Abstract
Study Design:
A network meta-analysis.
Objectives:
Lumbar degenerative disc disease (LDDD) is an important issue in aging population, for which lumbar interbody fusion (LIF) is a feasible management in cases refractory to conservative therapy. There are various techniques available to perform LIF, including posterior (PLIF), transforaminal (TLIF), and anterior (ALIF) approaches. However, the comparative safety profile of these procedures remains controversial. Our study aimed to evaluate comparative adverse events of the LIF procedures in patients with LDDD.
Methods:
We searched 5 databases for relevant prospective cohort studies and randomized clinical trials. After quality assessments, we extracted neural, spinal, vascular, and wound events for conducting contrast-based network meta-analysis. Results were reported in risk ratio (RR), 95% confidence interval (CI), and surface under the cumulative ranking (SUCRA).
Results:
We identified 14 studies involving 921 participants with LDDD. Pooled result showed that open PLIF (OPLIF) leads to significantly higher overall adverse event rate than does open TLIF (OTLIF; RR = 3.43, 95% CI = 1.21-9.73). OTLIF confers the highest SUCRA in neural (78.7) and spinal (80.8) event rates. Minimally invasive TLIF has the highest SUCRA in vascular event (84.2), and minimally invasive PLIF has the highest SUCRA in wound event (88.1). No inconsistency or publication bias was detected in the results.
Conclusions:
Based on our results, perhaps OPLIF should be avoided in the management of LDDD due to the inferiority of overall complications. Specifically, TLIF seems to have the safest profile in terms of neural, spinal, and vascular events. Nevertheless, shared decision making is still mandatory when choosing the proper LIF procedure for patients with LDDD in clinical practice.
Keywords: lumbar, thoracic, degenerative disc disease, lumbar interbody fusion
Introduction
Lumbar degenerative disc disease (LDDD), which is an important issue in the elderly, is the most common causes of low back pain (LBP) in the global trend of aging population.1 In clinical practice, LBP is a very common complaint with respect to pain and disability among patients aged 65 or older, who are also the second most common age group to seek medical attention for LBP.2-5 For instance, LBP was one of the most commonly reported symptoms among 5201 participants leading to difficulties doing 17 activities on a daily basis.6
LDDD is an irreversible and multifactorial process of wear and tear in the lumbar disk architecture and integrity.7,8 Several factors, including, and not exclusive to, age, genetics, gender, obesity, physical activity, occupations (repetitive lifting or vibration), have been proposed to alter the natural course of disk, leading to the LDDD.7,8 LDDD is a spectrum of diseases, which may present as disc herniation, spondylosis, spondylolysis, spondylolisthesis, spinal stenosis, facet joint arthropathy, or their combination.9
In clinical practice, lumbar interbody fusion (LIF) is not only a popular operation but also a feasible treatment option for patients with LDDD who fail to respond to conservative therapy.10 The procedures were also implemented to treat other spinal disorders, including spondylolisthesis, scoliosis, severe disc degeneration, trauma, infection, and spinal fractures.11,12 These procedures can be conducted through several approaches, including anterior lumbar interbody fusion (ALIF), posterior lumbar interbody fusion (PLIF), and transforaminal lumbar interbody fusion (TLIF). Moreover, these LIF procedures can be executed in traditional open and minimally invasive approach (MIS). Although our previous study had delved into the comparative effectiveness of these LIF procedures for LDDD and revealed the superiority of MIS-PLIF in terms of pain relief and function improvement,13 the results were insufficient to provide definite guidance for spine surgeons due to inadequate comparison of safety profile among these techniques. Having further knowledge of comparative adverse events among these approaches can help surgeons have better insight into surgical planning and decisions making. Although previous studies have evaluated the safety of different surgical techniques, it still remains controversial owing to limited evidence to support one is better than the other. Therefore, we would like to update evidence for safety among the LIF procedures among patients with LDDD.
Methods
This study is a prospective systematic review with network meta-analysis and was registered on the online platform PROSPERO (CRD42018094237). The methodology and reporting structure of this study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Eligibility Criteria and Evidence Selection
Before we executed this systematic review, we followed previous work to define eligibility criteria for evidence selection and designed the relatively objective method for the selection process.13 The eligibility criteria were related to specific population, intervention, and study design. The criteria for population were the patients with only degenerative disc disease. For the criteria of intervention, the treatments should be open TLIF (OTLIF), MIS-TLIF, open PLIF (OPLIF), MIS-PLIF, or ALIF. The criteria for study design were randomized clinical trial (RCT) or prospective cohort study. According to these criteria, 2 authors (KYC and YKK) screened the title and abstract for eligibility. Then, they retrieved the full texts for the further review. A third author (YNK) made a final judgement for disagreement between the 2 authors during the evidence selection process.
Data Source and Search Strategy
After the eligibility criteria and the evidence selection process were defined, we searched the Cochrane library database (including Cochrane Central Register of Controlled Trials), EMBASE, Ovid MEDLINE, PubMed (including MEDLINE), and Web of Science for the prospective studies and RCTs comparing the safety of LIF procedures in patient with LDDD, from inception to February 6, 2020 (Supplementary File 1), encompassing all languages. The comprehensive search involved relevant terms of degenerative disc disease, OTLIF, MIS-TLIF, OPLIF, MIS-PLIF, and ALIF. The synonyms were combined using Boolean operator “OR,” and the different concepts were combined by Boolean operator “AND.” In this study, we further screened relevant reference list for potential evidence.
Data Extraction and Quality Assessment
Two authors (YKK and EYL) independently extracted study information and outcome data. The trial information included publication year, study region, study design, treatments, age, and sex (female rate). The outcomes data was overall adverse event, neural event, spinal event, vascular event, and wound event. All the outcomes were binary data. If original reports used percentage, we converted to events according to sample size.
