Abstract
Chronic infection, especially in the setting of obstruction like calculous disease, may result in the fistula tract development of fistula tract from kidney to the other proximal organs. However, nephrocutaneous fistula is a rare complication, and the primary cause of its development is previous surgical intervention, trauma, or malignancy. Our case was a 26-year-old Afghan man with xanthogranulomatous pyelonephritis (XGP) resulted in spontaneous nephrocutaneous fistula. The patient underwent radical nephrectomy. Our case shows that previous surgery is not the only cause of fistula. After surgery, he presented with secondary enterocutaneous fistula due to surgery or chronic underlying inflammation. After systemic antibiotic therapy and total parenteral nutrition, he became well and discharged from the hospital. As a result, XGP is a rare subtype of chronic pyelonephritis that requires immediate evaluation and early diagnosis. Patients should be considered for possible complications such as fistulas. Physicians should be aware of this issue for appropriate diagnosis and treatment.
Keywords: Nephrocutaneous fistula, xanthogranulomatous pyelonephritis, enterocutaneous fistula, chronic pyelonephritis, nephrectomy
Introduction
Xanthogranulomatous pyelonephritis (XGP) is an unusual and invasive cause of chronic pyelonephritis in which lipid-laden macrophages of granulomatous tissue result in massive destruction of renal tissue [1]. Schlagonhaufer first described XGP in 1916 [2]. Then in 1944, it was named xanthogranuloma by Osterlin [3]. Complications of diffuse XGP can lead to entero-colonic fistula, emphysematous pyelonephritis, para-nephritic abscess, psaos muscle abscess and even can lead to sepsis. Therefore, timely identification and treatment of XGP is crucial [4,5].
Spontaneous nephrocutaneous fistula is a rare and severe disease. The lateral sinus drain is usually the first sign of a nephrocotaneous fistula. Kidney stones, xanthogranulomatous pyelonephritis, and renal tuberculosis are associated with nephrocutaneous fistula [6]. Although renal fistula formation to adjacent organs is not unusual, however nephrocutaneous fistula is a rare sequel of XGP and few cases have been reported in the literature [7-10]. It typically occurs in patients with a history of renal surgery [7,11].
We report a case of nephrocutaneous fistula caused by XGP in a 26-year-old man that presented with flank pain, purulent pus-like drainage and fever. Results of the histological analysis show the presence of XGP. The patient underwent a nephrectomy. After surgery, the patient developed enterocotaneus fistula. Most enterocutaneous fistulas are iatrogenic/postoperative, but it also can develop spontaneously [12]. This presentation is very dangerous because enterocotaneus fistula itself can lead to sepsis and has been associated with high mortality rates in studies [13]. Fortunately, He recovered well after surgery and antibiotic therapy. He recovered well post-operating. As we know, this is the first case report of XGP-induced nephrocotaneous fistula, after which the patient developed secondary enterocutaneous fistula.
Case report
In December 2019, a 26-year-old Afghan man with complaints of purulent discharge from an ulcer over his left side and fever and chill was admitted to the hospital. Additionally, he has a 3-month history of recurrent left flank pain. His past medical history was notable just for hypothyroidism, and his past surgical history was unremarkable.
On physical examination, the patient was febrile, had left flank pain and an ulcer of 1.5 cm × 1.5 cm on the left side of the back with purulent discharge.
Laboratory evaluations show elevated White blood cells (WBC) count (15 × 109/L), creatinine of 1.4 mg/dl, and normal urine analysis. No evidence of pulmonary or extrapulmonary Tuberculosis (TB) was identified. An Multidetector Computed Tomography (MDCT) scan with contrast of the abdomen and pelvis showed atrophic and nonfunctional left kidney containing a stone (13 mm) and fat density. Magnetic resonance imaging showed a fistula tract from the left kidney through the left psoas muscle of the back (Figure 1). Given the patient’s nationality and suspected TB, since one of the differential diagnoses of autonephrectomy is TB, we have thoroughly examined it. According to the consultation with the infectious disease service, Mantoux, a 24-hour urine Polymerase Chain Reaction (PCR) test and morning urine sample in three BK tests were requested, and urinary tuberculosis was ruled out.
Figure 1.
