Abstract
To detect, analyze, and discuss the different ear nose throat manifestations, those were reported in coronavirus disease-positive patients in the published and reviewed literature. Coronavirus disease has been reported to present with several symptoms. Common symptoms include new onset of fever, cough, fatigue, and myalgia. Other symptoms like sputum production, dyspnea, rhinorrhea, anosmia, nasal stuffiness, headache, and sore throat are less frequently reported, but the clinical presentation is highly variable among individuals. We review the otolaryngologic manifestations of coronavirus disease reported in the published literature to assess its importance in the early diagnosis of coronavirus disease. We searched PubMed database, MEDLINE, Web of Science, LILACS, SciELO, and Cochrane Library to find out relevant articles, using the following keywords: COVID-19, clinical features, characteristics, symptoms, clinical, manifestations, throat, cough, rhinorrhea, COVID-19 anosmia, headache, nasal, coronavirus, and coronavirus otolaryngologic. Article selection was based on their relevance to the research question. Totally, 14 articles and 2971 patients were recruited for our study. A wide variety of upper and lower airway manifestations were reported. Fever (34%–96.5%), cough (17.9%–83%), myalgia or fatigue (10%–31%), expectoration (20%–32.7%), dyspnea (7.6%–7.5%), rhinorrhea (1%–6.8%), sore throat (4%–61%), nasal congestion (3%–4.8%), and headache (3%–16.2%) were the most common symptoms reported. Our findings confirm that coronavirus disease infection presents with a wide spectrum of clinical presentation. The ear nose throat manifestations for coronavirus disease are not uncommon, but more attention should also be paid to patients with otolaryngologic symptoms which can appear early, as this could encourage an earlier diagnosis and treatment, which limits spread of the disease.
Keywords: Anosmia, clinical features, coronavirus, cough, COVID-19, ear nose throat, headache, manifestation, otolaryngologic, symptoms, rhinorrhea, throat
Introduction
Coronavirus is an enveloped, nonsegmented, single-stranded, positive-strand RNA virus, with round or elliptical particles that have a diameter of roughly 60–140 nm.1 They are widespread in bats across the world, and also found in many other species including other mammals, birds, and humans.1,2 In late December 2019, a series of cases with respiratory symptoms were reported in Wuhan, Hubei, China.3 After causing an outbreak in China, coronavirus disease (COVID-19) transformed into a pandemic that spread to over 213 countries, resulting in over 29 million cases and 930,000 deaths within a few months.4,5
The COVID-19 is presented mainly with lower respiratory tract-related symptoms such as fever, cough, dyspnea, and chest tightness that could progress rapidly to acute respiratory distress syndrome (ARDS).6 However, COVID-19 also causes different upper respiratory tract-related symptoms with early onset, including nasal congestion, sore throat, and smell dysfunction. The available data on the ear nose throat (ENT) manifestations of COVID-19 are not widely published, the aim of our research is to review clinical symptoms of COVID-19 among the different reviewed and previously published literature to increase clinician’s awareness of commonly seen respiratory and otolaryngologic symptoms of COVID-19. We hope this article will serve as a start for further research into the ENT implications of human COVID-19.
Method and materials
This article is a systemic review conducted via searching PubMed, MEDLINE, and Google Scholar databases for articles covering the period of January 1 to July 31, 2020, using the following keywords: clinical feature, COVID-19, COVID-19 clinical features, COVID-19 characteristics, COVID-19 symptoms, COVID-19 clinical, COVID-19 manifestations, COVID-19 throat, COVID-19 cough, COVID-19 rhinorrhea, COVID-19 anosmia, COVID-19 headache, COVID-19 nasal, coronavirus, and coronavirus otolaryngologic. Case reports, controlled studies, retrospective studies, and review articles were included. The number of articles found using the aforementioned keywords are demonstrated in Table 1. Apart from this, screening of World Health Organization (WHO) database for relevant publications on novel coronavirus (COVID-19) was screened. Some more articles were retrieved after screening the reference lists of the included studies.
Table 1.