Two authors (KYC and YKK) also reviewed studies and assessed quality of eligible studies. Following previous synthesis, our quality assessment applied the Cochrane Risk of Bias Tool (RoB) for assessing bias in randomized clinical trials and Risk of Bias in Non-randomized Studies–Interventions (ROBINS-I) tool for nonrandomized prospective studies. We used the RoB to check randomized allocation generation, randomized allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective report, and other source of bias. To assess nonrandomized prospective studies, we checked representative ness of the exposed cohort, selection of the nonexposed cohort, ascertainment of exposure, demonstration that outcome of interest was not present at start of study, comparability, assessment of outcome, was follow-up long enough for outcomes to occur, and adequacy of follow-up of cohorts according to the NOS. Any discrepancy on quality assessment was resolved by reaching a consensus with the other author (YNK).
Data Synthesis and Analysis
We synthesized quantitative data through contrast-based network meta-analysis in random-effects model. Because our outcomes were dichotomous data, we used events and sample size for pooled analysis in consistency model. Results were reported as risk ratio (RR) with 95% confidence interval (CI). We also applied surface under the cumulative ranking (SUCRA) to clarify risk probability among OTLIF, MIS-TLIF, OPLIF, MIS-PLIF, and ALIF. SUCRA is a numeric and graphical presentation of overall ranking among treatment groups. It transforms cumulative probabilities of each treatment into a single value between 0 and 1, with the higher value referring to the higher probability to be an effective treatment.14 Furthermore, we made a SUCRA cluster plot of overall adverse event, neural event, spinal event, vascular event, and wound event. We further analyzed the pooled quality by detecting inconsistency and small study bias in consistency model. Detection of inconsistency relied on Lu-Ades’ loop inconsistency test. About detection of small study bias in our network meta-analysis, we used adjusted funnel plot and Egger’s regression intercept. Determination of statistical significance in these analyses followed common threshold (P < .05). We conducted the analyses in STATA version 14 for Microsoft Windows.
Results
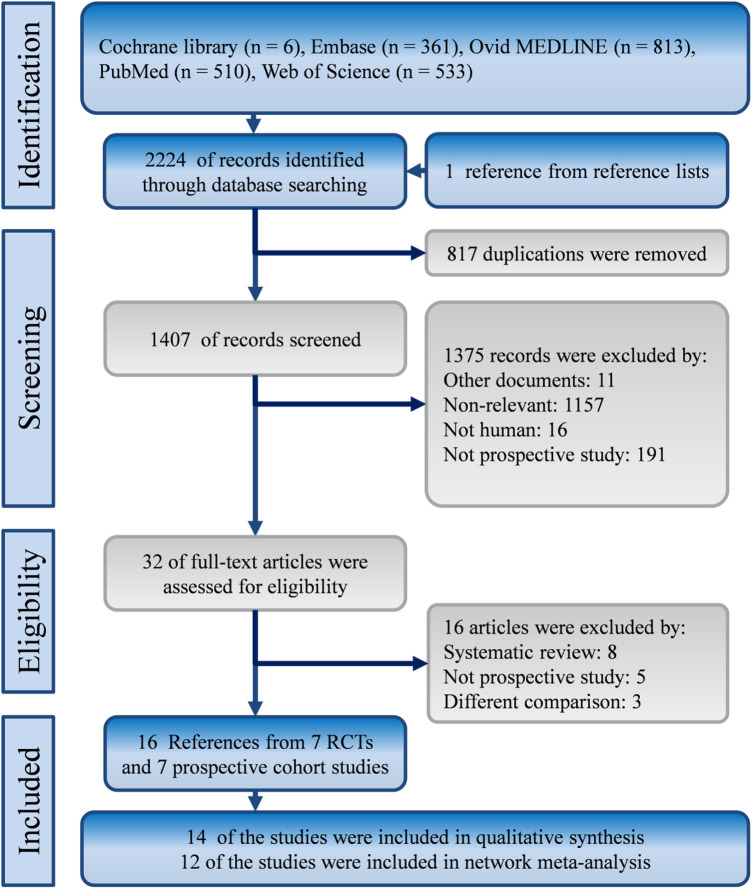
We identified 2224 references from the Cochrane library, Embase, Ovid Medline, PubMed, and Web of Science. Moreover, we followed reference lists of relevant syntheses and found one more reference. After title and abstract screening, we excluded duplicates (n = 817) and irrelevant references (n = 1375), and retrieved 32 full texts for further review. Finally, 7 randomized clinical trials and 7 prospective cohort studies met our eligibility criteria, and we included all of them in our synthesis. Figure 1 shows evidence selection flowchart.
Figure 1.
Flowchart of this systematic review with network meta-analysis of prospective studies. RCTs, randomized clinical trials.
Characteristics and Quality of Included Studies
Our study involves 14 studies: 7 randomized clinical trials and 7 prospective cohort studies from America (n = 3),15-17 Asia (n = 7),18-24 and Europe (n = 4).25-28 These studies recruited 921 patients with LDDD in OTLIF (n = 176), MIS-TLIF (n = 298), OPLIF (n = 122), MIS-PLIF (n = 60), and ALIF (n = 55) during the period from 1996 to 2014. Nearly half of cases were females (n = 437; 47.45%). Available information showed mean age in each study was from 33.62 years to 67.5 years. Relevant information is presented in Table 1, and quality of the included studies is shown in Supplementary File 2.
Table 1.
Characteristics of the Included Prospective Studies.