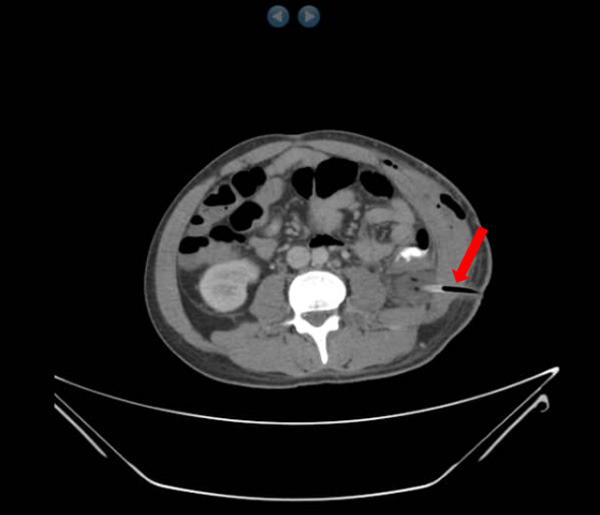
MRI image showing fistula tract from the left kidney through the left psoas muscle of the back.
An elective radical nephrectomy and fistulectomy were carried out successfully. A drain was inserted through the fistula tract to the back. On histopathological analysis of nephrectomy specimen, chronic granulomatous inflammatory cell of the left kidney was noted and no malignancy founded (Figure 2).
Figure 2.
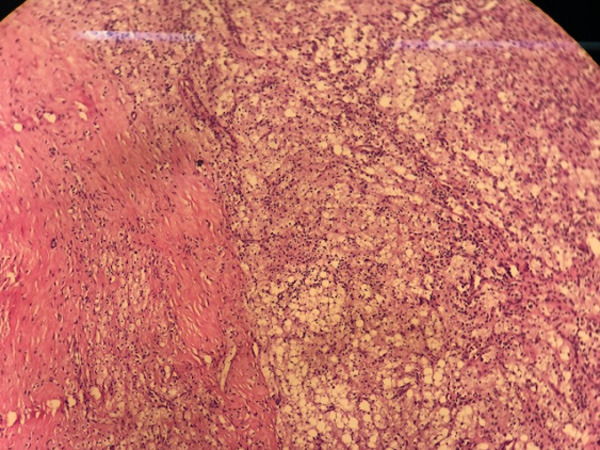
Section showed replacement of renal parenchyma with granuloma-like structure, foamy histiocytes, occasional multinucleated giant cells, inflammatory cells with extension to perinephritic fat (scale × 100).
After surgical intervention, at thirst post-operation day, the patient develops fecal excretion from the left-back surgical incision. On computed tomography, the enterocutaneous fistula was seen (Figure 3). The patient became Nil Per Os (NPO) and underwent total parenteral nutrition. Systemic injectable antibiotics Meropenem and Metronidazole was given. One week later, the patient recuperated well without any other intervention and discharged from the hospital.
Figure 3.
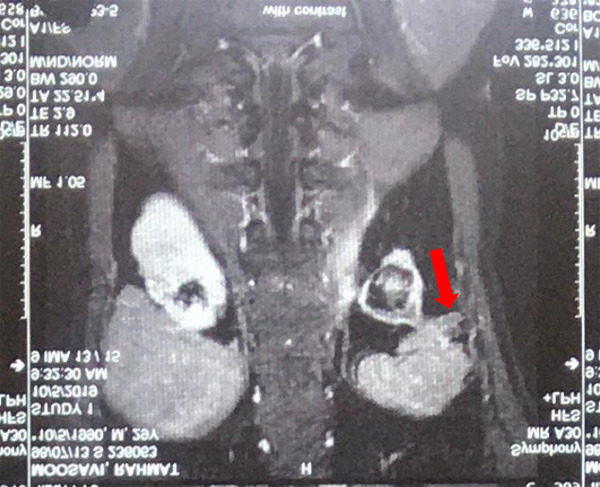
CT image showing enterocutaneous fistula.
On follow-up at 1 and 3 months later he was asymptomatic and had no complaint. His abdominopelvic Computed Tomography (CT) scan did not show any notable findings.
In this case, written consent and accompanying images, has been obtained from the patient, which is approved by the ethics committee.
Discussion
XGP is an unusual form of chronic pyelonephritis characterized histopathologically by massive renal destruction secondary to granulomatous tissue containing lipid-laden macrophages [14]. It usually affects women than men with ratio of 4:1 and usually occurs during the fifth and sixth decades of life [15].
Presenting symptoms usually include urinary tract infections, flank and abdominal pain, along with fever, malaise, weight loss, urinary incontinence, and enuresis [2].
Though the precise etiology of XGP is not clear, however, infection and obstruction of the urinary tract system are presented in 70-79 percent of patients [16]. Other predisposing factors are probably diabetes mellitus, abnormal lipid metabolism, and immunosuppression [17].
There are two forms of XGP: focal and diffuse. Based on the extent of inflammation and severity of disease a classification system for diffuse form of XGP has been described: stage 1: localized to the renal parenchyma, stage 2: spread to the perinephric fat, stage 3: extending into the Para renal space and other retroperitoneal structure [18].
