Abstract
Background
There are no reports of a large-scale survey on the infection prevention measures against coronavirus disease 2019 (COVID-19) in nephrology facilities. This study investigated the facility-level nephrology practices adopted during the COVID-19 pandemic and their associated challenges. Additionally, the treatment patterns and outcomes of chronic kidney disease (CKD) patients with COVID-19 were reviewed.
Methods
We conducted a nationwide questionnaire survey of 704 educational facilities that were certified by the Japanese Society of Nephrology (JSN) from October 20, 2020 to November 16, 2020. The questionnaire reviewed the facility characteristics, infection prevention measures taken during routine nephrology practice, impact of COVID-19 on nephrology practice, experiences in managing CKD patients with COVID-19, and nosocomial transmission in the nephrology unit.
Results
Of the 347 facilities that responded, 95.1% checked outpatients’ body temperatures and COVID-19 symptoms at their visits. To reduce face-to-face contact, 80% and 70% of the facilities lengthened the intervals between outpatient visits and introduced online/telephonic consultations, respectively. As a result, more than half of the hospitals experienced a decrease in the numbers of outpatients and inpatients (64% and 50%, respectively). During the study period, 347 facilities managed 479 CKD patients with COVID-19. Oxygen administration and mechanical ventilation were performed for 47.8% and 16.5% of the patients, respectively, with a 9.2% total mortality rate.
Conclusion
This survey demonstrated that JSN-certified educational nephrology facilities adopted multiple measures to manage the COVID-19 pandemic; however, they faced several challenges. Sharing these experiences could standardize these approaches and prepare us better for the future.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10157-021-02082-z.
Keywords: COVID-19, SARS-CoV-2, Chronic kidney disease, Questionnaire survey
Introduction
Chronic kidney disease (CKD) is a risk factor for end-stage kidney disease, as well as a variety of other conditions, such as cardiovascular diseases and dementia [1–3]. With respect to the recent spread of coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2, CKD has been identified as a risk factor for severe COVID-19 [4].
The COVID-19 outbreak was first confirmed in China in November 2019 [5], and the first Japanese COVID-19 patient was identified in January 2020 [6]. Due to the rapid spread of COVID-19 after April 2020, facilities have struggled to manage their patients, both with and without symptoms that were suggestive of COVID-19. Despite the dire situation, pre-dialysis CKD patients still required regular outpatient visits for medical checkups and prescriptions, as well as hospital admissions, if necessary. However, during the COVID-19 pandemic, each facility may have cared for pre-dialysis CKD patients in different ways. The types of infection prevention measures and consultation systems that were adopted in each nephrology department have not been investigated on a nationwide scale.
In this study, we conducted a nationwide questionnaire survey that targeted educational facilities certified by the Japanese Society of Nephrology (JSN), to investigate the types of infection prevention measures taken against COVID-19, and to assess the challenges faced by these nephrology facilities due to these measures. The summary of the survey results will prove useful for the comparison and standardization of the management of COVID-19 in patients with CKD and allow for better preparation for the future or the next pandemic.
Materials and methods
Surveyed hospitals
This research targeted JSN-certified educational facilities (N = 704). The JSN was established in 1959 and has worked to spread correct knowledge about kidney diseases to the public, while conducting research on nephrology and its related fields, which could benefit the public. The society has over 10,000 members.
Questionnaire development
The COVID-19 Task Force Committee was established by the Japanese Association of Dialysis Physicians (JADP), Japanese Society for Dialysis Therapy (JSDT), and JSN [7]. The authors in this study comprised part of the task force committee members. The committee summarized the important points in the medical care system and infection prevention measures for patients with CKD during the COVID-19 pandemic. The study contents and methodology were developed and refined based on this summary. Draft survey instruments were distributed to the committee members, and feedback was gathered through e-mail comments, as well as through in-person discussion.
The final Japanese version of the questionnaire and its English translation are shown in the Online Appendix. The questionnaire consisted of 5 parts: (i) facility characteristics (8 questions), (ii) infection prevention measures in routine nephrology practice (7 questions), (iii) impact of COVID-19 on routine nephrology practice (8 questions), (iv) experiences with managing CKD patients with COVID-19 (7 questions), and (v) nosocomial transmission in the nephrology department (3 questions). Nosocomial transmission was defined as horizontal COVID-19 transmission among the staff or patients in the facility.
