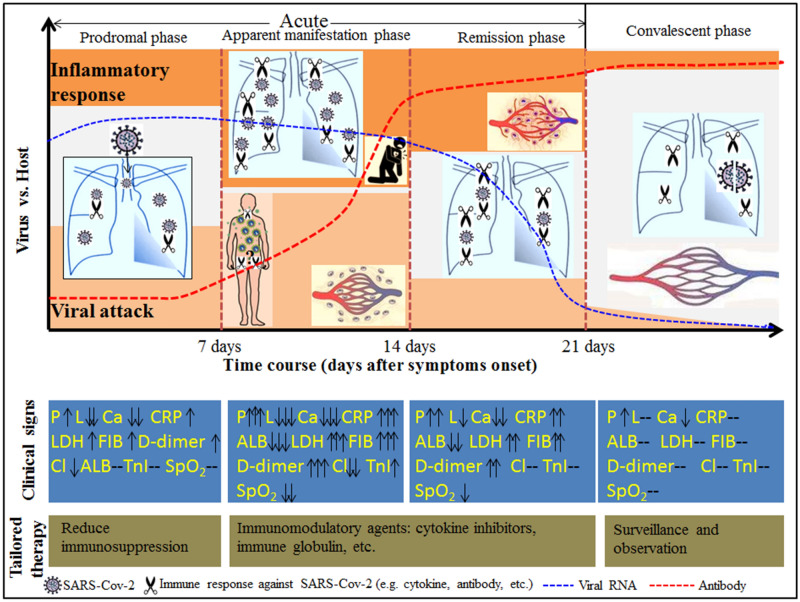
Figure 4.
Diagrammatic sketch of the clinical staging proposal of the disease course over time in non-severe patients with COVID-19. The disease course over time in non-severe patients with COVID-19 was divided into four phases: the prodromal phase (in the first week), the apparent manifestation phase (in the second week), the remission phase (in the third week), and the convalescent phase (after 3 weeks). The prodromal phase was characterized by pneumonia, lymphopenia, and slightly elevated inflammatory markers, suggesting that the infection was localized within the lung or the respiratory system. In the second week after symptoms onset, all the hematological and inflammatory markers were at the peak (bottom), indicating that an intense immune response might exist during this period. As a result of the secondary attack and the subsequent systemic inflammatory response, the disease progressed into the apparent manifestation phase. In this phase, pneumonia and other secondary organ damage (e.g. cardiac damage, coagulopathy, etc.) became apparent. After that, due to the production of effective SARS-Cov-2 antibodies, an accelerated viral clearance accompanied by a relatively high degree of inflammatory response defined the remission phase. The first three phases constituted the acute phase of COVID-19. After 3 weeks, COVID-19 patients were in the convalescent phase, in which all the indicators were maintained at a significantly low (high) level despite a positive result of SARS-Cov-2 and somewhat abnormal chest imaging. The dynamic profile of viral RNA was adapted from Lou et al.27. P pneumonia, L lymphocyte count, Ca calcium, Cl Chlorine, ALB albumin, TnI high sensitive troponin I, CRP C-reactive protein, LDH lactic dehydrogenase, FIB fibrinogen, SPO2 pulse oximeter O2 saturation.