Keywords Search.
| Keywords Search | Number of Articles in PubMed |
|---|---|
| COVID-19 | 51,693 |
| COVID-19 clinical features | 15,065 |
| COVID-19 characteristics | 24,143 |
| COVID-19 symptoms | 30,249 |
| COVID-19 clinical | 38,098 |
| COVID-19 manifestation | 3101 |
| COVID-19 throat | 5458 |
| COVID-19 cough | 11,135 |
| COVID-19 rhinorrhea | 891 |
| COVID-19 anosmia | 1653 |
| COVID-19 headache | 3795 |
| COVID-19 nasal | 8682 |
| COVID-19 anosmia | 1653 |
| COVID-19 ageusia | 714 |
| COVID-19 ENT manifestations | 120 |
| Coronavirus | 77,891 |
| Coronavirus otolaryngologic | 141 |
ENT: ear nose throat.
Statistical/data analyses used in this study
Studies across the globe—clinical case study, review, and systematic reviews analyzing the various ENT clinical presentations of COVID-19 since the outbreak started—till July 2020 were identified and studied. In our study, we focused on review of studies reporting the ENT manifestations in COVID-19-positive patients. Then, the data were collected, tabulated in an Excel sheet, and analyzed as per the results of the studies that met our inclusion and exclusion criteria. Randomized controlled studies, observational studies, comparative studies, case series, and case reports were evaluated for the eligibility. Statistical analysis was performed with SPSS 17 for Windows Paired-sample t-test was used to evaluate the differences in the same group before and after treatment in quantitative voice assessment.
The percentages of patients who presented with respiratory (cough, dyspnea, and sputum) and otolaryngologic (fever, sore throat, nasal rhinorrhea/congestion, anosmia/hyposmia, headache, and dizziness) manifestations were collected and summarized. This review article presents a baseline from where further prospective studies for smell and taste disturbances in COVID-19 patients could be designed and helps as a spur for further research in this clinical symptom.
The abstracts of articles from PubMed and MEDLINE were read to select relevant articles, whereas article selection from Google Scholar was based on titles only.
The inclusion criteria for our study are:
Articles published till July 2020 included in the study.
Articles written in English or Chinese language translated to English.
Articles including patients with a confirmed diagnosis of COVID-19 who presented with respiratory or otolaryngologic clinical features.
Articles included in the study, with a mean age from 6.8 to 55.5 years.
Filtering of articles based on abstract and title was done and duplicates were removed
The exclusion criteria for our study are:
Studies pertaining to other coronavirus-related illnesses, such as Middle East respiratory syndrome (MERS).
Articles published after July 2020 are excluded from the study.
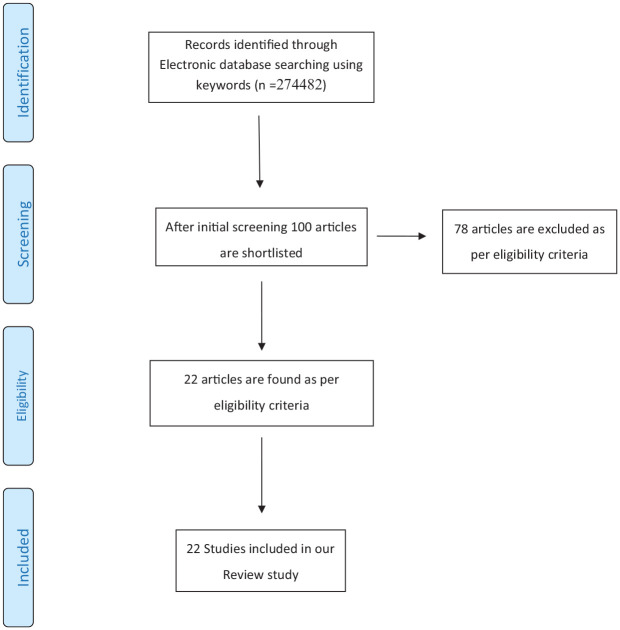
PRISMA Flow Diagram.
Result
A total of 274,482 records are electronically searched. The number of results found on searching each keyword are depicted in Table 1. After initial screening, around 100 articles were shortlisted; finally, with our inclusion/exclusion criteria, 22 studies fulfilled the eligibility for this research. A total of 5930 patients from this study are included for review in our study.