| Study | Area | Design | Procedure | Female/total | Mean age |
|---|---|---|---|---|---|
| Cheng et al, 2017 | Asia | PCS | Open PLIF, Open TLIF | 46/83 (55.42%) | 59.12 |
| Crandall et al, 2009 | America | PCS | Open TLIF, ALIF | 35/40 (87.50%) | 67.5 |
| Fen et al, 2010 | Asia | PCS | Open TLIF, MIS-TLIF | 30/62 (48.39%) | 51.6 |
| Hartwig et al, 2010 | Europe | RCT | Open PLIF, MIS-TLIF, ALIF | Total: 75 | NR |
| Hoff et al, 2016 | Europe | RCT | Open TLIF, ALIF | 26/62 (41.94%) | 5 |
| Kim et al, 2018 | Asia | RCT | Open PLIF, MIS-PLIF | 37/78 (47.43%) | 65.72 |
| Klara et al, 2003 | America | PCS | Open PLIF, ALIF | 17/32 (53.13%) | 48.44 |
| Kulkarni et al, 2016 | Asia | PCS | Open TLIF, MIS-TLIF | 40/61 (65.57%) | 51.08 |
| Lee et al, 2017 | Asia | PCS | Open PLIF, MIS-PLIF | 47/89 (52.81%) | 54.91 |
| Lin et al, 2012 | Asia | RCT | Open PLIF, MIS-TLIF | 35/102 (34.31%) | 51.52 |
| Parker et al, 2014 | America | PCS | Open TLIF, MIS-TLIF | 66/100 (66.00%) | 53.05 |
| Putzier et al, 2016 | Europe | RCT | Open PLIF MIS-TLIF | 27/47 (57.45%) | 62.83 |
| Rodríguez-Vela et al, 2013 | Europe | RCT | Open TLIF, MIS-TLIF | 14/41 (34.15%) | 42.46 |
| Xue et al, 2013 | Asia | RCT | Open PLIF, MIS-TLIF | 17/49 (34.69%) | 33.62 |
Abbreviations: ALIF, anterior lumbar interbody fusion; MIS-PLIF, minimally invasive posterior lumbar interbody fusion; MIS-TLIF, minimally invasive transforaminal lumbar interbody fusion; PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; PC, prospective cohort; RCT, randomized controlled trial.
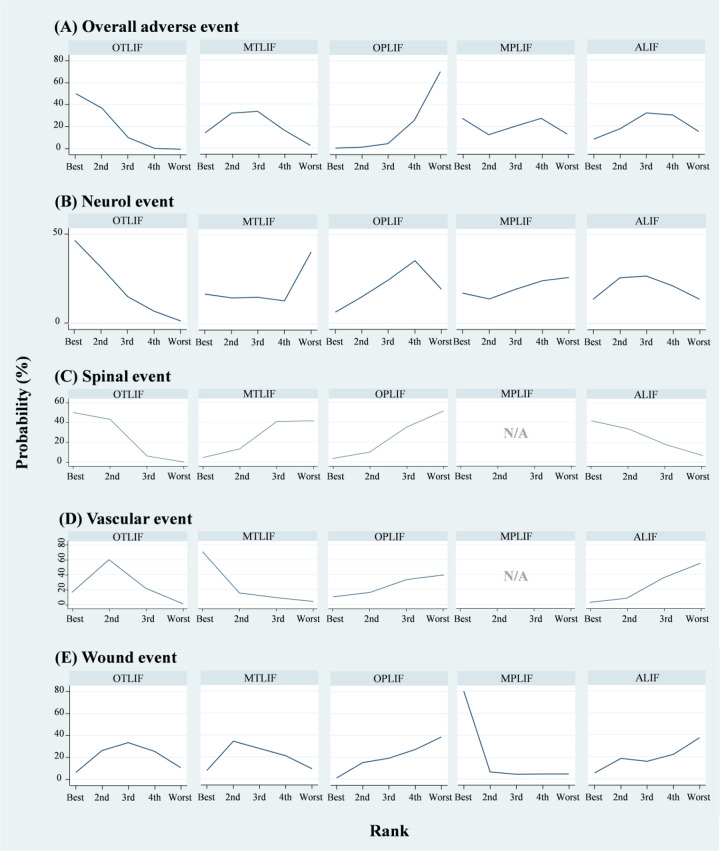
Overall Adverse Event
A total of 12 studies contributed to network meta-analysis of overall adverse event (Figure 2; Supplementary File 3).15-23,26-28 Pooled estimate showed that with OTLIF as the reference, there was no significant difference in overall adverse event rate compared to ALIF (RR 1.78, 95% CI 0.73 to 4.34), MIS-TLIF (RR 1.37, 95% CI 0.64 to 2.94), and MIS-PLIF (RR 1.57, 95% CI 0.27 to 9.00). Notably, OPLIF leads to significantly higher adverse event rate than OTLIF (RR 3.43, 95% CI 1.21 to 9.73). In SUCRA, OTLIF had the highest value of safety (mean rank = 1.6; SUCRA = 84.4) followed by MIS-TLIF (mean rank = 2.6; SUCRA = 59.5), MIS-PLIF (mean rank = 2.9; SUCRA = 53.4), ALIF (mean rank = 3.3; SUCRA = 43.5), and OPLIF (mean rank = 4.6; SUCRA = 9.1; Supplementary File 4). Loop inconsistency test did not show inconsistency in the network model of overall adverse event (χ2 = 1.64; P = .44; Supplementary File 5), and no evidence demonstrated small study effects in the pooled estimate of overall adverse event (t = −0.27, 95% CI −1.22 to 0.95; Supplementary File 6).
Figure 2.
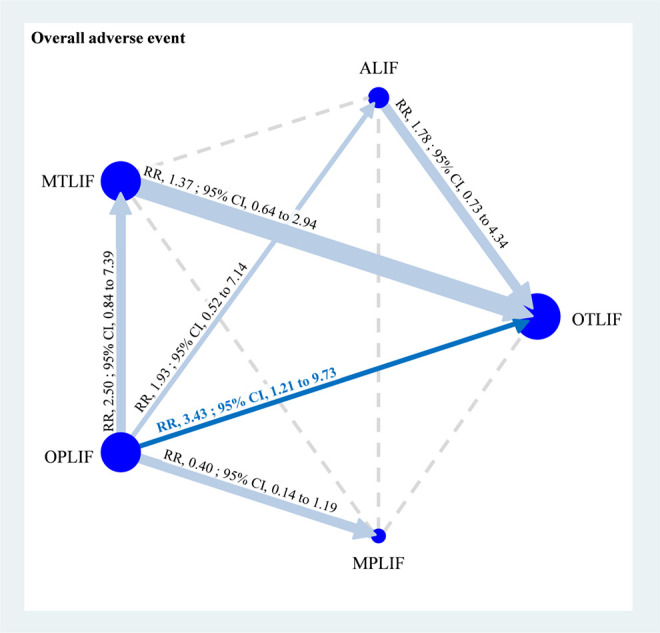
Network geometry of consistency model of overall adverse event. ALIF, anterior lumbar interbody fusion; CI, confidence interval; MIS-PLIF, minimally invasive posterior lumbar interbody fusion; MIS-TLIF, minimally invasive transforaminal lumbar interbody fusion; OPLIF, open posterior lumbar interbody fusion; OTLIF, open transforaminal lumbar interbody fusion; RR, risk ratio.