The JSN ethics review board approved this study (approval number 80). Informed consent was not necessary as this study was a facility-based survey that did not require individual patient’s information. Therefore, the need for written informed consent was waived.
Data collection
The questionnaires were sent by mail to eligible facilities and simultaneously distributed by e-mail from the 3 related societies and associations (JADP, JSDT, and JSN). The response period was from October 20, 2020 to November 16, 2020. There were 2 response methods: (1) the response form could be faxed in or (2) a web form could be filled out.
Data analysis
We summarized the data from the questionnaires that were returned from the 374 facilities for descriptive purposes. We compared the implementation statuses of the infection prevention measures that were taken in the medical institutions that were designated for specific infectious diseases and other facilities using the Chi-squared test.
SAS® University Edition (SAS Institute, Cary, NC, United States) was used for the analysis.
Results
Part 1: characteristics of the participating facilities
Of the 704 JSN-certified educational facilities, a total of 347 facilities responded (49.3% response rate). The facilities that responded were distributed throughout Japan, and there were no obvious differences in the response rates between the regions, which were as follows: Hokkaido, 50.0%; Tohoku, 62.1%; Kanto (excluding Tokyo), 44.5%; Tokyo, 55.2%; Chubu, 48.9%; Kinki, 44.8%; Chugoku, 54.5%; Shikoku, 40.0%; Kyusyu, 53.3%; and Okinawa, 57.1%. Among the 347 facilities that responded to the survey, 31.7% were officially designated for the management of infectious diseases in the Japanese healthcare system, which was similar to 29.7% among the JSN-certified educational facilities (N = 704) targeted in the current survey.
Part 2: implementation statuses of the infection prevention measures during the COVID-19 pandemic
Table 1 shows the percentages of the facilities that were reported as “yes” for each question. Both the overall percentages and proportions according to the institutions’ infectious disease treatment designations are shown. Overall, 20.2% answered that all medical staff wore goggles or face shields at all times during general practice, and only 4.9% wore disposable, non-permeable gowns, or plastic aprons. Additionally, 76.7% and 89.6% responded that medical staff wore goggles or face shields, and disposable, non-permeable gowns or plastic aprons, respectively, when performing invasive procedures. When patients visited the facilities, 95.1% used temperature measurements and interviews around COVID-19-related symptoms to check all outpatients, regardless of whether they were suspected of having an infectious disease. There were no significant differences between the groups for any of the five questions when the facilities were evaluated according to their infectious disease treatment designations.
Table 1.
Implementation statuses of the infection prevention measures at each nephrology facility, both overall and according to the facilities’ designated statuses for the treatment of specific infectious diseases
| Overall (N = 347) n (%) |
Medical institutions that were designated for the treatment of specific infectious diseases | p value | |||
|---|---|---|---|---|---|
| Yes (N = 110) n (%) |
No (N = 237) n (%) |
||||
| Q1 | All the medical staff wear goggles or face shields at all times during general practice | 70 (20.2) | 19 (17.3) | 51 (21.5) | 0.359 |
| Q2 | All the medical staff wear disposable, non-permeable gowns or plastic aprons at all times during general practice | 17 (4.9) | 5 (4.5) | 12 (5.1) | 0.835 |
| Q3 | Medical staffs who are performing invasive procedures wear goggles or face shields | 266 (76.7) | 79 (71.8) | 187 (78.9) | 0.147 |
| Q4 | Medical staffs who are performing invasive procedures wear disposable, non-permeable gowns, or plastic aprons | 311 (89.6) | 95 (86.4) | 216 (91.1) | 0.175 |
| Q5 | At their visit, all patients are screened for infectious diseases through temperature measurements and interviews about symptoms | 330 (95.1) | 102 (92.7) | 228 (96.2) | 0.163 |
With respect to the inpatients, 66.7% of the surveyed facilities conducted some form of COVID-19 screening test (such as polymerase chain reaction [PCR] and antigen tests, chest computed tomography [CT], or a combination of these tests [11.0%, 8.7%, 7.2%, and 39.8%, respectively]) for emergency admissions, while 34.0% did so for scheduled admissions (PCR and antigen tests, chest CT, or a combination of these tests [18.2%, 1.7%, 4.9%, and 9.2%]).