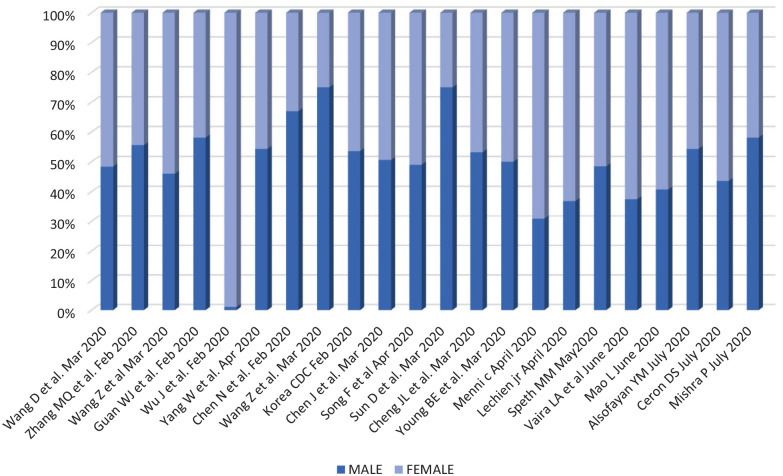
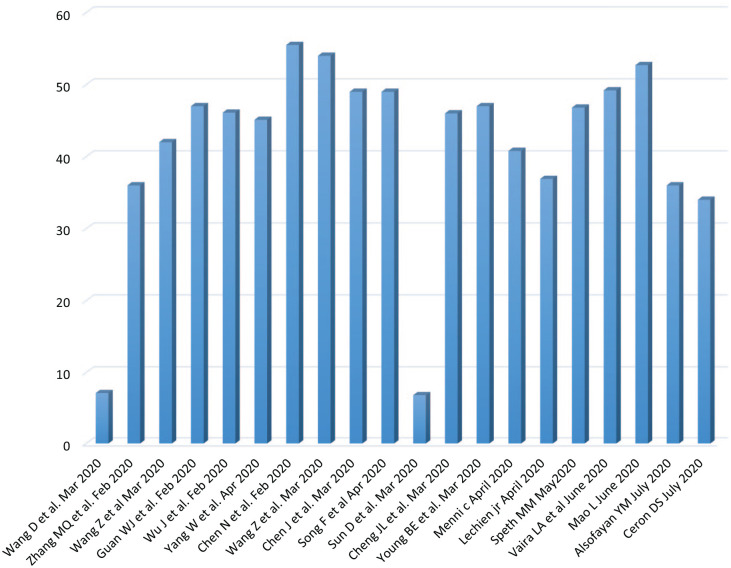
Out of 22 studies, 12 studies have male predominance (ranging from 30.90% to 75%) and females are predominant in nine studies (ranging from 25% to 69.10%), and in one study, the ratio is 1:1 (Figure 1). Median age is different for the pediatric and adult groups; for the pediatric group (two studies), it is 6.8 and 7.1 years, respectively, whereas for the adult group, the median age is between 34 and 55.5 years (20 studies) (Figures 2 and 3).
Figure 1.
Male-to-female ratio in different studies.
Figure 2.
Median age of patients under study.
Figure 3.
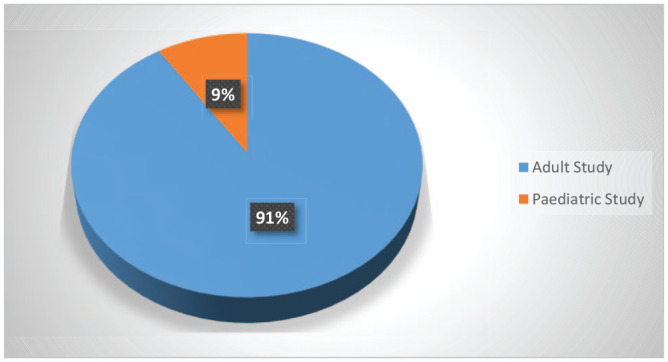
Source of data.
