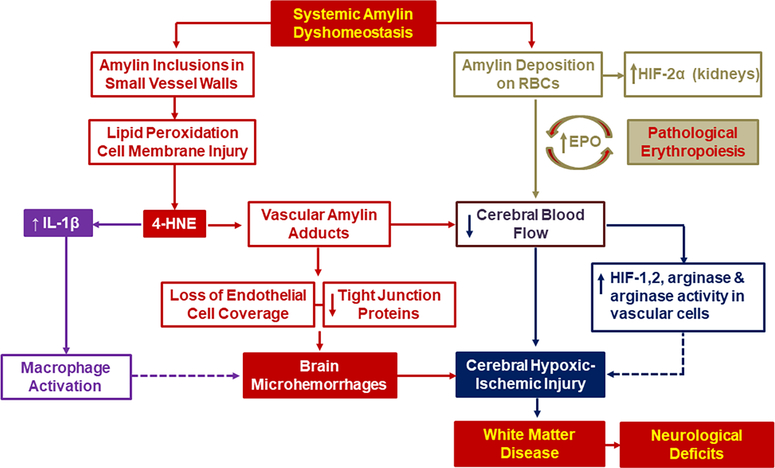
Figure 1. The amylin dyshomeostasis hypothesis of small vessel-type ischemic stroke in the setting of type-2 diabetes mellitus.
Systemic amylin dyshomeostasis is characterized by accumulation of aggregated amylin in blood and microvasculature, brain microhemorrhages and reduced cerebral blood flow leading to white matter injury and neurological deficits. At the cellular level, amylin inclusions in vascular walls generate reactive aldehydes such as 4-hydroxinonenal (4-HNE) and vascular amylin adducts causing loss of endothelial cell coverage and downregulation of tight junction proteins (red code pathway). Increased 4-HNE levels activates pro-inflammatory IL-1β signaling pathways leading to macrophage activation and macrophage infiltration in vascular areas positive for amylin deposition (magenta code pathway). In addition, amylin-coated RBCs directly activate hypoxia signaling (green code pathway), have increased adhesion to vascular endothelial cells and tendency to aggregate exacerbate the risk of small vessel-type ischemic stroke (navy code pathway).