Abstract
Dopamine is a neurotransmitter that mediates neuropsychological functions of the central nervous system (CNS). Recent studies have shown the modulatory effect of dopamine on the cells of innate and adaptive immune systems, including Th17 cells, which play a critical role in inflammatory diseases of the CNS. This article reviews the literature data on the role of dopamine in the regulation of neuroinflammation in multiple sclerosis (MS). The influence of dopaminergic receptor targeting on experimental autoimmune encephalomyelitis (EAE) and MS pathogenesis, as well as the therapeutic potential of dopaminergic drugs as add-on pathogenetic therapy of MS, is discussed.
Keywords: dopamine, Th17 cells, neuroinflammation, psychoneuroimmunology, multiple sclerosis
1. Introduction
Multiple sclerosis (MS) is the most common demyelinating disease of the central nervous system [1]. Despite the progress made in recent years in the development of new methods of MS therapy, the treatment of MS patients remains one of the main problems of clinical neurology. The existing highly effective targeted therapy can reduce the activity of the disease [2]. At the same time, the treatment with second- or third-line disease-modifying drugs is associated with severe side effects because of the immunosuppressive impact of such therapy [3,4]. It is important to note that the ingress of the monoclonal antibodies in the CNS could be limited by the blood–brain barrier [5]. Therefore, they cannot directly affect the immune response in the CNS, while the neuroinflammation seems to proceed at least partially independently of immune processes in the periphery [6].
In this regard, the modulation of immune cell functions in the CNS, without affecting peripheral immune response, is considered a promising direction of pathogenetic therapy of CNS autoimmune diseases. Biogenic amines, such as serotonin, dopamine, norepinephrine, and epinephrine, are direct mediators of neuroimmune interaction. The studies in recent decades have shown that neurotransmitters regulate not only CNS functions but also have immunomodulatory effects. Cells in both the innate and adaptive immune systems have been found to express dopamine, norepinephrine, and serotonin receptors and produce biogenic amines. In addition, autocrine regulatory effects of dopamine on immune cells were demonstrated [7]. The data on the influence of dopamine, norepinephrine, and serotonin on experimental autoimmune encephalomyelitis (EAE) and MS course allow one to propose the therapeutic prospective of their receptor targeting in MS [7,8,9,10].
In this brief report, we overview the literature and own data on dopamine’s role in the regulation of neuroimmune interaction in EAE and MS. The therapeutic potential of dopaminergic receptor targeting in MS is discussed.
2. The Involvement of Dopamine in the Development of Clinical Symptoms in MS
Among the neurotransmitters involved in the regulation of neuroimmune interaction in MS, dopamine is one of the most well studied. Dopamine is most widely represented in the brain and modulates different CNS functions. The involvement of dopamine in depression, cognitive impairments, and fatigue in MS was shown [11,12,13,14]. In addition, dopamine has been shown to modulate the gut–brain axis, which plays an important role in the development of autoimmunity, psychiatric disorders, and neuroinflammation [15,16,17]. It is important to note that depression is one of the most common symptoms in MS and may aggravate its course, which could be explained by similar pathogenetic mechanisms of MS and depression, including an enhanced Th17 immune response [18,19]. Conversely, the clinical efficacy of “controlled stress” therapies, such as treatment with antidepressants, lifestyle modification, and coping strategies in MS, was shown [10,20,21].
It can be assumed that other neuropsychological symptoms of MS, such as cognitive impairment and fatigue, may also aggravate MS course [11,12,22]. Thus, Alvarenga-Filho et al. reported that plasma levels of IL-6 and TNF-α were higher in relapsing–remitting MS patients with fatigue than in the control group (relapsing–remitting MS patients without fatigue) [22]. They also found a positive association between IL-6 and TNF-α concentrations and fatigue severity. The cytokine production by anti-CD3/anti-CD28-stimulated PBMCs (IL-6, TNF-α, IFN-γ, IL-17, IL-22, and GM-CSF), as well as CD4+ and CD8+ T cells (IL-17 and IFN-γ), was higher in MS patients with fatigue [22]. The production of Th17 cell differentiation cytokines IL-6, TNF-α, IL-1β, and IL-23 by LPS-activated monocytes also was higher in MS patients with fatigue. Again, they found a correlation between the severity of fatigue and TNF-α, IL-6, IL-17, IL-22, and GM-CSF production by stimulated T cells and IL-6, IL-1β, and IL-23 production by LPS-activated monocytes [22]. At the same time, combined exercise training reduces fatigue severity, pro-inflammatory cytokine production and regulates dopamine-mediated immunomodulation of T cells in relapsing–remitting MS patients [23].
On the other hand, secondary dysregulation of catecholamines in MS due to neuroinflammation and structural damage of catecholamine-dependent pathways within the brain was shown [18,24,25]. In particular, Carandini et al. showed that axonal damage imbalances dopamine and norepinephrine neurotransmission in relapsing–remitting MS patients [18]. They also showed a central role of the dopamine mesocorticolimbic pathway in fatigue in MS [18]. Carotenuto et al. reported the altered functional connectivity in the dopaminergic network in MS patients compared to healthy subjects [25].
Although the concentration of biogenic amines in peripheral blood is not stable and can depend on the different factors, the change of dopamine plasma level in MS was also reported. It was shown that the plasma dopamine level in relapsing–remitting MS patients during relapse was lower than in MS patients during clinical remission or in healthy subjects [26]. Escribano et al. also showed the decreased level of dopamine in patients with MS [27].