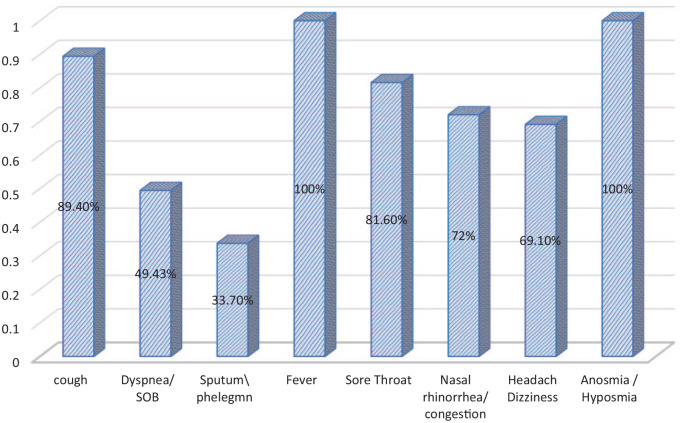
Fever was the most common reported symptom (29.10%–100%), followed by cough (17.9%–89.40%) (Table 2). Other respiratory symptoms included expectoration (17.9%–33.7%), and shortness of breath/dyspnea (2.10%–49.43%). Otolaryngologic symptoms were less common than respiratory symptoms. Among this, sore throat was the most common otolaryngologic manifestation (4%–81.60%) (Figure 1) followed by rhinorrhea/nasal congestion (3.36%–72%) and headache (3.5%–69.1%) of patients. Anosmia/hyposmia is not reported in the initial COVID-19 studies, but latest studies show that it is one of the most common symptoms (5%–100%). Figure 4 shows maximally reported percentage of symptoms in different studies.
Table 2.
Respiratory and otolaryngology manifestations of COVID-19.
| S. no. | Study authors (year) | Patients no. | Respiratory manifestation | Otolaryngologic manifestation | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male (%) | Female (%) | Mean age (Years) | Cough (%) | Dyspnea/SOB (%) | Sputum/Phlegm (%) | Fever (%) | Sore throat (%) | Nasal rhinorrhea/congestion (%) | Headache/dizziness (%) | Anosmia/hyposmia (%) | |||
| 1. | Wang et al. 20207 | 31 | 48.4 | 51.6 | 7.1 | 45 | 65 | 6 | 6 | 10 | |||
| 2 | Zhang et al. 20208 | 9 | 55.5 | 44.4 | 36 | 55.5 | 88.9 | 44.4 | 55.5 | ||||
| 3 | Wang et al. 20209 | 69 | 46 | 54 | 42 | 55 | 29 | 29 | 87 | 9 | 14 | ||
| 4 | Guan et al. 202010 | 1099 | 58.1 | 41.9 | 47 | 67.8 | 18.7 | 33.7 | 88.7 | 13.9 | 4.8 | 13.6 | |
| 5 | Wu et al. 202011 | 80 | 51.2 | 48.8 | 46.1 | 63.75 | 37.5 | 78.75 | 13.75 | 6.10 | 16.25 | ||
| 6 | Yang et al. 202012 | 149 | 54.3 | 45.7 | 45.1 | 58.39 | 10.74 | 32.2 | 76.51 | 14.09 | 3.36 | 8.72 | |
| 7 | Chen et al. 202013 | 99 | 67 | 33 | 55.5 | 82 | 31 | 82 | 5 | 8 | |||
| 8 | Wang et al. 202014 | 4 | 75 | 25 | 54 | 75 | 100 | 50 | 50 | ||||
| 9 | Korea CDC 202015 | 28 | 53.6 | 46.4 | 17.9 | 17.9 | 32.1 | 32.1 | 10.7 | ||||
| 10 | Chen et al. 202016 | 249 | 50.6 | 49.4 | 49 | 36.5 | 7.6 | 87.1 | 6.4 | 6.8 | 11.2 | ||
| 11 | Song et al 202017 | 51 | 49 | 51 | 49 | 47 | 14 | 20 | 96 | 6 | 4 | 16 | |
| 12 | Sun et al. 202018 | 8 | 75 | 25 | 6.8 | 75 | |||||||
| 13 | Cheng et al. 202019 | 1077 | 53.2 | 46.8 | 46 | 18.2 | 91.4 | 4 | 3.5 | 3.5 | |||
| 14 | Young et al. 202020 | 18 | 50 | 50 | 47 | 83 | 11 | 72 | 61 | 6 | |||
| 15 | Menni 202021 | 579 | 30.9 | 69.1 | 40.79 | 58.03 | 49.43 | 31.61 | 59 | ||||
| 16 | Lechien 202022 | 417 | 36.9 | 63.1 | 36.9 | 79 | 27.5 | 49 | 30 | 37 | 85.6 | ||
| 17 | Speth 202023 | 103 | 48.5 | 51.5 | 46.8 | 68 | 46.6 | 74.8 | 49 | 61 | |||
| 18 | Vaira et al. 202024 | 72 | 37.5 | 62.5 | 49.2 | 83.3 | 95.8 | 51.4 | 15.3 | 41.6 | 60 | ||
| 19 | Mao et al. 202025 | 214 | 40.7 | 59.3 | 52.7 | 50 | 61.7 | 14.5 | — | 13.1 | 5 | ||