Neural Event
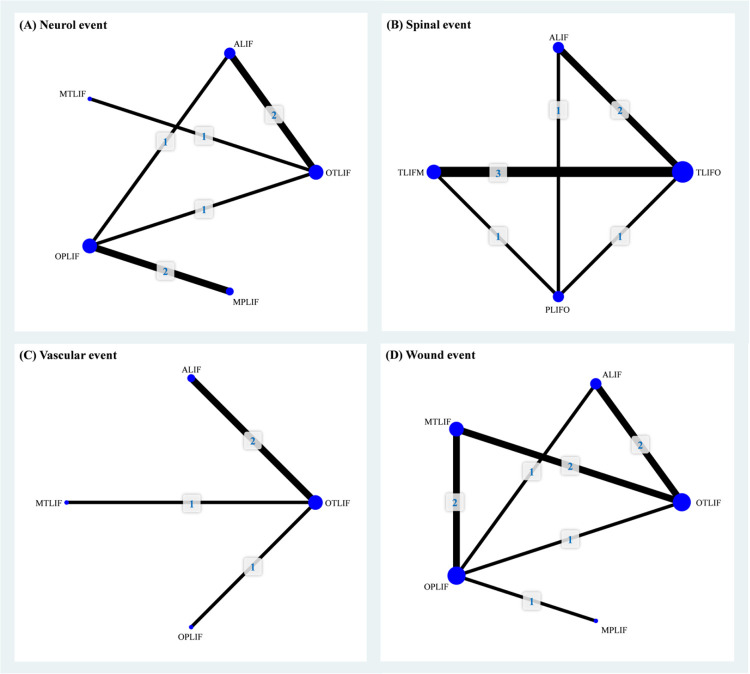
Seven of the included studies reported data on neural event among the 5 LIF procedures (Figure 3A).15,16,18,20,21,26,29 Pooled result of neural event rate indicated that no significant difference was noted among the comparisons of OTLIF, ALIF, MIS-TLIF, OPLIF, and MIS-PLIF though ALIF (RR 2.09, 95% CI 0.34 to 13.00), MIS-TLIF (RR 3.51, 95% CI 0.18 to 70.19), OPLIF (RR 3.10, 95% CI 0.28 to 34.57), and MIS-PLIF (RR 2.87, 95% CI 0.14 to 58.71) seemed to have higher neural event rate than does OTLIF (Table 2). Similar trend could be observed in SUCRA. OTLIF had the highest SUCRA value and mean rank of safety (mean rank = 1.9; SUCRA = 78.7), but mean ranks of the other 4 LIF procedures were very close to each other (Figure 4; Supplementary File 7). About quality of this pooled estimate, loop inconsistency test showed no significant difference in the network meta-analysis of neural event rate (χ2 = 0.00; P = .97; Supplementary File 8), and Egger’s test demonstrated no significant small study effects in the pooled estimate of neural event rate (t = −0.75, 95% CI −4.33 to 2.37; Supplementary File 9).
Figure 3.
Network geometry of consistency model of (A) neural event, (B) spinal event, (C) vascular event, and (D) wound event. ALIF, anterior lumbar interbody fusion; MIS-PLIF, minimally invasive posterior lumbar interbody fusion; MIS-TLIF, minimally invasive transforaminal lumbar interbody fusion; OPLIF, open posterior lumbar interbody fusion; OTLIF, open transforaminal lumbar interbody fusion.
Table 2.
Summary of Further Network Meta-Analysis for Total Number of Infectious Patients.
| Procedure | Model | Effect size | I 2 | Inconsistency | Publication bias | ||||
|---|---|---|---|---|---|---|---|---|---|
| Arm 1 | Arm 2 | RR | 95% CI | χ2 | P | t | P | ||
| Neurol event | 0.00 | .97 | −0.75 | .49 | |||||
| ALIF | OTLIF | Consistency | 2.09 | 0.34 to 13.00 | 0% | ||||
| MTLIF | OTLIF | Consistency | 3.51 | 0.18 to 70.19 | N/A | ||||
| OPLIF | OTLIF | Consistency | 3.10 | 0.28 to 34.57 | N/A | ||||
| MPLIF | OTLIF | AIC | 2.87 | 0.14 to 58.71 | N/A | ||||
| MTLIF | ALIF | AIC | 1.68 | 0.05 to 56.71 | N/A | ||||
| OPLIF | ALIF | Consistency | 1.49 | 0.13 to 16.36 | N/A | ||||
| MPLIF | ALIF | AIC | 1.37 | 0.07 to 27.86 | N/A | ||||
| OPLIF | MTLIF | AIC | 0.88 | 0.02 to 41.27 | N/A | ||||
| MPLIF | MTLIF | AIC | 0.82 | 0.01 to 57.35 | N/A | ||||
| MPLIF | OPLIF | Consistency | 0.92 | 0.15 to 5.69 | 0% | ||||
| Spinal event | 0.77 | .68 | −0.78 | .47 | |||||
| ALIF | OTLIF | Consistency | 1.12 | 0.31 to 4.03 | 43.7% | ||||
| MTLIF | OTLIF | Consistency | 2.39 | 0.73 to 7.84 | 0% | ||||
| OPLIF | OTLIF | Consistency | 2.67 | 0.74 to 9.67 | N/A | ||||
| MTLIF | ALIF | AIC | 2.14 | 0.38 to 11.96 | N/A | ||||
| OPLIF | ALIF | Consistency | 2.39 | 0.47 to 12.21 | N/A | ||||
| OPLIF | MTLIF | Consistency | 1.12 | 0.22 to 5.63 | N/A | ||||
| Vascular event | 0.52 | .47 | −1.82 | .21 | |||||
| ALIF | OTLIF | Consistency | 4.75 | 0.56 to 40.31 | 0% | ||||
| MTLIF | OTLIF | Consistency | 0.31 | 0.01 to 7.40 | N/A | ||||
| OPLIF | OTLIF | Consistency | 3.22 | 0.13 to 76.82 | N/A | ||||
| MTLIF | ALIF | AIC | 0.07 | 0.00 to 3.00 | N/A | ||||
| OPLIF | ALIF | AIC | 0.68 | 0.01 to 31.05 | N/A | ||||
| OPLIF | MTLIF | AIC | 10.28 | 0.12 to 906.80 | N/A | ||||
| Wound event | 0.43 | .81 | −2.08 | .76 | |||||
| ALIF | OTLIF | Consistency | 1.39 | 0.27 to 7.10 | 51.3% | ||||
| MTLIF | OTLIF | Consistency | 0.92 | 0.24 to 3.52 | 17.7% | ||||
| OPLIF | OTLIF | Consistency | 1.49 | 0.27 to 8.26 | N/A | ||||
| MPLIF | OTLIF | AIC | 0.15 | 0.00 to 4.56 | N/A | ||||
| MTLIF | ALIF | AIC | 0.66 | 0.09 to 4.92 | N/A | ||||
| OPLIF | ALIF | Consistency | 1.07 | 0.13 to 9.07 | N/A | ||||
| MPLIF | ALIF | AIC | 0.11 | 0.00 to 4.20 | N/A | ||||
| OPLIF | MTLIF | Consistency | 1.62 | 0.35 to 7.46 | 0% | ||||
| MPLIF | MTLIF | AIC | 0.16 | 0.01 to 4.64 | N/A | ||||