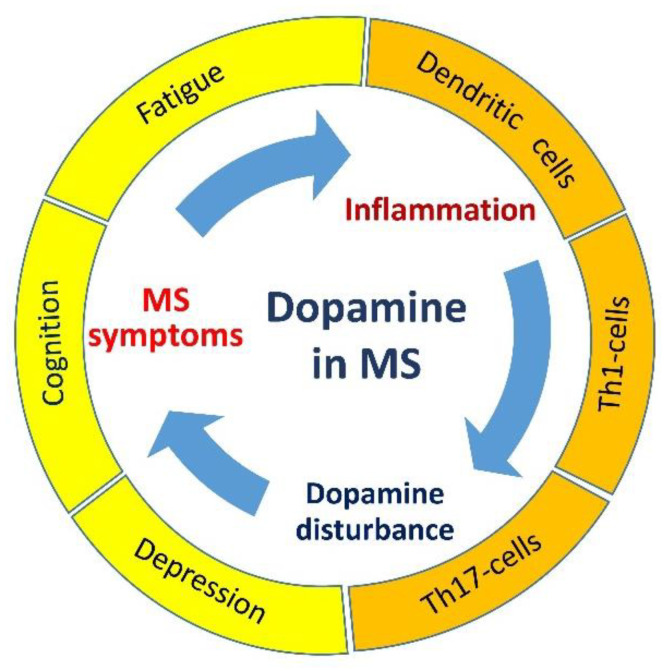
Thus, dopaminergic system disturbance may affect MS pathogenesis by the influence on neuropsychological symptoms (development or reduction) followed by modulation of neuroinflammation and, therefore, creating one of the ‘vicious circles’ of MS (Figure 1).
Figure 1.
The possible role of dopamine in the development of clinical symptoms and autoimmune inflammation in MS. The dopaminergic system disturbance causes MS neuropsychological symptoms, which may aggravate MS course by the induction of pro-inflammatory cytokine production. MS exacerbation may induce a disturbance of dopamine metabolism and increase neuropsychological symptom severity.
3. The Role of Dopamine in Regulation of Neuroimmune Interaction in MS
The Th17 immune response is known to be involved in the pathogenesis of several autoimmune diseases, including MS [28]. Th17 cells produce pro-inflammatory cytokines such as interleukin (IL)-17, IL-21, IL-22, granulocyte- and granulocyte-macrophage colony-stimulating factors (G-CSF and GM-CSF). The pathogenetic role of Th17 cells in MS pathogenesis could be explained by their ability to transmigrate into CNS through the blood–brain barrier by expressing chemokine receptor 6 (CCR6 [CD196]) and producing IL-17 and IL-22 [29,30]. The presence of Th17 cells and IL-17 in the foci of EAE and MS, as well as an increase in the number of Th17 cells in blood and IL-17 production by activated peripheral blood mononuclear cells (PBMCs) in vitro, was demonstrated in MS patients during relapse compared with MS patients in clinical remission or with healthy subjects [26]. Mice knocked out by IL-17A or IL-23 have been shown to be resistant to EAE. The same effect on EAE development has IL-17 or IL-23 neutralization [31,32,33]. Finally, the role of Th17 cells on MS pathogenesis is confirmed by the influence of disease-modifying drugs on Th17 functions [34].
Recent studies have shown the ability of dopamine to modulate Th17 cell function. According to literature data, dopamine has various effects on Th17 cells. According to different reports, dopamine may either increase or reduce IL-17 production in MS [35]. Possibly, this could depend on the micro-environmental conditions and dopamine concentration. Depending on the concentration, dopamine may activate different dopaminergic receptors, which have different affinity and functions [35]. It is well known that there are at least five subtypes of dopamine receptors (D1–D5). D1- and D5-dopaminergic receptors (D1-like family) are coupled to Gαs and activate adenylate cyclase enzyme, increasing the level of cyclic adenosine monophosphate (cAMP). By contrast, D2-, D3-, and D4-dopaminergic receptors (D2-like family) are coupled to Gαi and inhibit adenylate cyclase enzyme, decreasing the cAMP level [36].
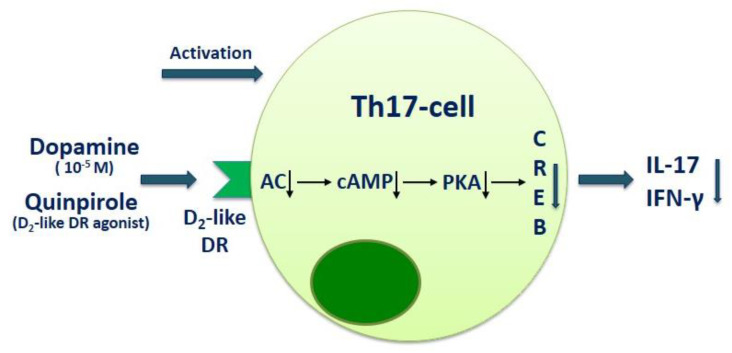
However, the involvement of dopaminergic receptors in modulation of Th17 cell function is not sufficiently investigated. According to our previous studies, the inhibitory effect of dopamine on Th17 cells could be mediated by the D2-like dopaminergic receptor activation. Thus, it has been shown, that D2-like dopaminergic receptor antagonist sulpiride abolishes dopamine-mediated IL-17 suppression in PBMC culture obtained from relapsing–remitting MS patients, while D1-like dopaminergic receptor antagonist SCH23390, conversely, further reduces dopamine-mediated inhibition of IL-17 production [26]. It has also been shown that SCH23390 exerts a direct inhibitory effect on IL-17, IFN-γ, and GM-CSF production by anti-CD3 and anti-CD28-activated CD4+ T cells in relapsing–remitting MS patients, while sulpiride has no effect on cytokine production [37]. These data correspond with data from Huang et al., who showed the inhibitory effect of D2-like dopaminergic receptor agonist quinpirole on the expression of Th17- and Th1-specific transcription factors (ROR-γt and T-bet, respectively) as well as IL-17, IL-22, IFN-γ, and IL-2 mRNA expression in concanavalin A-activated T-lymphocytes obtained from mesenteric lymph nodes of mice. Conversely, quinpirole increased FOXP3 and TGF-β mRNA expression, which indicates the different effect of D2-like dopaminergic receptor activation in pro-inflammatory Th1/Th17 cells and anti-inflammatory Treg cells [38]. In line with these data, Cosentino et al. reported the inhibitory effect of dopamine on human CD4+ and CD8+ Treg cells through D1-like dopaminergic receptor [39,40].