| 20 | Alsofayan et al. 202026 | 1519 | 54.3 | 45.7 | 36 | 89.4 | 85.6 | 81.6 | 72 | 27.3 | |||
| 21 | Ceron et al. 202027 | 55 | 43.6 | 56.4 | 34 | 40 | 2.1 | 29.1 | 40 | 69.1 | 100 | ||
| 22 | Mishra et al. 202028 | 74 | 58.1 | 41.9 | 14.8 | ||||||||
CDC: Centers for Disease Control and Prevention.
Figure 4.
Maximally reported percentage of symptoms in different studies.
Sneezing, epistaxis, postnasal discharge, facial edema or tenderness, diminution of hearing, ear pain, vertigo, hoarseness, or stridor were not described in the recruited studies.
Discussion
Symptomatology of COVID-19 is diverse; clinically, it ranges from asymptomatic to mild upper respiratory tract infection (URTI)-like symptoms to ARDS to multiorgan dysfunction.6 Most common symptoms include fever, cough, sore throat, headache, fatigue, myalgia, and breathlessness,1,2,29 due to which COVID-19 infection become indistinguishable from other upper respiratory infections.
The main aim of the current research was to review the initial clinical presentations of COVID-19 infection among patients, as reported in the literature in different studies. Results from our review showed that fever was the most common presenting symptom of COVID-19 infection. Up to 100% of patients in the recruited studies had a fever.14 Cough, expectoration, and dyspnea were the next common respiratory symptoms in different studies in our review. Otolaryngologic symptoms were less commonly reported in the initial presentation of COVID-19 infection. Sore throat was the most common otolaryngologic symptom of COVID-19 infection, followed by nasal discharge, headache, and anosmia. Our results were consistent with other literature studies that described the full symptoms spectrum of COVID-19.2,30 In these studies, fever was the most common symptom, reported to affect up to 92.8% of patients, followed by cough (69.8%), dyspnea (34.5%), myalgia (27.7%), headache (7.2%), and diarrhea (6.1%).2,30 Rhinorrhea was noted in only 4%, and sore throat in 5.1% of patients with relevant clinical information.2,30
The pathophysiology of COVID-19 explains the prevalence of respiratory symptoms. COVID-19 spreads most commonly through the respiratory tract by upper airway secretions, droplets, and direct/indirect contact.17,20,29 Nasal, nasopharyngeal, and/or oropharyngeal area was one of the main harbor sites of the infection, main sites of taking the sample for testing, and a main source of transmission of infection. However, most published COVID-19 studies are focused on the lower respiratory tract manifestation and sequels due to their life-threatening nature and ignoring the importance of these otolaryngological symptoms for early diagnosis and treatment of disease.
Studies like a multicenter retrospective study done in Saudi Arabia26 show that fever and cough were common symptoms followed by sore throat and rhinorrhea.
