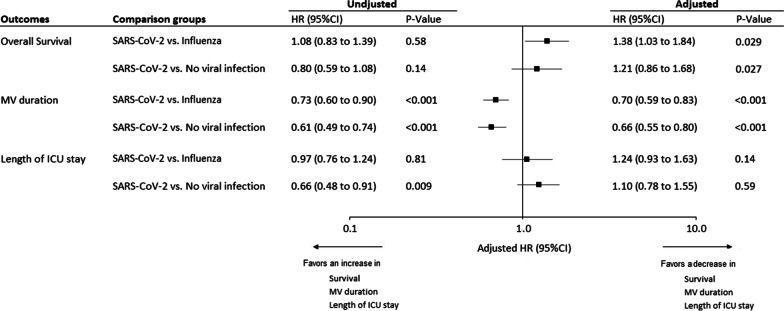
Fig. 1.
Unadjusted and Adjusted hazard ratios for 28-day mortality, extubation alive and ICU discharge alive, associated with SARS-CoV-2 pneumonia, versus influenza pneumonia and no viral infection groups. HRs were calculated using cause-specific proportional hazard models, by considering mortality as competing event for MV duration, and length of ICU stay. Adjusted HRs were calculated, including age, gender, simplified acute physiology score II, Charlson score, MacCabe classification, shock, and acute respiratory distress syndrome as pre-specified covariates in Cox’s models (after handling missing values by multiple imputation). A HR > 1 indicates a decrease in survival duration (i.e. an increased risk for mortality), MV duration (i.e. an increased risk for extubation alive) and ICU length of stay (i.e. an increased risk for discharge alive) and a HR < 1 indicates an increase in survival duration (i.e. a decreased risk for mortality), MV duration (i.e. a decreased risk for extubation alive) and ICU length of stay (i.e. a decreased risk for discharge alive). Note that the event of interest for survival is a pejorative event (death) whereas for MV duration and ICU length of stay, the event of interest is a positive event (extubation or discharge alive). Consequently, the detrimental effect of SARS-CoV-2 pneumonia (vs influenza pneumonia and no viral infection groups) was associated with a HR > 1 for overall survival but was associated with a HR < 1 for MV duration and ICU length of stay. HR, hazard ratio; ICU, intensive care unit; MV, mechanical ventilation