Huang and coauthors also found that activation of D2-like dopaminergic receptor by quinpirole decreased intracellular cAMP content and reduced the phosphorylated cAMP-response element-binding (CREB) level in T cells. The D2-like dopaminergic receptor antagonist haloperidol blocked the effects of quinpirole. These data suggest that D2-like dopaminergic receptor modulate the cAMP-protein kinase A (PKA)-CREB pathway and regulate Th17 cell function (Figure 2) [38].
Figure 2.
The role of dopamine and D2-like dopaminergic receptor in modulation of Th17 cell function. D2-like DR—D2-like dopaminergic receptor; CA—adenylyl cyclase; cAMP—cyclic adenosine monophosphate; PKA—protein kinase A; CREB—cAMP response element-binding protein.
The effect of the D2-like receptor agonist on Th17 cells was observed also in vivo in mice with EAE. The study by Lieberknecht et al. showed that treatment of EAE mice with a pramipexole (D2- and D3-dopaminergic receptor agonist) reduced IL-17 production in lymph nodes and prevented clinical signs of the disease [41]. In this regard, D2-like dopaminergic receptor attracts attention as a new therapeutic target in MS. However, the molecular mechanisms that mediated D2-like dopaminergic receptor on Th17 cells need to be clarified.
It is important to discuss the effect of dopamine on mononuclear phagocytes, including dendritic cells and macrophages. The etiology and triggering mechanisms of the autoimmune inflammation in MS are still unclear. Dendritic cells and macrophages are professional antigen-presenting cells and play a central role in innate immune system functioning. Both types of these cells are present in the CNS. Depending on the phenotype, dendritic cells and macrophages can support autoimmune inflammation and immunological tolerance to self-antigens [42,43,44]. It is important to note that resident macrophages of the CNS form microglia are capable of producing cytokines, presenting antigens’ underlying mechanisms of neuroinflammation and MS progression [43,45]. It has been shown that in both acute and chronic foci of demyelination in MS, macrophages are more abundant to T- and B-lymphocytes [46,47,48].
In the demyelination lesions, macrophages can comprise cell populations: resident glial cells of the CNS and macrophages that penetrate the blood–brain barrier from the periphery to the CNS (infiltrating macrophages). According to literature data, the activation of microglial cells mediates the early neuroinflammation stage [49]. Conversely, infiltrating macrophages mediate the effector phase of demyelination [50]. It is important to note that in healthy brain tissue, there are no infiltrating macrophages [43].
The influence of dopamine on dendritic cells that induce Th17 immune response has been shown. In a study by Nakano et al., it was shown that blockade of D1-like dopaminergic receptor by specific antagonists (SCH23390, SKF83566 or LE300) on human dendritic cells inhibited their ability to induce Th17-immune response. Conversely, blockade of D2-like dopaminergic receptor by L750667, sulpiride, or nemonapride (D2-like dopaminergic receptor antagonists) enhanced dendritic cells-mediated Th17-cell differentiation. They also found that treatment with SCH23390 had a preventive and curative effect on EAE in mice, while D2-like dopaminergic receptor antagonist (L750667) increased the EAE severity [51]. The results of Prado et al. and Osorio-Barrios et al. studies confirm the anti-inflammatory effect of D1-like receptor (D5-receptor) deficiency on dendritic-cell-induced Th17 immune response in EAE mice [52,53,54].
The ability of dopamine to modulate macrophages and microglia function has also been shown [55]. In particular, dopamine has been shown to inhibit the production of IL-6 and IL-1β through NF-kB pathway suppression in LPS-activated murine microglial cells. However, authors did not find any effect of agonists/antagonists of D1- and D2-like dopaminergic receptor on dopamine-mediated microglial cell suppression [56].
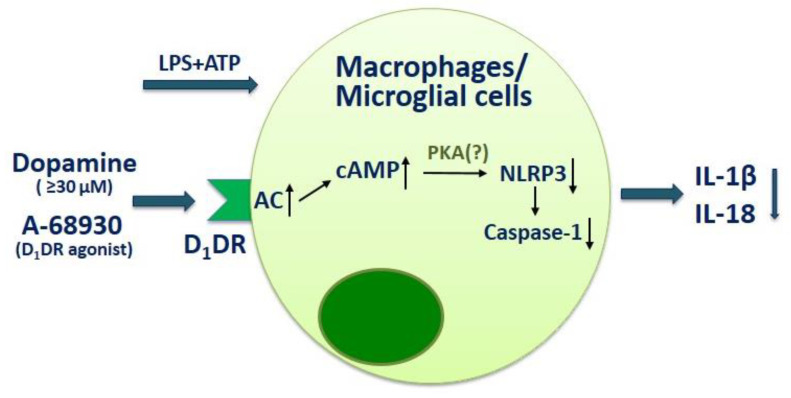
Another study reported the influence of dopamine on macrophages through NLRP3-inflammasome modulation. The treatment of macrophages with dopamine reduced NLRP3-dependent caspase-1 activation as well as IL-1β and IL-18 production by microglial cells upon stimulation with LPS and adenosine triphosphate (ATP). The D1-dopaminergic receptor also has been shown to be involved in dopamine-mediated NLRP3 inflammasome inhibition. Thus, knockdown of D1-dopaminergic receptor in macrophages significantly blunted the inhibitory effect of dopamine on inflammasome activation, while agonist of D1-dopaminergic receptor A-68930 had the same effect with dopamine on macrophages (Figure 3) [57]. These data suggest the dual role of D1-like dopaminergic receptor in the modulation of the innate immunity.
Figure 3.
The influence of dopamine on macrophages and microglial cell function. D1DR—D1-dopaminergi receptor; CA—adenylyl cyclase; cAMP—cyclic adenosine monophosphate; PKA—protein kinase A; LPS—lipopolysaccharide; ATP—adenosintriphosphat.