| MPLIF | OPLIF | Consistency | 0.10 | 0.00 to 1.99 | N/A | ||||
Abbreviations: AIC, adjusted indirect comparison; ALIF, anterior lumbar interbody fusion; CI, confidence interval; MPLIF, minimally invasive posterior lumbar interbody fusion; MTLIF, minimally invasive transforaminal lumbar interbody fusion; N/A, not applicable; OPLIF, open posterior lumbar interbody fusion; OTLIF, open transforaminal lumbar interbody fusion; RR, risk ratio.
Figure 4.
Ranking probability of (A) overall adverse event, (B) neural event, (C) spinal event, (D) vascular event, and (E) wound event. ALIF, anterior lumbar interbody fusion; MIS-PLIF, minimally invasive posterior lumbar interbody fusion; MIS-TLIF, minimally invasive transforaminal lumbar interbody fusion; OPLIF, open posterior lumbar interbody fusion; OTLIF, open transforaminal lumbar interbody fusion.
Spinal Event
There were 8 studies reported data on spinal event from 4 LIF procedures (OTLIF, ALIF, MIS-TLIF, and OPLIF).15-19,23,26,28 Network meta-analysis showed that the difference in spinal events was little among OTLIF, ALIF, MIS-TLIF, and OPLIF (Figure 3B). However, ALIF (RR 1.12, 95% CI 0.31 to 4.03), MIS-TLIF (RR 2.39, 95% CI 0.73 to 7.84), and OPLIF (RR 2.67, 95% CI 0.74 to 9.67) had higher point estimates when they were compared with OTLIF (Table 2). SUCRA provided similar trend. OTLIF had the highest SUCRA value and mean rank of safety (mean rank = 1.6; SUCRA = 80.8) followed by ALIF (mean rank = 1.9; SUCRA = 69.9), MIS-TLIF (mean rank = 3.2; SUCRA = 27.2), and OPLIF (mean rank = 3.3; SUCRA = 22.1; Supplementary File 10). Loop inconsistency test did not detect significant inconsistency in the network meta-analysis of spinal event rate (χ2 = 0.77; P = .68; Supplementary File 11), and Egger’s test detected no significant small study effects in the pooled estimate of spinal event rate (t = −0.78, 95% CI −2.36 to 1.23; Supplementary File 12).
Vascular Event
A total of 4 studies presented available data on vascular event in OTLIF, ALIF, MIS-TLIF, and OPLIF.15,18,19,26 Pooled estimate demonstrated no significant finding of vascular event rate among OTLIF, ALIF, MIS-TLIF, and OPLIF (Figure 3C; Table 2). Yet MIS-TLIF seems to cause lower vascular event rate than OTLIF (RR 0.31, 95% CI 0.01 to 7.40), ALIF (RR 0.07, 95% CI 0.00 to 3.00), and OPLIF (RR 0.10, 95% CI 0.00 to 8.58). In SUCRA, MIS-TLIF had the highest SUCRA value and mean rank of safety (mean rank = 1.5; SUCRA = 84.2) followed by OTLIF (mean rank = 2.1; SUCRA = 64), OPLIF (mean rank = 3.0; SUCRA = 32.5), and ALIF (mean rank = 3.4; SUCRA = 19.4; Supplementary File 13). No significant inconsistency was detected by loop inconsistency test in the network meta-analysis of vascular event rate (χ2 = 0.52; P = .74; Supplementary File 14), and no significant small study effects was detected by Egger’s test in the pooled estimate of vascular event rate (t = −1.89, 95% CI −13.29 to 5.40; Supplementary File 15).
Wound Event
There were 9 studies that reported data on wound event among OTLIF, ALIF, MIS-TLIF, OPLIF, and MIS-PLIF (Figure 3D).15-19,22,23,26,27 Pooled result showed that no significant difference in wound event rate among the 5 LIF procedures though MIS-PLIF seems to result in lower wound event rate than OTLIF (RR 0.15, 95% CI 0.00 to 4.65), ALIF (RR 0.11, 95% CI 0.00 to 4.20), MIS-TLIF (RR 0.16, 95% CI 0.01 to 4.64), and OPLIF (RR 0.10, 95% CI 0.00 to 1.99; Table 2). Similar trend could be observed in SUCRA. MIS-PLIF had the highest SUCRA value and mean rank of safety (mean rank = 1.5; SUCRA = 88.1), but mean ranks of the other 4 LIF procedures were very close to each other (Figure 4; Supplementary File 16). Loop inconsistency test showed no significant result in the network meta-analysis of wound event rate (χ2 = 0.43; P = .81; Supplementary File 17), and Egger’s test demonstrated no significant small study effects in the pooled estimate of neural event rate (t = −2.08, 95% CI −3.49 to 0.22; Supplementary File 18).
