines and the growing threat of viral variants. JAMA. 2021, in press. 10.1001/jama.2021.1114. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.