The multicenter Coranosmia cohort study27 shows that anosmia (100%), followed by headache (69.1%), rhinorrhea/nasal obstruction (40%), and cough (40%) were the most common symptoms. This study also shows the importance of ENT symptoms for the diagnosis of COVID-19.27
In recent studies, sudden asymptomatic anosmia has been reported in the initial presentation of COVID-19 infection.31 The precise etiology of this syndrome remains undetermined.31 Two explanations were proposed:
“conductive” loss due to the mucosal obstruction of the olfactory cleft, leading to loss of smell; and
“neural” loss due to post viral anosmia syndrome with direct infection of the olfactory mucosa and destruction of the olfactory sensory neurons.31
Another study shows a 14.8% prevalence of new-onset anosmia in the Indian population with COVID-19.28
Post viral anosmia was one of the important reasons of smell dysfunction in adults (40% of cases of anosmia). Viruses that cause common cold or upper respiratory tract infections are well known to be associated with postinfectious smell loss. The previously described coronaviruses, accounts for 10%–15% cases.32 Therefore, the novel COVID-19 virus is supposed also to be able to cause anosmia in infected patients, and if it occurs, it will not be a specific finding.
There is very little mentioned in the literature about smell and taste dysfunctions in COVID-19 patients, and also there is still a paucity of peer-reviewed literature to support a causal association between anosmia and COVID-19.33 Moreover, most studies on smell in COVID-19 patients did not fully describe the clinical manifestations of the patients, so more research required to prove their relationship.
Menni et al.21 found that loss of smell and taste were presented in 59% of COVID-19-positive patients, compared to 18% of those with a COVID-19-negative test. They suggested that a combination of loss of smell and taste, fever, persistent cough, fatigue, and GIT symptoms is predictive of COVID-19-positive test with good specificity (0.86) and average sensitivity (0.54). But they do not know whether anosmia was developed prior to other COVID-19 symptoms, during the illness or afterward.
Lechien et al.22 in their peer-reviewed multicenter study reported 85.6% olfactory dysfunction. They used a questionnaire focused on the psychological and social burden of smell disorders, particularly with the COVID-19 pandemic scenario, and the subsequent social life restrictions might lead to overestimation.34
Kaye et al.35 report on 237 patients with COVID-19 and found that anosmia was noted in 73% of patients prior to COVID-19 diagnosis and was the initial symptom in 26.6%. It was found that many patients with anosmia without nasal obstruction or runny nose are positive for COVID-19, so it is recommended that these patients should be considered as COVID-19 suspicious and early COVID-19 testing and/or self-isolation for them.35
Mao et al.25 study revealed anosmia in 5.1% of their studied cases.
Data from this literature review show that COVID-19 infection had a wide spectrum of clinical presentation. Thus, strict medical observation for all patients with suspected disease is highly recommended, until the results of nucleic acid amplification tests (reverse transcription polymerase chain reaction (RT-PCR)) from nasopharynx swab, throat swab, sputum, and even lung lavage are obtained. All the reported ENT manifestations in COVID-19 patients are nonspecific and so could be easily missed. Patients with COVID-19 have no emergency ENT symptoms such as bleeding per nose, but throat or stridor was reported. No laryngeal manifestations were documented.36 No reported sneezing or postnasal discharge. Therefore, in line with the above statement, it is important to inform our ENT colleagues about paying attention that anosmia and dysgeusia can be the sole presenting feature that can be manifested early in the course of the disease. Although these patients have a mild form of the disease, they are potential carriers and can add to the burden of disease transmission. Therefore, we suggest that these symptoms should be considered highly susceptible to COVID-19 and should be included during the screening of patients.
Auditory manifestation was not reported in the studies on COVID-19 and auditory complication due to coronavirus is little mentioned in the literature. In a previous report on other coronavirus infection,37 brainstem involvement was observed and the neuroauditory problem is possible. While in the study of Mustafa,38 COVID-19 infection could have deleterious effects on cochlear hair cell functions despite being asymptomatic as the reduction of high-frequency pure-tone thresholds as well as the TEOAE amplitudes were detected.
Waheed El-Anwar36 in his study reported that ENT manifestations in COVID-19 patients are not common as fever and cough. He emphasized that there is a need of a universal questionnaire using well-defined COVID-19 manifestations to make the COVID-19 data precisely defined, complete, and homogeneous.
While the literature on ENT manifestation during COVID-19 infection is still sparse, it is important to study ENT manifestations of such novel virus and defining ENT epidemiological and clinical characteristics. In the current review of literature, we tried to collect the data of patients with ENT manifestations in the laboratory-confirmed COVID-19 cases in only the peer-reviewed and published articles, to provide a recent delineation of the otorhinolaryngology (ORL), clinical characteristics of COVID-19 patients, to help ENT doctors to understand the disease and approach such cases and also to assist them in building up the ENT data for the disease.