In addition, the influence of atypical antipsychotic agents (such as quetiapine, risperidone, and clozapine) on EAE course through modulation of macrophages/microglia also has been shown [58,59,60]. However, these therapeutic agents affect not only dopaminergic receptors.
Taken together, these data suggest the critical role of the dopaminergic system in the control of neuroinflammatory processes. It can be proposed that dopamine may affect EAE and MS pathogenesis by mechanisms that are not mutually exclusive: by influencing neuroinflammation through the regulation of the severity of neuropsychological symptoms or by direct impact on the cells of both adaptive and innate immune systems, including resident immune cells of CNS.
4. The Prospects of Dopaminergic Therapeutics in MS Treatment
The in vitro anti-inflammatory effect of dopaminergic therapeutics has been confirmed in vivo. The data on the influence of dopamine/dopaminergic receptor targeting on EAE/MS pathogenesis and course are presented in detail in Table 1.
Table 1.
The effect of dopaminergic receptor targeting on EAE/MS pathogenesis and course.
| Disease | Cell Type | The Effect of Dopaminergic Receptor Targeting | Authors |
|---|---|---|---|
| EAE | Splenic lymphocytes |
D2-like dopaminergic receptor agonist bromocriptine has a preventive and curative effect on EAE in mice. The treatment with bromocriptine reduces prolactin serum level and splenic lymphocyte proliferation upon Con A stimulation. | Riskind et al., 1991 [61] |
| EAE | Not investigated | The treatment with D2-like dopaminergic receptor agonist bromocriptine reduces prolactin plasma level and clinical symptoms of acute and chronic EAE. | Dijkstra et al., 1993 [62] |
| EAE | Dendritic cells T cells |
D1-like dopaminergic receptor antagonist (SCH23390) has a preventive and curative effect on EAE in mice. D2-like dopaminergic receptor antagonist (L750667) enhances EAE severity. The spleen cells from SCH23390-treated mice produce less IL-17 than the PBS-treated mice. Dendritic cells treated with SCH23390 and transferred to mice have the same effect compared with the direct influence of SCH23390 on EAE. | Nakano et al., 2008 [51] |
| EAE | Dendritic cells | D5-dopaminergic receptor deficiency on dendritic cells impair LPS-induced IL-12 production and IL-23 mRNA expression and attenuate CD4+ T-cell activation. D5-dopaminergic receptor deficient mice show a delayed onset of the EAE and reduced disease severity compared with WT mice. Transfer of D5-dopaminergic receptor deficiency dendritic cells to EAE mice lessens the infiltration of Th17 cells in the CNS. | Prado et al., 2012 [52] |
| EAE | Peripheral lymphoid tissue |
The treatment with a D2- and D3-dopaminergic receptors agonist pramipexole reduces IL-17, IL-1β and TNF-α production in lymph nodes and prevents clinical signs of the EAE in mice. | Lieberknecht et al., 2017 [41] |
| EAE | Dendritic cells | Transfer of D5-dopaminergic-receptor-deficient dendritic cells to EAE mice reduces EAE manifestation and decreases the infiltration of IL-17+, IFN-γ+IL-17+ and GM-CSF+IFN-γ+IL-17+CD4+ T cells at the peak of the disease. | Prado et al., 2018 [53] |
| EAE | CD4+ T cells | D5-dopaminergic receptor signaling in naive CD4+ T cells potentiates T cell activation with the acquisition of Th17-phenotype favoring EAE development. D5-dopaminergic receptor signaling in Treg cells contributes to their suppressive activity. | Osorio-Barrios et al., 2018 [54] |
| RRMS Progressive MS |
Not investigated | No evidence of clinical efficacy of bromocriptine therapy in MS. After one year of treatment, 14 of the 15 patients showed disease progression. | Bissay et al., 1994 [63] |
| RRMS | PBMCs CD4+ T cells CD8+ T cells |
Dopamine (at 10−6 M) enhances IL-17 and IL-21 but suppresses IL-10 and TGF-β production by PHA-activated PBMCs in RRMS patients and enhances IL-17 production by anti-CD3/anti-CD28-antibody-activated CD4+ and CD8+ T cells in RRMS patients. | Ferreira et al., 2014 [64] |
| RRMS | CD3+ T cells | Dopamine (at 10−6 M) enhances IL-6, IL-17, IL-21, and IL-22 but suppresses IL-10 production by anti-CD3/anti-CD28-antibody-activated CD3+ T cells in RRMS patients. | Alvarenga-Filho et al., 2016 [23] |
| RRMS | PBMCs | Dopamine (at 10−5 M) suppresses IL-17 and IFN-γ production by anti-CD3/anti-CD28 microbead-activated PBMCs in RRMS patients and healthy subjects. Blockade of D1-like dopaminergic receptor with SCH23390 enhances the inhibitory effect of dopamine on IL-17 production, while blockade of D2-like dopaminergic receptor with sulpiride conversely reduces it. | Melnikov et al., 2016 [26] |
| RRMS | CD4+ T cells | Dopamine (at 10−5 M) suppresses IL-17 and IFN-γ production by anti-CD3/anti-CD28 microbead-activated CD4+ T cells in RRMS patients and healthy subjects. Blockade of D2-like dopaminergic receptor with sulpiride reduces dopamine-mediated IL-17 suppression in MS patients. Blockade of D1-like dopaminergic receptor with SCH23390 reduces IL-17 and GM-CSF production by activated CD4+ T cells in MS patients and in healthy subjects. | Melnikov et al., 2020 [37] |
In this regard, the repurposing of dopaminergic drugs is one of the most promising directions in the development of new therapeutic approaches in MS [8,9,35]. However, the existing data were obtained primarily in in vitro studies or EAE (an animal model of MS), while the effect of dopaminergic system targeting on MS is not sufficiently studied. In one pilot study (Bissay et al. [63]), the influence of D2-like dopaminergic receptor agonist bromocriptine on relapsing–remitting and progressive MS courses was tested. However, no clinical benefits of such therapy were observed [63]. It should be noted that patients who participated in these studies had not been treated with disease-modifying drugs [63]. It can be proposed that dopaminergic therapy may be more effective as an add-on to first-line disease-modifying drugs (interferon-β or glatiramer acetate). In line with this suggestion, Green et al. reported that a combination of clozapine and glatiramer acetate therapy was more effective in EAE treatment than using clozapine or glatiramer acetate alone [60].