Radiographic findings confirm the diagnosis, and CT is the reliable imaging modality [19]. XGP is almost always unilateral, and therefore the mainstay of treatment is surgical en-bloc nephrectomy. All involved tissues are removed, and any extensions of the disease, including fistulas, are closed [20].
Our case describes a rare finding of nephrocutaneous fistula due to XGP. In XGP, chronic inflammatory processes in infection presence result in perinephric abscess formation and fistula [7]. However, fistula between the kidney and skin is rare and typically occurs in patients with previous renal surgery [4]. In our case, the tract was due to XGP, and he has not any past surgical history. Radical nephrectomy and excision of the fistula were performed successfully. Although after surgery, he presented with enterocutaneous fistula that may be due to surgery or chronic inflammatory process. Enterocutaneous fistulas occur in 75 to 85% of cases in postoperative conditions, and fistulas occur spontaneously in 15% to 25% of cases, mostly due to Crohn’s disease. However, foreign bodies, radiation, inflammation or infection, and neoplasms cause spontaneous fissures [21].
The most common clinical manifestations of enterocutaneous fistula are lack of surgical recovery, abdominal symptoms, and intestinal obstruction signs. As our case, the contents of the bowel may also appear in the surgical wound [22]. He recovered well after seven days of Total Parenteral Nutrition (TPN) without any other intervention.
XGP and nephrocutaneous fistula, have been reported previously. Kiris et al. reported a case of XGP and coexisting renal replacement lipomatosis [10]. Pathenveetil et al. described a 45-year-old man with nephrocutaneous fistula formation in XGP after a history of the expulsion of stones in his kidney [8]. Biyani et al. similarly, described a case of XGP with bilateral nephrocutaneous fistula after several surgical interventions [23]. Similarly, in our case, few reported have existed in patients without any history of surgery [7,9]. Our case and similar reports illustrate an unusual finding that prior surgical procedure is not the only cause of fistula. However, as we know, this is the first case that shows enterocutaneous fistula because of the surgery or chronic inflammation process in XGP (Table 1).
Table 1.
Summary of the case reports included in discussion
| Reference N. | Publication | Coexisting disease | Age (year)/gender | Presenting symptoms | Prior surgery |
|---|---|---|---|---|---|
| [10] | Kiris et al. | Nephrolithiasis, Renal replacement lipomatosis | 24/M | fever, left lumbar pain, left lumbar mass sense | + |
| [9] | Weissman et al. | urinary tract infections | 57/M | fever, Hypotension | - |
| [7] | Alazab et al. | Nephrolithiasis | 37/F | Fever, purulent discharge, a palpable mass | - |
| [8] | Puthenveetil et al. | Nephrolithiasis | 45/M | flank pain, purulent discharge, fever with chill | + |
| [23] | Biyani et al. | urinary tract infections | 80/F | FUO, Fatigue, weight loss | + |
As a result, XGP is a rare subtype of chronic pyelonephritis that requires immediate evaluation and early diagnosis. Patients should be considered for possible complications such as fistulas. Besides, the leading cause of kidney fistula is surgery. Our case shows that previous surgery is not the only cause of the fistula. Imaging is essential for diagnosis and, ultimately, the treatment of choice for nephrectomy and fistula removal. The patient also developed secondary enterocutaneous fistula to surgery or chronic underlying inflammation. Physicians must be aware of this in order to make a timely diagnosis and appropriate treatment.
Disclosure of conflict of interest
None.