Discussion
Key Findings
To examine the comparative safety profile of MIS-TLIF, MIS-PLIF, OTLIF, OPLIF, and ALIF in patients with LDDD, we successfully synthesized 7 prospective cohort studies and 7 randomized clinical trials involving 921 participants to compare safety of the 5 LIF procedures for LDDD. The main finding of the present network meta-analysis is that OTLIF demonstrated the lowest rates of overall complications (including neurological, spinal, vascular, and wound events), comparted to other LIF procedures (Figure 2).
According to our network meta-analysis, the complications rate of OPLIF is significantly higher than that of OTLIF (RR 4.06; 95% CI 1.25 to 13.18). In addition, compared to MIS-TLIF, MIS-PLIF, and ALIF, OPLIF still demonstrates higher tendency of complications in spite of statistical insignificance. It came as no surprise because OPLIF had been reported to bear many complications, inclusive of nerve root injury, dural tear, and epidural adhesions,30,31 which are compatible with the fact that OPLIF also serves the highest rate of neurological events, including foot-drop, affections of left sympathetic plexus, and of spinal events in our further analysis. Because there is fewer retraction of the dura in TLIF technique from its lateral approach to the vertebral foramen, TLIF approach causes the least neurological events. Our meta-analysis and previous studies constantly support the theory.32,33
For the vascular events, including nonfatal pulmonary embolus, stroke, deep vein thrombosis, injury of the iliac vein, and postoperative hematoma, MIS-TLIF has the least chance to cause the complications compared to OPLIF; although it is not statistically different, such high RR of 10.28 deserves attention from clinical practitioners. Interestingly, this finding is consistent with our previous study showing that the operative time of MIS-TLIF is significantly longer than OPLIF (57.48 minutes; 95% CI 4.18 to 110.79), which reflects the fact that longer operation is directly related to an increased risk of thromboembolism.34 Moreover, ALIF is notorious for its vascular events due to its retroperitoneal approach to access the anterior spine with high probability to result in visceral and vascular injury,35-37 and it explains our finding that ALIF is the poorest approach with regard to vascular events.
In terms of wound events, defined as prolonged wound secretion, fat liquefaction of postsurgical incision, superficial and deep wound infection, MIS-PLIF contributes to better outcomes, followed by OTLIF, MIS-TLIF, ALIF, and OPLIF, though there is no statistically significant distinction among the comparisons. There is no astonishment that OPLIF has the greatest wound events owing to its approach involving dissection of the paraspinal muscle for the access to the posterior column of the vertebral body,12,38 which may prolong the wound recovery for its iatrogenic injury. On the other hand, both TLIF and ALIF diminish direct dissection of paraspinal muscles with its unilateral and anterior access, respectively.36 However, our results present a bizarre phenomenon that OTLIF has lower wound events than MIS-TLIF does and it could probably be attributed to relatively lower proficiency and experience of minimal invasive approach by surgeons compared to open approach since the OTLIF was first introduced in 1982 by Harms and Jeszenszky,39,40 which is way more earlier than MIS-TLIF was. For the same reason, PLIF is a traditional approach first described by doctor Cloward in 1953,41 and most spinal surgeons are well trained and much more familiar with this procedure, which could probably explain why MIS-PLIF has the best result. Nevertheless, we believe that as time goes by, with the increased volume of minimal invasive approach, MIS-TLIF will further decrease the wound events and may have the chance to surpass the OTLIF and MIS-PLIF.
Comparison With Previous Syntheses
This is the first network meta-analysis on comparative safety profile of PLIF, TLIF, and ALIF in patients with LDDD, yet our evidence is not the first synthesis in this field. Although some syntheses also investigated safety of LIF procedures before our study,32,33,42-44 few of them focused on LDDD.32 Pooling data from various populations usually leads to inappropriate estimate. For instance, one of them identified 29 studies for comparing efficacy and safety among ALIF, PLIF, TLIF, and lateral LIF,44 and it concluded that complication rates were similar between each 2 LIF procedures. However, the conclusion was based on highly heterogeneous results, and, for instance, I2 in pooled complication rate between ALIF and PLIF reached 83.3%. This may be associated with the fact that the synthesis did not separate MIS surgery from open surgery and they involved diverse demographics of patients with not only LDDD but also with post discectomy syndrome, spondylosis, stenosis, and spinal deformity. Furthermore, they only pooled data from the four LIF procedures in head-to-head meta-analysis.
Another synthesis appropriately specified population and comparators.32 It focused on the efficacy and safety of PLIF and TLIF on LDDD. Moreover, the meta-analysis clarified complications including nerve injury, wound infection, and graft malposition. Its conclusion mentioned that TLIF was superior to PLIF with lower incidence of complication (nerve root injury and dural tear). Unfortunately, the pooled result of overall complication was heterogeneous (I2 = 40%; P = .05). As in the meta-analysis of 2017 we mentioned above, this synthesis also simply pooled data without considering MIS and open surgery. In addition, the study admitted that its evidence may be limited because of data source. Using retrospective observational studies in meta-analysis possibly lead to imprecise estimate. Taken together, we designed our study to overcome potential bias from diverse population, mixed interventions (MIS and open surgery), and inadequate analysis. Our systematic review specified population with LDDD and clarified MIS surgery from open surgery. Then, our team member constructed 5-arm (ALIF, OTLIF, MIS-TLIF, OPLIF, and MIS-PLIF) consistency model for providing an overview of safety of common LIF procedures on LDDD.