Limitations
Data collection and analysis are difficult in the era of serious health emergency of COVID-19. Thus, our current study shares the following limitations that usually met during the studies on the novel virus COVID-19:
First, most articles not reported/missed asymptomatic or mild cases managed at home, without availing health facilities.
Second, the COVID-19 diagnosis is based on the RT-PCR test, which is not 100% sensitive. Also, improper collection, storage, and transportation of sample may decrease test sensitivity.
Third, variation in the methods, source, and structure of clinical data collection rapidly from time to time, person to person, from a country to another, from a study to another. Also, presently, there is no specific universal questioner for those patients by healthcare provider.
Fourth, incomplete documentation of the symp-toms without a precise definition of the clinical manifestations.
Fifth, studies till the month of July are included in this review article.
Sixth, there is no available data on the sequential appearance of the ENT manifestation or clear definition of the COVID-19 manifestation.
All these limitations are present in published research articles on COVID-19 till now and should be considered in future studies.
Conclusion
ENT manifestations are not common as fever and cough in COVID-19, but increasingly more attention should be paid to patients with otolaryngologic symptoms that appear early, as this could encourage an earlier diagnosis, resulting in nonpharmacological strategies to achieve better prevention of respiratory viral infections. Also, by early diagnosis of disease, silent carriers can be reduced which helps us to break the chain of virus transmission and prevent community spread of this infection. We hope our article will serve as a start for further research into the ENT implications of human COVID-19.
Supplemental Material
Supplemental material, sj-doc-1-smo-10.1177_20503121211016965 for Upper respiratory tract and otolaryngological manifestations of coronavirus disease 2019 (COVID-19): A systemic review by Jamil N Al-Swiahb and Mohammed A Motiwala in SAGE Open Medicine
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Jamil N Al-Swiahb  https://orcid.org/0000-0002-6997-1548
https://orcid.org/0000-0002-6997-1548
Supplemental material: Supplemental material for this article is available online.
References
- 1. Cascella M, Rajnik M, Cuomo A, et al. Features, evaluation and treatment coronavirus (COVID-19). Statpearls 2020. [Internet]. http://www.ncbi.nlm.nih.gov/pubmed/32150360 [PubMed]
- 2. Lai CC, Shih TP, Ko WC, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020; 55(3): 105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. NHC. National Health Commission of the People’s Republic of China main, 2019. [Internet]. http://en.nhc.gov.cn/ (accessed 20 January 2020). [DOI] [PMC free article] [PubMed]
- 4. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak: an update on the status. Milit Med Res 2020; 137(1): 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. https://www.who.int/emergencies/diseases/novel-coronavirus-2019?gclid=CjwKCAjw74b7BRA_EiwAF8yHFHpecCFO_QTu_a21V39_LPCrLWLTt1aRaZmp_w1ewu5Qm2XsVN0T_RoCt00QAvD_BwE
- 6. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis 2020; 34: 101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wang D, Ju XL, Xie F, et al. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of northern China. Zhonghua Er Ke Za Zhi 2020; 58(4): 269–274. [DOI] [PubMed] [Google Scholar]
- 8. Zhang MQ, Wang XH, Chen YL, et al. Clinical features of 2019 novel coronavirus pneumonia in the early stage from a fever clinic in Beijing. Zhonghua Jie He He Hu Xi Za Zhi 2020; 43: E013. [DOI] [PubMed] [Google Scholar]
- 9. Wang Z, Yang B, Li Q, et al. Clinical features of 69 cases with Coronavirus disease 2019 in Wuhan, China. Clin Infect Di 2020; 71(15): 769–777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med 2020; 382(18): 1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu Province: a multicenter descriptive study. Clin Infect Dis 2020; 71(15): 706–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect 2020; 80(4): 388–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395(10223): 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wang Z, Chen X, Lu Y, et al. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci Trends Adv Pub 2020; 14(1): 64–68. [DOI] [PubMed] [Google Scholar]