Part 3: impact of COVID-19 on routine nephrology practice
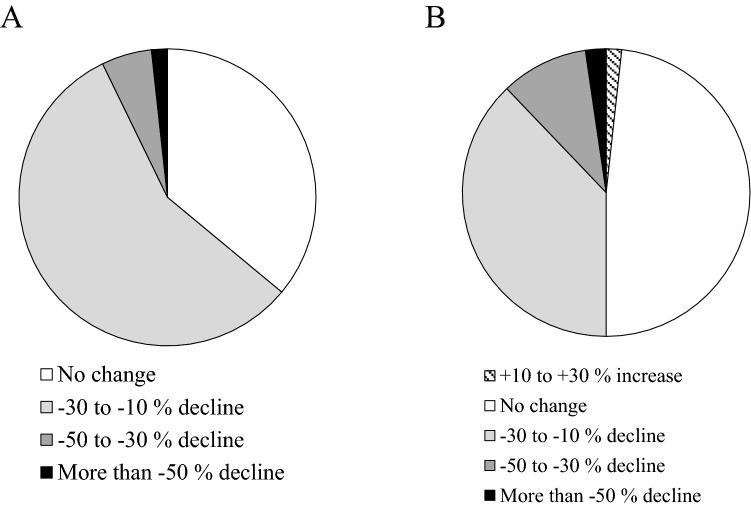
The majority of facilities (64%) experienced a decrease in the number of outpatients (Fig. 1A). Notably, 1.7% reported a substantial decrease (50% or more) in the number of outpatients. Similarly, 50% of the facilities showed a decrease in the number of inpatients (Fig. 1B), including 2.3% that reported a substantial decrease (50% or more). However, some facilities (2.3%) did report a small increase (10% to 30%) in the number of inpatients.
Fig. 1.
The distribution of the facilities according to the change in the proportion of (A) outpatients and (B) inpatients per facility
To minimize patient contact, 80% of the facilities indicated that they extended the intervals between the outpatient visits and 70% of facilities reported that they implemented online or telephonic consultations. Overall, 13% of the facilities experienced problems related to the extension of the interval between visits or online/telephonic consultations. Table 2 lists the details of each problem that was reported by the facilities that responded. Many of the responses mentioned inadequate drug-dosage adjustment and worsened management due to the lack of face-to-face consultation and/or blood tests. Some inconveniences in hospital operations were also reported, such as worsened hospital incomes and increased burden on the back office.
Table 2.
List of the inconveniences that were caused by the extended intervals between visits or the implementation of online/telephonic medical care
| Issues related to the treatment of patients with chronic kidney disease |
|---|
| Inadequate drug-dosage adjustment (21 answers in total) |
| - Worsened management of renal anemia (13 answers) |
| - Worsened glycemic control (3 answers) |
| - Worsened blood pressure control (2 answers) |
| - Delayed steroid dose reduction (1 answer) |
| Inadequate management due to lack of face-to-face examination and blood tests (20 answers in total) |
| - Renal function deterioration and/or worsened urinary protein (11 answers) |
| - The occurrence of acute heart failure, resulting in hospitalization (1 answer) |
| - Worsened systemic lupus erythematosus status (1 answer) |
| - Decreased ability to complete activities of daily living and worsened dementia symptoms (1 answer) |
| Patients asked for continuation of online/telephonic medical care despite the poor suitability (6 answers) |
| Increased number of patients who interrupted or discontinued hospital visits (2 answers) |
| Ran out of prescriptions (1 answer) |
| Issues related to the operation of the hospital |
|---|
| Decreased hospital profits (2 answers) |
| Increased burden on the back office (1 answer) |
| Confusion in relation to the provision of both regular and online/telephonic medical care (1 answer) |
| Patients did not answer the phone calls, which resulted in extended clinic hours (1 answer) |
Part 4: treatment patterns and outcomes of Japanese CKD patients with COVID-19
Of the 374 participating facilities, 125 (33%) treated CKD patients with COVID-19. There were 4.3 patients treated per facility on average (standard deviation, 6.8), with the highest number of patients at 50. In total, there were 479 CKD patients with COVID-19. The facilities that were designated for infectious disease treatment managed 175 out of the 479 patients (37%), while the remaining 304 patients (63%) were treated at other facilities.