Limitation
Our study has 2 main limitations though we tried to overcome some problems in previous syntheses. First, because our study would like to avoid inherent biases from retrospective studies, we only synthesized 14 studies with 921 cases. This sample size may lead to pooled estimates under power. In fact, we have expanded our literature by searching Web of Science in this update systematic review. Second, surgeon experience is very important in this topic, especially in clinical practice, but we did not find enough information in the included studies. We anticipate that future studies on this topic provide sufficient information about surgical team.
Conclusions
Our evidence reveals that perhaps OPLIF should be avoided in the management of LDDD because it confers significantly higher overall adverse event rate. Moreover, TLIF seems to have the safest profile in terms of neural, spinal events, and vascular evens. Nevertheless, our previous work found that MIS-PLIF and OPLIF may have better outcomes in terms of pain relief and Oswestry Disability Index.13 Therefore, shared decision making may be an appropriate approach to choose LIF procedure for LDDD before surgery. Our evidence only focuses on the most common LIF procedures, and we anticipate further studies taking lateral LIF, extreme lateral LIF, and oblique LIF into analysis though these LIF procedures are not popular in clinical practice now. A comprehensive comparison of LIF procedures will improve decision of LIF surgery.
Supplemental Material
Supplemental Material, Appendix for Safety of Lumbar Interbody Fusion Procedures for Degenerative Disc Disease: A Systematic Review With Network Meta-Analysis of Prospective Studies by Kuan-Yu Chi, Shih-Hao Cheng, Yu-Kai Kuo, En-Yuan Lin and Yi-No Kang in Global Spine Journal
Footnotes
Author Contributions: KYC: Conception of the work, interpretation of data, drafting the work, and final approval of the version to be published.
SHC: Supervision of the research, critical revision of the draft for enhancing crucial intellectual content, and final approval of the version to be published.
YKK: The acquisition of data and final approval of the version to be published.
EYL: Interpretation of data, revising draft critically for important intellectual content, and final approval of the version to be published.
YNK: Design of the work, the acquisition of data, analysis, interpretation of data, revising draft critically for important intellectual content, and final approval of the version to be published.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Shih-Hao Cheng, MD  https://orcid.org/0000-0001-8579-8792
https://orcid.org/0000-0001-8579-8792
Yi-No Kang, MA  https://orcid.org/0000-0001-8244-2846
https://orcid.org/0000-0001-8244-2846
Supplemental Material: Supplemental materials for this article is available online.
References
- 1. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363–370. [DOI] [PubMed] [Google Scholar]
- 2. Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine (Phila Pa 1976). 1999;24:1813–1819. [DOI] [PubMed] [Google Scholar]
- 3. Cypress BK. Characteristics of physician visits for back symptoms: a national perspective. Am J Public Health. 1983;73:389–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoy D, Bain C, Williams G, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64:2028–2037. [DOI] [PubMed] [Google Scholar]
- 5. Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385:549–562. [DOI] [PubMed] [Google Scholar]
- 6. Wolfe F. Determinants of WOMAC function, pain and stiffness scores: evidence for the role of low back pain, symptom counts, fatigue and depression in osteoarthritis, rheumatoid arthritis and fibromyalgia. Rheumatology (Oxford). 1999;38:355–361. [DOI] [PubMed] [Google Scholar]
- 7. Choi YS. Pathophysiology of degenerative disc disease. Asian Spine J. 2009;3:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yong-Hing K, Kirkaldy-Willis WH. The pathophysiology of degenerative disease of the lumbar spine. Orthop Clin North Am. 1983;14:491–504. [PubMed] [Google Scholar]
- 9. Saleem S, Aslam HM, Rehmani MAK, Raees A, Alvi AA, Ashraf J. Lumbar disc degenerative disease: disc degeneration symptoms and magnetic resonance image findings. Asian Spine J. 2013;7:322–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Phillips FM, Slosar PJ, Youssef JA, Andersson G, Papatheofanis F. Lumbar spine fusion for chronic low back pain due to degenerative disc disease: a systematic review. Spine (Phila Pa 1976). 2013;38:E409–E422. [DOI] [PubMed] [Google Scholar]
- 11. Dunn R. Lumbar fusion–indications and surgical options. SA Orthop J. 2008;7:8–12. [Google Scholar]
- 12. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 2015;1:2–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lin EY, Kuo YK, Kang YN. Effects of three common lumbar interbody fusion procedures for degenerative disc disease: a network meta-analysis of prospective studies. Int J Surg. 2018;60:224–230. [DOI] [PubMed] [Google Scholar]
- 14. Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–171. [DOI] [PubMed] [Google Scholar]
- 15. Crandall DG, Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine (Phila Pa 1976). 2009;34:2126–2133. [DOI] [PubMed] [Google Scholar]
- 16. Klara P, Freidank S, Rezaiamiri S. Comparison of lumbar interbody fusion techniques using ray threaded fusion cages and pedicle screw fixation systems. Neurosurg Q. 2003;13:20–29. [Google Scholar]
- 17. Parker SL, Mendenhall SK, Shau DN, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg. 2014;82:230–238. [DOI] [PubMed] [Google Scholar]
- 18. Cheng X, Zhang K, Sun X, et al. Clinical and radiographic outcomes of bilateral decompression via a unilateral approach with transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis with stenosis. Spine J. 2017;17:1127–1133. [DOI] [PubMed] [Google Scholar]
- 19. Shunwu F, Xing Z, Fengdong Z, Xiangqian F. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976). 2010;35:1615–1620. [DOI] [PubMed] [Google Scholar]