- 15. COVID-19 National Emergency Response Center Epidemiology and Case Management Team Korea Centers for Disease Control and Prevention. Early epidemiological and clinical characteristics of 28 cases of coronavirus disease in South Korea. Osong Public Health Res Perspect 2020; 11(1): 8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chen J, Qi T, Liu L, et al. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect 2020; 80(5): e1–e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Song F, Shi N, Shan F, et al. Emerging 2019 novel coronavirus (2019-NCoV) pneumonia. Radiology 2020; 295(1): 210–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sun D, Li H, Lu XX, et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J Pediatr 2020; 16(3): 251–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cheng JL, Huang C, Zhang GJ, et al. Epidemiological characteristics of novel coronavirus pneumonia in Henan. Zhonghua Jie He He Hu Xi Za Zhi 2020; 43(4): 327–331. [DOI] [PubMed] [Google Scholar]
- 20. Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 2020; 323(15): 1488–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Menni C, Valdes A, Freydin MB, et al. Loss of smell and taste in combination with other symptoms is a strong predictor of COVID-19 infection. Medrxiv 2020. https://www.medrxiv.org/content/10.1101/2020.04.05.20048421v1#:~:text=We%20also%20find%20that%20a,and%20cross%2Dvalidation%20ROC%2DAUC
- 22. Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020; 277(8): 2251–2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Speth MM, Singer-Cornelius T, Oberle M, et al. Olfactory dysfunction and sinonasal symptomatology in COVID-19: prevalence, severity, timing, and associated characteristics. Otolaryngol Head Neck Surg 2020; 163(1): 114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vaira LA, Deiana G, Fois AG, et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: single-center experience on 72 cases. Head Neck 2020; 42(6): 1252–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mao L, Jin H, Wang M, et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol 2020; 77(6): 683–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alsofayan YM, Althunayyan SM, Khan AA, et al. Clinical characteristics of COVID-19 in Saudi Arabia: a national retrospective study. J Infect Public Health 2020; 13(7): 920–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ceron DS, Bartier S, Hautefort C, et al. Self-reported loss of smell without nasal obstruction to identify COVID-19. The multicenter Coranosmia cohort study, Elsevier Public Health Emergency Collection. J Infect 2020; 81(4): 614–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mishra P, Gowda V, Dixit S, et al. Prevalence of new onset anosmia in COVID-19 patients: is the trend different between European and Indian population? Indian J Otolaryngol Head Neck Surg 2020; 72(4): 484–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Moriyama M, Hugentobler WJ, Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol 2020; 7(1): 83–101. [DOI] [PubMed] [Google Scholar]
- 30. Tian S, Hu N, Lou J, et al. Characteristics of COVID-19 infection in Beijing. J Infect 2020; 80(4): 401–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gane SB, Kelly C, Hopkins C. Isolated sudden onset anosmia in COVID-19 infection. A novel syndrome? Rhinology 2020; 58(3): 299–301. [DOI] [PubMed] [Google Scholar]
- 32. Dubé M, Le Coupanec A, Wong AH, et al. Axonal transport enables neuron-to-neuron propagation of human coronavirus OC43. J Virol 2018; 92(17): e00404–e00418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hopkins C, Surda P, Whitehead E, et al. Early recovery following new onset anosmia during the COVID—19 pandemic —an observational cohort study. J Otolaryngol Head Neck Surg 2020; 49: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Passali GC, Bentivoglio AR. Comment to the article “Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020; 277(8): 2391–2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kaye R, Chang CD, Kazahaya K, et al. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg 2020; 163(1): 132–134. [DOI] [PubMed] [Google Scholar]
- 36. El-Anwar MW, Elzayat S, Fouad YA. ENT manifestation in COVID-19 patients. Auris Nasus Larynx 2020; 47: 559–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wege H, Watanabe R, ter Meulen V. Relapsing subacute demyelinating encephalomyelitis in rats during the course of coronavirus JHM infection. J Neuroimmunol 1984; 6(5): 325–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mustafa MWM. Audiological profile of asymptomatic Covid-19 PCR-positive cases. Am J Otolaryngol 2020; 41(3): 102483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395(10223): 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-smo-10.1177_20503121211016965 for Upper respiratory tract and otolaryngological manifestations of coronavirus disease 2019 (COVID-19): A systemic review by Jamil N Al-Swiahb and Mohammed A Motiwala in SAGE Open Medicine