References
- 1.Parsons MA, Harris SC, Longstaff AJ, Grainger RG. Xanthogranulomatous pyelonephritis: a pathological, clinical and aetiological analysis of 87 cases. Diagn Histopathol. 1983;6:203–219. [PubMed] [Google Scholar]
- 2.Kuo CC, Wu CF, Huang CC, Lee YJ, Lin WC, Tsai CW, Wu VC, Chen YM, Wu MS, Chu TS, Wu KD. Xanthogranulomatous pyelonephritis: critical analysis of 30 patients. Int Urol Nephrol. 2011;43:15–22. doi: 10.1007/s11255-010-9778-8. [DOI] [PubMed] [Google Scholar]
- 3.Jha SK, Aeddula NR. Pyelonephritis Xanthogranulomatous. StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2020, StatPearls Publishing LLC.; 2020. [Google Scholar]
- 4.Loffroy R, Guiu B, Watfa J, Michel F, Cercueil JP, Krausé D. Xanthogranulomatous pyelonephritis in adults: clinical and radiological findings in diffuse and focal forms. Clin Radiol. 2007;62:884–890. doi: 10.1016/j.crad.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 5.Harikrishnan JA, Hall TC, Hawkyard SJ. Nephrobronchial fistula. A case report and review of the literature. Cent European J Urol. 2011;64:50–51. doi: 10.5173/ceju.2011.01.art12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rubilotta E, Balzarro M, Sarti A, Artibani W. Spontaneous nephrocutaneous fistula: a case report, update of the literature and management algorithm. Urol Int. 2016;97:241–246. doi: 10.1159/000360403. [DOI] [PubMed] [Google Scholar]
- 7.Alazab R, Ghawanmeh HM, Abushamma F, Ababneh O, Al-Karasneh AI. Spontaneous nephrocutaneous fistula: rare complication of xanthogranulomatous pyelonephritis. Urol Case Rep. 2017;11:44–46. doi: 10.1016/j.eucr.2016.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Puthenveetil RT, Baishya D, Barua S, Sarma D. Unusual case of nephrocutaneous fistula - our experience. Asian J Urol. 2016;3:56–58. doi: 10.1016/j.ajur.2015.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weissman S, Ghaffar M, Safavian D, Rubal S, Khabut A, Maruf MG, Krzyzak M. Nephrocutaneous fistula due to xanthogranulomatous pyelonephritis. Cureus. 2018;10:e3467. doi: 10.7759/cureus.3467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kiris A, Kocakoc E, Poyraz AK, Dagli F, Boztosun Y. Xanthogranulomatous pyelonephritis with nephrocutanous fistula and coexisting renal replacement lipomatosis: the report of a rare case. Clin Imaging. 2005;29:356–358. doi: 10.1016/j.clinimag.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Sarmiento Robles C, Blasco Carratalá F, Herrera Fernández F, Chica Rusillo A, Ostalé Gómez J. Spontaneous nephrocutaneous fistula. Report of a case and review of the literature. Arch Esp Urol. 1990;43:411–413. [PubMed] [Google Scholar]
- 12.Gribovskaja-Rupp I, Melton GB. Enterocutaneous fistula: proven strategies and updates. Clin Colon Rectal Surg. 2016;29:130–137. doi: 10.1055/s-0036-1580732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollington P, Mawdsley J, Lim W, Gabe SM, Forbes A, Windsor AJ. An 11-year experience of enterocutaneous fistula. Br J Surg. 2004;91:1646–1651. doi: 10.1002/bjs.4788. [DOI] [PubMed] [Google Scholar]
- 14.Goodman M, Curry T, Russell T. Xanthogranulomatous pyelonephritis (XGP): a local disease with systemic manifestations. Report of 23 patients and review of the literature. Medicine (Baltimore) 1979;58:171–181. [PubMed] [Google Scholar]
- 15.Goyal S, Gupta M, Goyal R. Xanthogranulomatous pyelonephritis: a rare entity. N Am J Med Sci. 2011;3:249–250. doi: 10.4297/najms.2011.3249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malek RS, Greene LF, DeWeerd JH, Farrow GM. Xanthogranulomatous pyelonephritis. Br J Urol. 1972;44:296–308. doi: 10.1111/j.1464-410x.1972.tb10080.x. [DOI] [PubMed] [Google Scholar]
- 17.McDermott RL, Dowling CM, Alsinnawi M, Grainger R. Incidental renocolic fistula with xanthogranulomatous pyelonephritis. Int J Surg Case Rep. 2013;4:222–224. doi: 10.1016/j.ijscr.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malek RS, Elder JS. Xanthogranulomatous pyelonephritis: a critical analysis of 26 cases and of the literature. J Urol. 1978;119:589–593. doi: 10.1016/s0022-5347(17)57559-x. [DOI] [PubMed] [Google Scholar]
- 19.Craig WD, Wagner BJ, Travis MD. Pyelonephritis: radiologic-pathologic review. Radiographics. 2008;28:255–277. doi: 10.1148/rg.281075171. [DOI] [PubMed] [Google Scholar]
- 20.Çaliskan S, Özsoy E, Kaba S, Koca O, Öztürk MI. Xanthogranulomatous pyelonephritis. Arch Iran Med. 2016;19:712–714. [PubMed] [Google Scholar]
- 21.Schecter WP, Hirshberg A, Chang DS, Harris HW, Napolitano LM, Wexner SD, Dudrick SJ. Enteric fistulas: principles of management. J Am Coll Surg. 2009;209:484–491. doi: 10.1016/j.jamcollsurg.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 22.Osborn C, Fischer JE. How I do it: gastrointestinal cutaneous fistulas. J Gastrointest Surg. 2009;13:2068–2073. doi: 10.1007/s11605-009-0922-7. [DOI] [PubMed] [Google Scholar]
- 23.Biyani CS, Torella F, Cornford PA, Brough SJ. Xanthogranulomatous pyelonephritis with bilateral nephrocutaneous fistulae. Urol Int. 1997;59:46–47. doi: 10.1159/000283016. [DOI] [PubMed] [Google Scholar]