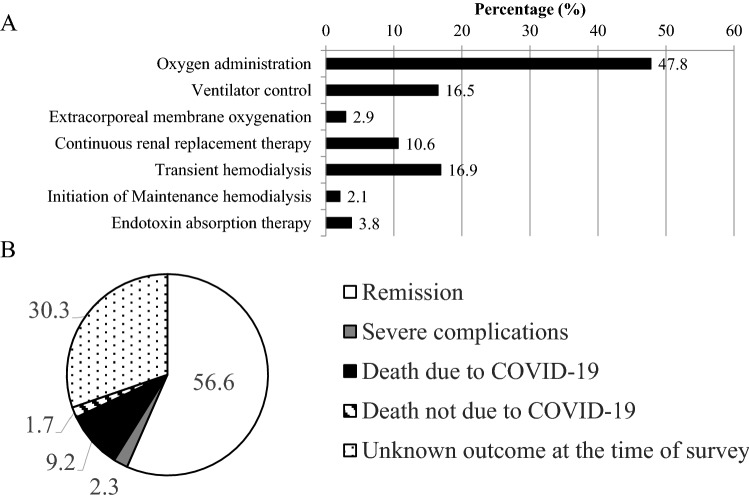
The percentages of patients who received each treatment are shown in Fig. 2A. Almost half of the patients with CKD who were infected with COVID-19 (47.8%) required oxygen administration, while 16.5% required ventilatory support, and 2.9% required extracorporeal membrane oxygenation treatment. Transient hemodialysis was performed for 16.9% of the patients with CKD, and 2.1% started maintenance hemodialysis because of worsened kidney function due to COVID-19.
Fig. 2.
A Treatment patterns and B distribution of the outcomes (when the survey was performed) of the chronic kidney disease patients with coronavirus disease 2019 (COVID-19, n = 479)
In terms of the outcomes, although almost half of the patients (56.6%) recovered from COVID-19, there were COVID-19-related deaths reported in 9.2% of the patients, and severe complications such as cerebral infarction or foot gangrene were observed in 2.3% of the patients (Fig. 2B).
Part 5: experiences with nosocomial COVID-19 transmission in the nephrology departments
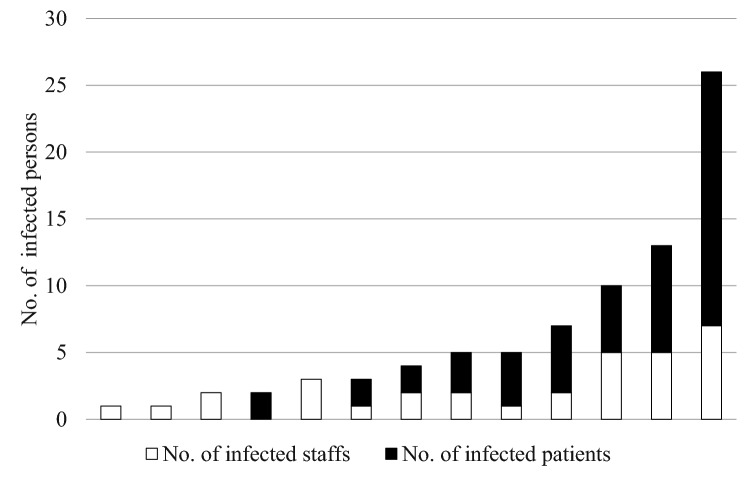
A total of 14 facilities responded that they experienced nosocomial COVID-19 transmission. Thirteen hospitals provided the actual number of infected staff members and patients. The number of infected persons per hospital ranged from 1 to 26, with a median of 4 (interquartile range 2–7). The staff accounted for 39.0% of the infected persons (Fig. 3).
