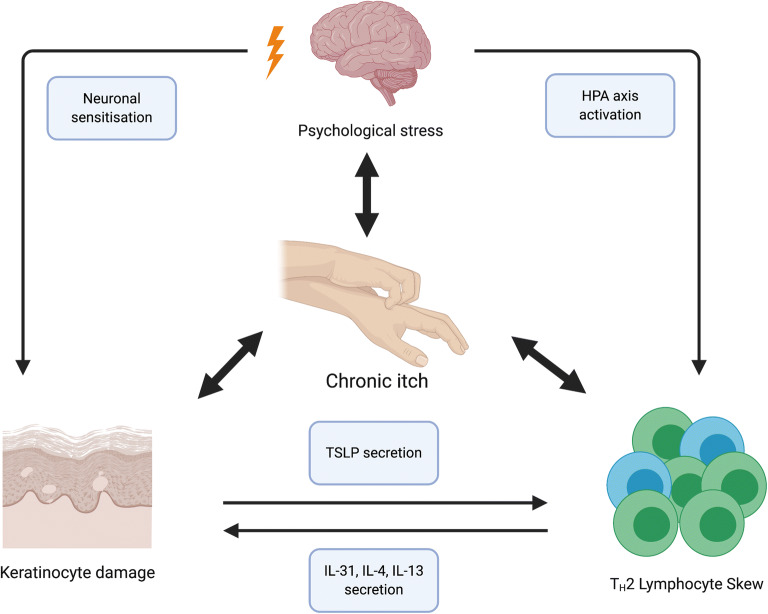
Fig. 3.
The interplay of the central nervous, immune and cutaneous systems in atopic dermatitis (AD). The multi-directional interactions of the central nervous (CNS), systemic immune systems and the AD lesional skin are complex. Psychological stress may lead to a TH2-dominant peripheral lymphocyte phenotype via activation of the hypothalamic-pituitary-adrenal (HPA) axis. Consequently, the secretion of TH2 cytokines, in particular IL-31, IL-4 and IL-13, damages cutaneous keratinocytes through persistent inflammation, leading to the secretion of thymic stromal lymphopoietin (TSLP) by keratinocytes and further expanding the TH2 population, thereby creating a feed-forward loop. The above pathways are further compounded by the key AD symptom of chronic itch. Chronic itch not only perpetuates psychological distress, often leading to its chronicity and an impact on lifestyle, but ultimately damages the keratinocytes and leads to cutaneous nervous sensitisation, whereby a minimal pruritogenic stimulus produces an excessive pruritic response