- 20. Kim HJ, Kang KT, Chun HJ, et al. Comparative study of 1-year clinical and radiological outcomes using robot-assisted pedicle screw fixation and freehand technique in posterior lumbar interbody fusion: a prospective, randomized controlled trial. Int J Med Robot. 2018;14:e1917. [DOI] [PubMed] [Google Scholar]
- 21. Kulkarni AG, Bohra H, Dhruv A, Sarraf A, Bassi A, Patil VM. Minimal invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion. Indian J Orthop. 2016;50:464–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lee N, Kim KN, Yi S, et al. Comparison of outcomes of anterior, posterior, and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg. 2017;101:216–226. [DOI] [PubMed] [Google Scholar]
- 23. Lin B, Lin QY, He MC, Liu H, Guo ZM, Lin KS. Clinical study on unilateral pedicle screw fixation and interbody fusion for the treatment of lumbar degenerative diseases under Quadrant system [in Chinese]. Zhongguo Gu Shang. 2012;25:468–473. [PubMed] [Google Scholar]
- 24. Jian X, An-Min J, Xiao-Ping S, Yan-Bin W, Wei-Yong X. Clinical outcomes of unilateral lumbar pedicle screw combined with translamina facet screw fixation versus bilateral fixation. Chin J Tissue Eng Res. 2013;17:1571–1578. [Google Scholar]
- 25. Hartwig T, Strube P, Hoff E, Groß C, Perka C, Putzier M. Prospective randomized comparison between single-level transforaminal (TLIF), posterior (PLIF) and anterior stand alone (ALIF) lumbar interbody fusion regarding qualitative and quantitative radiologic changes of the paraspinal muscles and clinical parameters. Eur Spine J. 2010;19:1977. [Google Scholar]
- 26. Hoff EK, Strube P, Pumberger M, Zahn RK, Putzier M. ALIF and total disc replacement versus 2-level circumferential fusion with TLIF: a prospective, randomized, clinical and radiological trial. Eur Spine J. 2016;25:1558–1566. [DOI] [PubMed] [Google Scholar]
- 27. Putzier M, Hartwig T, Hoff EK, Streitparth F, Strube P. Minimally invasive TLIF leads to increased muscle sparing of the multifidus muscle but not the longissimus muscle compared with conventional PLIF—a prospective randomized clinical trial. Spine J. 2016;16:811–819. [DOI] [PubMed] [Google Scholar]
- 28. Rodríguez-Vela J, Lobo-Escolar A, Joven E, Muñoz-Marín J, Herrera A, Velilla J. Clinical outcomes of minimally invasive versus open approach for one-level transforaminal lumbar interbody fusion at the 3- to 4-year follow-up. Eur Spine J. 2013;22:2857–2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee LY, Idris Z, Beng TB, et al. Outcomes of minimally invasive surgery compared to open posterior lumbar instrumentation and fusion. Asian J Neurosurg. 2017;12:620–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. DiPaola CP, Molinari RW. Posterior lumbar interbody fusion. J Am Acad Orthop Surg. 2008;16:130–139. [DOI] [PubMed] [Google Scholar]
- 31. Talia AJ, Wong ML, Lau HC, Kaye AH. Comparison of the different surgical approaches for lumbar interbody fusion. J Clin Neurosci. 2015;22:243–251. [DOI] [PubMed] [Google Scholar]
- 32. Lan T, Hu SY, Zhang YT, et al. Comparison between posterior lumbar interbody fusion and transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: a systematic review and meta-analysis. World Neurosurg. 2018;112:86–93. [DOI] [PubMed] [Google Scholar]
- 33. Zhang Q, Yuan Z, Zhou M, Liu H, Xu Y, Ren Y. A comparison of posterior lumbar interbody fusion and transforaminal lumbar interbody fusion: a literature review and meta-analysis. BMC Musculoskelet Disord. 2014;15:367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kim JY, Khavanin N, Rambachan A, et al. Surgical duration and risk of venous thromboembolism. JAMA Surg. 2015;150:110–117. [DOI] [PubMed] [Google Scholar]
- 35. Malham GM, Parker RM, Ellis NJ, Blecher CM, Chow FY, Claydon MH. Anterior lumbar interbody fusion using recombinant human bone morphogenetic protein-2: a prospective study of complications. J Neurosurg Spine. 2014;21:851–860. [DOI] [PubMed] [Google Scholar]
- 36. Mobbs RJ, Phan K, Daly D, Rao PJ, Lennox A. Approach-related complications of anterior lumbar interbody fusion: results of a combined spine and vascular surgical team. Global Spine J. 2016;6:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, Jacobs GB. Visceral and vascular complications resulting from anterior lumbar interbody fusion. J Neurosurg. 1999;91(1 suppl):60–64. [DOI] [PubMed] [Google Scholar]
- 38. Madhu TS. Posterior and anterior lumbar interbody fusion. Orthop Trauma. 2008;22:406–413. [Google Scholar]
- 39. de Kunder SL, Rijkers K, Caelers IJMH, de Bie RA, Koehler PJ, van Santbrink H. Lumbar interbody fusion: a historical overview and a future perspective. Spine (Phila Pa 1976). 2018;43:1161–1168. [DOI] [PubMed] [Google Scholar]
- 40. Harms JG, Jeszenszky D. Die posteriore, lumbale, interkorporelle Fusion in unilateraler transforaminaler Technik. Orthop Traumatol. 1998;10:90–102. [DOI] [PubMed] [Google Scholar]
- 41. Cloward RB. The treatment of ruptured lumbar intervertebral discs; criteria for spinal fusion. Am J Surg. 1953;86:145–151. [DOI] [PubMed] [Google Scholar]
- 42. Khan NR, Clark AJ, Lee SL, Venable GT, Rossi NB, Foley KT. Surgical outcomes for minimally invasive vs open transforaminal lumbar interbody fusion: an updated systematic review and meta-analysis. Neurosurgery. 2015;77:847–874. [DOI] [PubMed] [Google Scholar]
- 43. Qin R, Liu B, Zhou P, et al. Minimally invasive versus traditional open transforaminal lumbar interbody fusion for the treatment of single-level spondylolisthesis grades 1 and 2: a systematic review and meta-analysis. World Neurosurg. 2019;122:180–189. [DOI] [PubMed] [Google Scholar]
- 44. Teng I, Han J, Phan K, Mobbs R. A meta-analysis comparing ALIF, PLIF, TLIF and LLIF. J Clin Neurosci. 2017;44:11–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Appendix for Safety of Lumbar Interbody Fusion Procedures for Degenerative Disc Disease: A Systematic Review With Network Meta-Analysis of Prospective Studies by Kuan-Yu Chi, Shih-Hao Cheng, Yu-Kai Kuo, En-Yuan Lin and Yi-No Kang in Global Spine Journal