Fig. 3.
Number of patients/staff members who were affected in the facilities with nosocomial COVID-19 transmission
Discussion
This study was the first nationwide survey of JSN-certified educational facilities that investigated the impact of the COVID-19 pandemic on the medical care system, as well as the infection control measures that were adopted at each facility. Through this study, we understood the real-time clinical situation in nephrology facilities in Japan. We hope that this information is useful in standardizing measures at each facility in case of similar future global health emergencies. The survey revealed several issues in clinical practice during the COVID-19 pandemic; this information is beneficial for all the medical staffs in the nephrology units and the patients with CKD, especially in Japan.
Most facilities prevented nosocomial transmission by measuring temperatures, checking symptoms when outpatients came to the hospital (Table 1, Question 05), and by performing a form of COVID-19 test for emergency admissions. However, only a few facilities always used goggles or face shields, and disposable, non-permeable gowns or plastic aprons during outpatient consultations. COVID-19 tests for regular admissions were also performed in a small number of facilities. Such measures will likely be necessary if community-acquired COVID-19 becomes more widespread. It should be noted that this survey was conducted from October to November 2020, during the period between the “second wave” and “third wave” in Japan. Thus, infection control measures may have changed thereafter. When the facilities were compared according to their designated statuses for the management of infectious diseases, there were no obvious differences in the implementation rates of infection prevention measures.
Many of the nephrology facilities that responded to this survey adopted measures such as extension of the intervals between consultations and/or provision of medical care using online tools and/or telephones to avoid face-to-face contact; however, this caused problems and inconveniences with medical treatment that directly affected patients. Examples of such cases were included in the survey results, such as inadequate drug-dosage adjustment and worsened disease management due to a lack of physical examination and blood tests (Table 2). These reports provoked concerns about whether patients with CKD were being treated properly during the COVID-19 pandemic. In addition, these measures raised issues related to hospital management. Some hospitals reported that the introduction of online and/or telephonic medical services resulted in a decrease in their profits due to the reimbursement system in Japan (Table 2). Moreover, the numbers of outpatients and inpatients decreased in more than half of the facilities that responded (Fig. 1). Other countries reported the same phenomenon, i.e., a decrease in hospital admissions and outpatient visits for diseases other than COVID-19 [8–10].
There are concerns that the combined effect of the aforementioned phenomena will have a negative impact on future maintenance of the medical system. Although the number of patients with COVID-19 in Japan is relatively small compared to other countries in Europe and the United States [11], our survey results show that COVID-19 still has a significant influence on the medical system.
In this facility-level analysis of treatment patterns and outcomes of CKD patients with COVID-19, the mortality rate was at least 9.2%. It is possible that this is a low estimate, because the clinical outcomes of 30.3% of the patients were unknown when the survey was performed. A substantial proportion of the patients (47.8%) required oxygen administration, and 16.5% needed ventilatory support, while the previous report of the 5,194 COVID-19 patients in Japanese general population showed that 32.1% received oxygen administration and 7.5% received ventilator support or extracorporeal membrane oxygenation treatment [12]. These results were consistent with those of previous reports. This suggests that CKD is a risk factor for severe COVID-19 [4]. However, because this questionnaire targeted a relatively large-volume hospital, it is also possible that the results may have disproportionately represented relatively severe disease. In addition, since we did not collect individual patients’ information, such as their age or CKD stage, in this survey, we were unable to make adjustments based on individual background factors.
In the facilities where nosocomial COVID-19 transmission occurred, the staff accounted for 39.0% of the infected cases; thus, we proposed that not only did nosocomial transmission have a direct negative impact on the affected patients, but it also led to a significant reduction in the number of available medical staff and a decrease in the quality of medical care for patients who were unaffected by COVID-19.
