Figure 3.
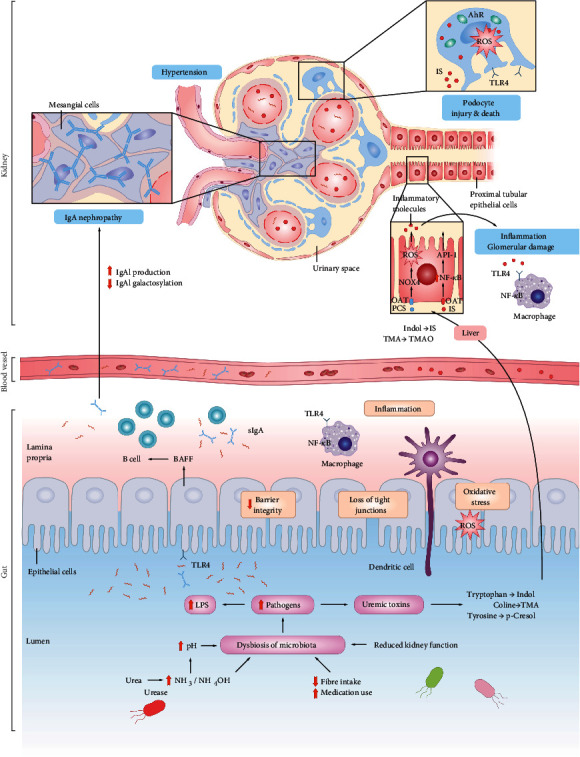
Changes in diet, numerous medication use, and decreased kidney function in CKD patients may lead to intestinal dysbiosis. The digestive tract becomes the main route for urea excretion in CKD patients with impaired renal function. A large amount of NH3 or NH4OH which are produced by bacteria can increase the intestinal pH value, promote the intestinal dysbiosis and destroy intestinal barrier. Thus, the transport of endotoxins (e.g., lipopolysaccharides (LPSs)) into the bloodstream has different effects on systemic inflammation, oxidative stress, cardiac injury, and atherosclerosis. Dysbiotic gut-derived uremic toxins, such as indoles and phenols, are further metabolized into trimethylamine N-oxide (TMAO), indoxyl sulfate (IS), and p-cresyl sulfate (PCS) in the liver and colon. The introduction of uremic toxins into the circulation causes inflammation and tubulointerstitial damage and promotes ROS production, tubulointerstitial damage, and nephrotoxicity of proximal tubuloepithelial cells. Intestinal microbial metabolites SCFAs are associated with hypertension and are important risk factors for CKD. SCFAs trigger hypertension through Olfr78, leading to renin secretion and regulation of peripheral resistance. In addition, bacteria and their components are involved in the hyperproduction and hypogalactosylation of IgA.