Secondly, in Bissay’s study, patients with progressive MS were included. However, the MS progression is mediated by neurodegeneration, partly independent of autoimmune inflammation [65], while dopamine presumably affects inflammatory processes. Finally, this study contains just fifteen MS patients. Thus, the effect of bromocriptine on MS course needs to be clarified.
5. Conclusions
Taken together, the results of more than twenty years of studies suggest the potential prospect of dopaminergic therapeutics for the treatment of CNS demyelinating diseases. However, confirmation of the clinical efficacy of such therapeutics still needs to be clarified. Several reasons necessitate the development of such a therapeutic. About 30 percent of MS patients do not respond to first-line disease-modifying drugs, so it is required to switch over to more effective therapeutics [66]. At the same time, the treatment with the second- or third-line therapy may cause severe side effects. In addition, the cost of such treatment may be high. It is possible to propose that using dopaminergic therapeutics as add-on pathogenetic MS treatment will control disease course without treatment escalation. However, efficacy of such therapeutics needs to be confirmed in clinical trials.
Author Contributions
M.M.: writing—original draft preparation; M.P.: writing—review and editing; A.B.: project administration. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant from the Russian Science Foundation (project №19-75-00075).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Boyko A., Melnikov M. Prevalence and Incidence of Multiple Sclerosis in Russian Federation: 30 Years of Studies. Brain Sci. 2020;10:305. doi: 10.3390/brainsci10050305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu X., Chi S., Wang Q., Li C., Xu B., Zhang J., Chen X. Efficacy and safety of monoclonal antibody therapies for relapsing remitting multiple sclerosis: A network meta-analysis. Mult. Scler. Relat. Disord. 2018;25:322–328. doi: 10.1016/j.msard.2018.08.026. [DOI] [PubMed] [Google Scholar]
- 3.Soleimani B., Murray K., Hunt D. Established and Emerging Immunological Complications of Biological Therapeutics in Multiple Sclerosis. Drug Saf. 2019;42:941–956. doi: 10.1007/s40264-019-00799-1. [DOI] [PubMed] [Google Scholar]
- 4.Sellner J., Rommer P.S. Immunological consequences of “immune reconstitution therapy” in multiple sclerosis: A systematic review. Autoimmun. Rev. 2020;19:102492. doi: 10.1016/j.autrev.2020.102492. [DOI] [PubMed] [Google Scholar]
- 5.Yu Y.J., Watts R.J. Developing therapeutic antibodies for neurodegenerative disease. Neurotherapeutics. 2013;10:459–472. doi: 10.1007/s13311-013-0187-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ziemssen T. Modulating processes within the central nervous system is central to therapeutic control of multiple sclerosis. J. Neurol. 2005;252(Suppl. 5):v38–v45. doi: 10.1007/s00415-005-5007-2. [DOI] [PubMed] [Google Scholar]
- 7.Hodo T.W., de Aquino M.T.P., Shimamoto A., Shanker A. Critical Neurotransmitters in the Neuroimmune Network. Front. Immunol. 2020;11:1869. doi: 10.3389/fimmu.2020.01869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cosentino M., Marino F. Adrenergic and dopaminergic modulation of immunity in multiple sclerosis: Teaching old drugs new tricks? J. Neuroimmune Pharm. 2013;8:163–179. doi: 10.1007/s11481-012-9410-z. [DOI] [PubMed] [Google Scholar]
- 9.Marino F., Cosentino M. Multiple sclerosis: Repurposing dopaminergic drugs for MS—The evidence mounts. Nat. Rev. Neurol. 2016;12:191–192. doi: 10.1038/nrneurol.2016.33. [DOI] [PubMed] [Google Scholar]
- 10.Melnikov M., Sviridova A., Rogovskii V., Oleskin A., Boziki M., Bakirtzis C., Kesidou E., Grigoriadis N., Boyko A. Serotoninergic system targeting in multiple sclerosis: The prospective for pathogenetic therapy. Mult. Scler. Relat. Disord. 2021;51:102888. doi: 10.1016/j.msard.2021.102888. [DOI] [PubMed] [Google Scholar]
- 11.Manjaly Z.M., Harrison N.A., Critchley H.D., Do C.T., Stefanics G., Wenderoth N., Lutterotti A., Müller A., Stephan K.E. Pathophysiological and cognitive mechanisms of fatigue in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry. 2019;90:642–651. doi: 10.1136/jnnp-2018-320050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dobryakova E., Genova H.M., de Luca J., Wylie G.R. The dopamine imbalance hypothesis of fatigue in multiple sclerosis and other neurological disorders. Front. Neurol. 2015;6:52. doi: 10.3389/fneur.2015.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grech L.B., Butler E., Stuckey S., Hester R. Neuroprotective Benefits of Antidepressants in Multiple Sclerosis: Are We Missing the Mark? J. Neuropsychiatry Clin. Neurosci. 2019;31:289–297. doi: 10.1176/appi.neuropsych.18070164. [DOI] [PubMed] [Google Scholar]
- 14.Carandini T., Cercignani M., Galimberti D., Scarpini E., Bozzali M. The distinct roles of monoamines in multiple sclerosis: A bridge between the immune and nervous systems? Brain Behav. Immun. 2021;94:381–391. doi: 10.1016/j.bbi.2021.02.030. [DOI] [PubMed] [Google Scholar]
- 15.González-Arancibia C., Urrutia-Piñones J., Illanes-González J., Martinez-Pinto J., Sotomayor-Zárate R., Julio-Pieper M., Bravo J.A. Do your gut microbes affect your brain dopamine? Psychopharmacology. 2019;236:1611–1622. doi: 10.1007/s00213-019-05265-5. [DOI] [PubMed] [Google Scholar]
- 16.Boziki M.K., Kesidou E., Theotokis P., Mentis A.A., Karafoulidou E., Melnikov M., Sviridova A., Rogovski V., Boyko A., Grigoriadis N. Microbiome in Multiple Sclerosis; Where Are We, What We Know and Do Not Know. Brain Sci. 2020;10:234. doi: 10.3390/brainsci10040234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kozhieva M.K., Melnikov M.V., Rogovsky V.S., Oleskin A.V., Kabilov M.R., Boyko A.N. Gut human microbiota and multiple sclerosis. Zh. Nevrol. Psikhiatr. Im. S S Korsakova. 2017;117:11–19. doi: 10.17116/jnevro201711710211-19. [DOI] [PubMed] [Google Scholar]
