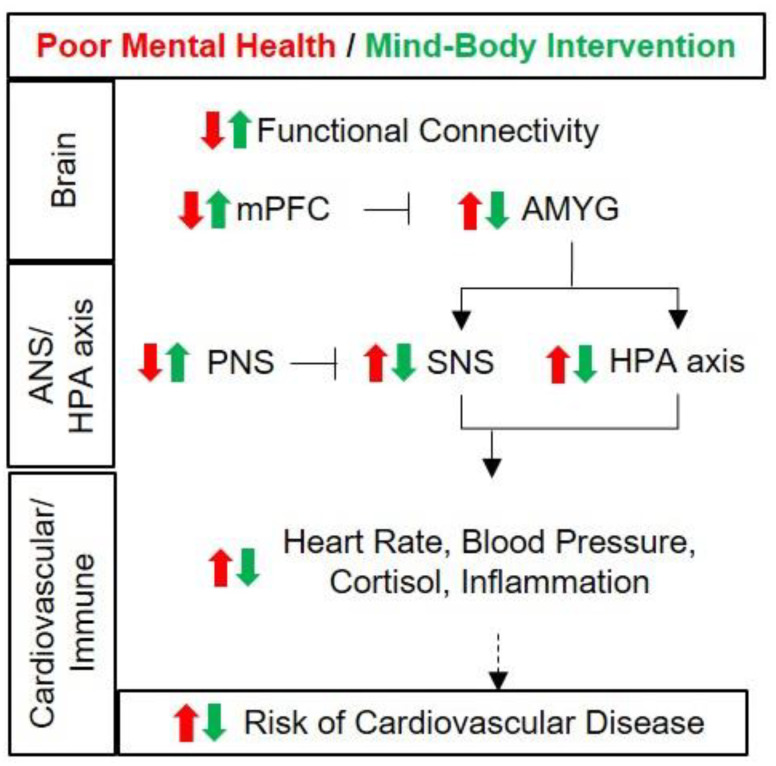
Figure 1.
Potential mechanism of reduction in cardiovascular disease risks by mind–body intervention in women. Unlike in men, significant associations between amygdala activity and physiological responses have been reported specifically in women [72,73,74,75]. Poor mental health (red), such as chronic persistence of depression and stress, reduces functional connectivity between the prefrontal cortex and the amygdala, decreases activity of the medial prefrontal cortex and increases activity of the amygdala, which is controlled by the prefrontal cortex. Subsequently, the sympathetic nervous system is activated to increase the heart rate and blood pressure, while the HPA axis is activated to increase cortisol secretion, and the chronic activation of these states induces inflammation. The above states represent increased risks for cardiovascular disease. On the other hand, the application of mind–body intervention (green) helps improve mental health by reducing perceived stress and depression. The functional connectivity between the prefrontal cortex and the amygdala increases, and the activity of the medial frontal cortex also increases, thereby reducing the activity of the amygdala. Mind–body intervention activates the parasympathetic nervous system, thereby reducing sympathetic nerve activity, as well as reducing HPA axial activity as stress decreases. As a result, heart rate, blood pressure and cortisol secretion are reduced and inflammatory conditions are reduced. These states mean a reduction in cardiovascular disease risk. AMYG, amygdala; mPFC, medial prefrontal cortex; SNS, sympathetic nervous system; HPA, hypothalamus–pituitary–adrenal cortex.