This study had several limitations. First, the response rate was 49.3%. Although the response rate did not vary widely among the different regions in Japan, or with/without designation for the management of infectious diseases, it is unclear how well the participating facilities represented the total population for other aspects, such as the facility size or its equipment level. In addition, there may have been recall bias or misreporting in the questionnaire, which may have led to misclassification of the results. Finally, as previously mentioned, we were unable to collect detailed information on individual patients’ characteristics (such as age, CKD stage, and comorbidities) in the section of the survey that dealt with the treatment patterns and the patients’ COVID-19-related outcomes. In this respect, further research is required to investigate the association between CKD status, stage, and treatment, and COVID-19-related outcomes.
This nationwide survey demonstrated that several nephrology facilities took various measures to treat patients with CKD safely, even during the COVID-19 pandemic. However, these facilities were still confronted by problems that were associated with the hastily implemented measures. Some problems were directly related to patient care, and these problems should be resolved promptly. Our results also suggested that patients with CKD may be more susceptible to severe COVID-19 symptoms; however, further examination of this concept in more detailed studies is required.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to express great appreciation to all the survey participants. We would also like to thank Editage (www.editage.com) for English language editing.
Author contributions
YS, MI, and MN planned the study and analyzed and interpreted the data. YS and MI mainly wrote the manuscript. All the other authors provided critical intellectual contributions in the development of manuscript, as well as the questionnaire. All authors read and approved the final manuscript.
Funding
This study was supported by the MHLW CA Program (grant number 20CA2042).
Declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethical approval
This article does not contain any studies with animals that were performed by any of the authors. All procedures performed in this study were in accordance with the ethical standards of the JSN ethics committee (approval number 80) and with the tenets of the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not necessary, because this study was a facility-based survey that did not require individual patient’s information. Therefore, the need for written informed consent was waived.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Matsushita K, Ballew SH, Astor BC, Jong PE, Gansevoort RT, Hemmelgarn BR, et al. Cohort profile: the chronic kidney disease prognosis consortium. Int J Epidemiol. 2013;42(6):1660–1668. doi: 10.1093/ije/dys173. [DOI] [PubMed] [Google Scholar]
- 2.Levin A, Tonelli M, Bonventre J, Coresh J, Donner JA, Fogo AB, et al. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet. 2017;390(10105):1888–1917. doi: 10.1016/S0140-6736(17)30788-2. [DOI] [PubMed] [Google Scholar]
- 3.Fukui A, Yokoo T, Nangaku M, Kashihara N. New measures against chronic kidney diseases in Japan since 2018. Clin Exp Nephrol. 2019;23(11):1263–1271. doi: 10.1007/s10157-019-01786-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Pneumonia of unknown cause in China. 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/.
- 6.Furuse Y, Ko YK, Saito M, Shobugawa Y, Jindai K, Saito T, et al. Epidemiology of COVID-19 outbreak in Japan, from January–March 2020. Jpn J Infect Dis. 2020;73(5):391–393. doi: 10.7883/yoken.JJID.2020.271. [DOI] [PubMed] [Google Scholar]
- 7.Kikuchi K, Nangaku M, Ryuzaki M et al. COVID-19 Task Force Committee of the Japanese Association of Dialysis Physicians, Japanese Society for Dialysis Therapy, Japanese Society of Nephrology. COVID-19 of dialysis patients in Japan: current status and guidance on preventive measures. Ther Apher Dial. 2020; 24:361–5. 10.1111/1744-9987.13531 [DOI] [PMC free article] [PubMed]
- 8.Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324(1):96–99. doi: 10.1001/jama.2020.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Filippo O, D’Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Domeyer P, Katsari V, Mariolis A. Chronic non-communicable diseases: a sacrifice on the altar of COVID-19? Br J Gen Pract. 2020;70(695):281. doi: 10.3399/bjgp20X710057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVID-19 map-johns Hopkins coronavirus resource center. https://coronavirus.jhu.edu/map.html. Accessed 3 Jul 2021.
- 12.Saito S, Asai Y, Matsunaga N, Hayakawa K, Terada M, Ohtsu H, et al. First and second COVID-19 waves in Japan: a comparison of disease severity and characteristics. J Infect. 2021;82(4):84–123. doi: 10.1016/j.jinf.2020.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.