- 18.Carandini T., Mancini M., Bogdan I., Rae C.L., Barritt A.W., Sethi A., Harrison N., Rashid W., Scarpini E., Galimberti D., et al. Disruption of brainstem monoaminergic fibre tracts in multiple sclerosis as a putative mechanism for cognitive fatigue: A fixel-based analysis. Neuroimage Clin. 2021;30:102587. doi: 10.1016/j.nicl.2021.102587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beurel E., Lowell J.A. Th17 cells in depression. Brain Behav. Immun. 2018;69:28–34. doi: 10.1016/j.bbi.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Coyle P.K. Symptom Management and Lifestyle Modifications in Multiple Sclerosis. Continuum. 2016;22:815–836. doi: 10.1212/CON.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 21.Mohr D.C., Lovera J., Brown T., Cohen B., Neylan T., Henry R., Siddique J., Jin L., Daikh D., Pelletier D. A randomized trial of stress management for the prevention of new brain lesions in MS. Neurology. 2012;79:412–419. doi: 10.1212/WNL.0b013e3182616ff9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alvarenga-Filho H., Salles M., Hygino J., Ferreira T.B., Sacramento P.M., Monteiro C., Vasconcelos C.C., Alvarenga R.M., Bento C.A. Fatigue favors in vitro Th1 and Th17-like cell expansion and reduces corticoid sensitivity in MS patients. J. Neuroimmunol. 2017;303:81–89. doi: 10.1016/j.jneuroim.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 23.Alvarenga-Filho H., Sacramento P.M., Ferreira T.B., Hygino J., Abreu J.E.C., Carvalho S.R., Wing A.C., Alvarenga R.M.P., Bento C.A.M. Combined exercise training reduces fatigue and modulates the cytokine profile of T-cells from multiple sclerosis patients in response to neuromediators. J. Neuroimmunol. 2016;293:91–99. doi: 10.1016/j.jneuroim.2016.02.014. [DOI] [PubMed] [Google Scholar]
- 24.Polak P.E., Kalinin S., Feinstein D.L. Locus coeruleus damage and noradrenaline reductions in multiple sclerosis and experimental autoimmune encephalomyelitis. Brain. 2011;134:665–677. doi: 10.1093/brain/awq362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carotenuto A., Wilson H., Giordano B., Caminiti S.P., Chappell Z., Williams S., Hammers A., Silber E., Brex P., Politis M. Impaired connectivity within neuromodulatory networks in multiple sclerosis and clinical implications. J. Neurol. 2020;267:2042–2053. doi: 10.1007/s00415-020-09806-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Melnikov M., Belousova O., Murugin V., Pashenkov M., Boyкo A. The role of dopamine in modulation of Th-17 immune response in multiple sclerosis. J. Neuroimmunol. 2016;292:97–101. doi: 10.1016/j.jneuroim.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 27.Escribano B.M., Aguilar-Luque M., Bahamonde C., Conde C., Lillo R., Sanchez-Lopez F., Giraldo A.I., Cruz A.H., Luque E., Gascon F., et al. Natalizumab Modifies Catecholamines Levels Present in Patients with Relapsing- Remitting Multiple Sclerosis. Curr. Pharm. Des. 2016;22:4876–4880. doi: 10.2174/1381612822666160708000453. [DOI] [PubMed] [Google Scholar]
- 28.Milovanovic J., Arsenijevic A., Stojanovic B., Kanjevac T., Arsenijevic D., Radosavljevic G., Milovanovic M., Arsenijevic N. Interleukin-17 in Chronic Inflammatory Neurological Diseases. Front. Immunol. 2020;11:947. doi: 10.3389/fimmu.2020.00947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kebir H., Kreymborg K., Ifergan I., Dodelet-Devillers A., Cayrol R., Bernard M., Giuliani F., Arbour N., Becher B., Prat A. Human TH17 lymphocytes promote blood-brain barrier disruption and central nervous system inflammation. Nat. Med. 2007;13:1173–1175. doi: 10.1038/nm1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sallusto F., Impellizzieri D., Basso C., Laroni A., Uccelli A., Lanzavecchia A., Engelhardt B. T-cell trafficking in the central nervous system. Immunol. Rev. 2012;248:216–227. doi: 10.1111/j.1600-065X.2012.01140.x. [DOI] [PubMed] [Google Scholar]
- 31.McGinley A.M., Sutton C.E., Edwards S.C., Leane C.M., DeCourcey J., Teijeiro A., Hamilton J.A., Boon L., Djouder N., Mills K.H.G. Interleukin-17A Serves a Priming Role in Autoimmunity by Recruiting IL-1β-Producing Myeloid Cells that Promote Pathogenic T Cells. Immunity. 2020;52:342–356. doi: 10.1016/j.immuni.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Cua D.J., Sherlock J., Chen Y., Murphy C.A., Joyce B., Seymour B., Lucian L., To W., Kwan S., Churakova T., et al. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature. 2003;421:744–748. doi: 10.1038/nature01355. [DOI] [PubMed] [Google Scholar]
- 33.Guo W., Luo C., Wang C., Wang Y.H., Wang X., Gao X.D., Yao W.B. Suppression of human and mouse Th17 differentiation and autoimmunity by an endogenous Interleukin 23 receptor cytokine-binding homology region. Int. J. Biochem. Cell. Biol. 2014;55:304–310. doi: 10.1016/j.biocel.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 34.Moser T., Akgün K., Proschmann U., Sellner J., Ziemssen T. The role of TH17 cells in multiple sclerosis: Therapeutic implications. Autoimmun. Rev. 2020;19:102647. doi: 10.1016/j.autrev.2020.102647. [DOI] [PubMed] [Google Scholar]
- 35.Melnikov M., Rogovskii V., Boyko A., Pashenkov M. Dopaminergic Therapeutics in Multiple Sclerosis: Focus on Th17-Cell Functions. J. Neuroimmune Pharm. 2020;15:37–47. doi: 10.1007/s11481-019-09852-3. [DOI] [PubMed] [Google Scholar]
- 36.Arreola R., Alvarez-Herrera S., Pérez-Sánchez G., Becerril-Villanueva E., Cruz-Fuentes C., Flores-Gutierrez E.O., Garcés-Alvarez M.E., de la Cruz-Aguilera D.L., Medina-Rivero E., Hurtado-Alvarado G., et al. Immunomodulatory Effects Mediated by Dopamine. J. Immunol. Res. 2016;2016:3160486. doi: 10.1155/2016/3160486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Melnikov M., Sviridova A., Pashenkov M., Boyko A. Dopamine Suppresses Th17-Cells Function in Multiple Sclerosis. Poster Presentation. European Charcot Foundation. 28th Annual Meeting, Digital, 15–19 November 2020: The Role of Environmental Factors in Multiple Sclerosis. [(accessed on 24 April 2021)]; Available online: https://www.charcot-ms.org/28th-annual-meeting-digital/poster-presentations/basic-studies/mikhail-melnikov-57.
- 38.Huang Y., Chen C.C., Wang T.T., Qiu Y.H., Peng Y.P. Dopamine receptors modulate T lymphocytes via inhibition of cAMP-CREB signaling pathway. Neuro. Endocrinol. Lett. 2016;37:491–500. [PubMed] [Google Scholar]
- 39.Cosentino M., Fietta A.M., Ferrari M., Rasini E., Bombelli R., Carcano E., Saporiti F., Meloni F., Marino F., Lecchini S. Human CD4+CD25+ regulatory T cells selectively express tyrosine hydroxylase and contain endogenous catecholamines subserving an autocrine/paracrine inhibitory functional loop. Blood. 2007;109:632–642. doi: 10.1182/blood-2006-01-028423. [DOI] [PubMed] [Google Scholar]
- 40.Nasi G., Ahmed T., Rasini E., Fenoglio D., Marino F., Filaci G., Cosentino M. Dopamine inhibits human CD8+ Treg function through D1-like dopaminergic receptors. J. Neuroimmunol. 2019;332:233–241. doi: 10.1016/j.jneuroim.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 41.Lieberknecht V., Junqueira S.C., Cunha M.P., Barbosa T.A., de Souza L.F., Coelho I.S., Santos A.R., Rodrigues A.L., Dafré A.L., Dutra R.C. Pramipexole, a Dopamine D2/D3 Receptor-Preferring Agonist, Prevents Experimental Autoimmune Encephalomyelitis Development in Mice. Mol. Neurobiol. 2017;54:1033–1045. doi: 10.1007/s12035-016-9717-5. [DOI] [PubMed] [Google Scholar]
- 42.Flórez-Grau G., Zubizarreta I., Cabezón R., Villoslada P., Benitez-Ribas D. Tolerogenic Dendritic Cells as a Promising Antigen-Specific Therapy in the Treatment of Multiple Sclerosis and Neuromyelitis Optica From Preclinical to Clinical Trials. Front. Immunol. 2018;9:1169. doi: 10.3389/fimmu.2018.01169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nally F.K., De Santi C., McCoy C.E. Nanomodulation of Macrophages in Multiple Sclerosis. Cells. 2019;8:543. doi: 10.3390/cells8060543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Melnikov M.V., Paschenkov M.V., Boyko A.N. Dendritic cells in multiple sclerosis. Zh. Nevrol. Psikhiatr. Im. S S Korsakova. 2017;117:22–30. doi: 10.17116/jnevro20171172222-30. [DOI] [PubMed] [Google Scholar]
- 45.Absinta M., Lassmann H., Trapp B.D. Mechanisms underlying progression in multiple sclerosis. Curr. Opin. Neurol. 2020;33:277–285. doi: 10.1097/WCO.0000000000000818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Polman C.H., Dijkstra C.D., Sminia T., Koetsier J.C. Immunohistological analysis of macrophages in the central nervous system of Lewis rats with acute experimental allergic encephalomyelitis. J. Neuroimmunol. 1986;11:215–222. doi: 10.1016/0165-5728(86)90005-6. [DOI] [PubMed] [Google Scholar]
- 47.Brück W., Sommermeier N., Bergmann M., Zettl U., Goebel H.H., Kretzschmar H.A., Lassmann H. Macrophages in multiple sclerosis. Immunobiology. 1996;195:588–600. doi: 10.1016/S0171-2985(96)80024-6. [DOI] [PubMed] [Google Scholar]
- 48.Henderson A.P., Barnett M.H., Parratt J.D., Prineas J.W. Multiple sclerosis: Distribution of inflammatory cells in newly forming lesions. Ann. Neurol. 2009;66:739–753. doi: 10.1002/ana.21800. [DOI] [PubMed] [Google Scholar]
- 49.Ponomarev E.D., Shriver L.P., Maresz K., Dittel B.N. Microglial cell activation and proliferation precedes the onset of CNS autoimmunity. J. Neurosci. Res. 2005;81:374–389. doi: 10.1002/jnr.20488. [DOI] [PubMed] [Google Scholar]
- 50.Ajami B., Bennett J.L., Krieger C., McNagny K.M., Rossi F.M. Infiltrating monocytes trigger EAE progression, but do not contribute to the resident microglia pool. Nat. Neurosci. 2011;14:1142–1149. doi: 10.1038/nn.2887. [DOI] [PubMed] [Google Scholar]
- 51.Nakano K., Higashi T., Hashimoto K., Takagi R., Tanaka Y., Matsushita S. Antagonizing dopamine D1-like receptor inhibits Th17 cell differentiation: Preventive and therapeutic effects on experimental autoimmune encephalomyelitis. Biochem. Biophys. Res. Commun. 2008;373:286–291. doi: 10.1016/j.bbrc.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 52.Prado C., Contreras F., González H., Díaz P., Elgueta D., Barrientos M., Herrada A.A., Lladser Á., Bernales S., Pacheco R. Stimulation of dopamine receptor D5 expressed on dendritic cells potentiates Th17-mediated immunity. J. Immunol. 2012;188:3062–3070. doi: 10.4049/jimmunol.1103096. [DOI] [PubMed] [Google Scholar]
- 53.Prado C., Gaiazzi M., González H., Ugalde V., Figueroa A., Osorio-Barrios F.J., López E., Lladser A., Rasini E., Marino F., et al. Dopaminergic Stimulation of Myeloid Antigen-Presenting Cells Attenuates Signal Transducer and Activator of Transcription 3-Activation Favouring the Development of Experimental Autoimmune Encephalomyelitis. Front. Immunol. 2018;9:571. doi: 10.3389/fimmu.2018.00571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Osorio-Barrios F., Prado C., Contreras F., Pacheco R. Dopamine Receptor D5 Signaling Plays a Dual Role in Experimental Autoimmune Encephalomyelitis Potentiating Th17-Mediated Immunity and Favoring Suppressive Activity of Regulatory T-Cells. Front. Cell. Neurosci. 2018;12:192. doi: 10.3389/fncel.2018.00192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xia Q.P., Cheng Z.Y., He L. The modulatory role of dopamine receptors in brain neuroinflammation. Int. Immunopharmacol. 2019;76:105908. doi: 10.1016/j.intimp.2019.105908. [DOI] [PubMed] [Google Scholar]
- 56.Yoshioka Y., Sugino Y., Shibagaki F., Yamamuro A., Ishimaru Y., Maeda S. Dopamine attenuates lipopolysaccharide-induced expression of proinflammatory cytokines by inhibiting the nuclear translocation of NF-κB p65 through the formation of dopamine quinone in microglia. Eur. J. Pharm. 2020;866:172826. doi: 10.1016/j.ejphar.2019.172826. [DOI] [PubMed] [Google Scholar]
- 57.Yan Y., Jiang W., Liu L., Wang X., Ding C., Tian Z., Zhou R. Dopamine controls systemic inflammation through inhibition of NLRP3 inflammasome. Cell. 2015;160:62–73. doi: 10.1016/j.cell.2014.11.047. [DOI] [PubMed] [Google Scholar]
- 58.Mei F., Guo S., He Y., Wang L., Wang H., Niu J., Kong J., Li X., Wu Y., Xiao L. Quetiapine, an atypical antipsychotic, is protective against autoimmune-mediated demyelination by inhibiting effector T cell proliferation. PLoS ONE. 2012;7:e42746. doi: 10.1371/journal.pone.0042746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Green L.K., Zareie P., Templeton N., Keyzers R.A., Connor B., La Flamme A.C. Enhanced disease reduction using clozapine, an atypical antipsychotic agent, and glatiramer acetate combination therapy in experimental autoimmune encephalomyelitis. Mult. Scler. J. Exp. Transl. Clin. 2017;3:2055217317698724. doi: 10.1177/2055217317698724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Robichon K., Patel V., Connor B., La Flamme A.C. Clozapine reduces infiltration into the CNS by targeting migration in experimental autoimmune encephalomyelitis. J. Neuroinflamm. 2020;17:53. doi: 10.1186/s12974-020-01733-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Riskind P.N., Massacesi L., Doolittle T.H., Hauser S.L. The role of prolactin in autoimmune demyelination: Suppression of experimental allergic encephalomyelitis by bromocriptine. Ann. Neurol. 1991;29:542–547. doi: 10.1002/ana.410290514. [DOI] [PubMed] [Google Scholar]
- 62.Dijkstra C.D., van der Voort E.R., de Groot C.J., Uitdehaag B.M., Polman C.H., Berkenbosch F. The therapeutic effect of bromocriptine on acute and chronic experimental allergic encephalomyelitis. Ann. Neurol. 1992;31:450–451. doi: 10.1002/ana.410310420. [DOI] [PubMed] [Google Scholar]
- 63.Bissay V., De Klippel N., Herroelen L., Schmedding E., Buisseret T., Ebinger G., De Keyser J. Bromocriptine therapy in multiple sclerosis: An open label pilot study. Clin. Neuropharmacol. 1994;17:473–476. doi: 10.1097/00002826-199410000-00011. [DOI] [PubMed] [Google Scholar]
- 64.Ferreira T.B., Barros P.O., Teixeira B., Cassano T., Centurião N., Kasahara T.M., Hygino J., Vasconcelos C.C., Filho H.A., Alvarenga R., et al. Dopamine favors expansion of glucocorticoid-resistant IL-17-producing T cells in multiple sclerosis. Brain Behav. Immun. 2014;41:182–190. doi: 10.1016/j.bbi.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 65.Faissner S., Plemel J.R., Gold R., Yong V.W. Progressive multiple sclerosis: From pathophysiology to therapeutic strategies. Nat. Rev. Drug Discov. 2019;18:905–922. doi: 10.1038/s41573-019-0035-2. [DOI] [PubMed] [Google Scholar]
- 66.Teter B., Agashivala N., Kavak K., Chouhfeh L., Hashmonay R., Weinstock-Guttman B. Characteristics influencing therapy switch behavior after suboptimal response to first-line treatment in patients with multiple sclerosis. Mult. Scler. 2014;20:830–836. doi: 10.1177/1352458513513058. [DOI] [PubMed] [Google Scholar]