ABSTRACT
Mobile-based applications are popular and prevalently used in the US population. Applications focusing on nutrition offer platforms for quantifying and changing behaviors to improve dietary intake. Such behavior changes can intervene in the relation of diet to promote health and prevent disease. Mobile applications offer a safe and convenient way to collect user data and share it back to users, researchers, and to health care providers. Other lifestyle factors like activity, sleep, and sedentary behavior, can also be quantified and included in investigations of how lifestyle is related to health. Yet, challenges in the assessment offered through mobile applications and effectiveness to change behavior still remain, including rigorous evaluation, demonstration of successful health improvement, and participant engagement. The data mobile applications generate, however, expands opportunities for discovery of the integrated and time-based nature of various daily activities in relation to health. This article is a summary of a symposium at Nutrition 2020 Live Online on the role of mobile applications as a tool for nutrition research and health promotion. The types and capabilities of mobile applications, challenges in their evaluation and use in research, and opportunities for the data they generate along with a specific example, are reviewed.
Keywords: mobile-based, technology, nutrition, health promotion, applications, prevention, dietary assessment, mobile health, image-based, nutrition interventions
Mobile based applications are a tool for nutrition research and health promotion that are contrasted with traditional methods and their challenges and opportunities explored in this paper.
Introduction
The American Society for Nutrition sponsored a symposium at Nutrition 2020 Live Online on the role of mobile phones as a tool for nutrition research and health promotion. This overview summarizes the traditional context for nutrition research and the new capabilities that mobile applications offer to quantify dietary intake, behavior, environment, lifestyle, and their link with health outcomes. The opportunities for assessment and interventions using mobile applications are reviewed herein with a description of strengths and potential pitfalls. An in-depth example of the data opportunities presented by mobile-based applications is also featured.
Mobile devices offer new ways to quantify dietary behaviors and potentially inform the diet-health relation. Patterns of intake of nutrients, energy, and other dietary components over time can be measured and shared with mobile device users, researchers, and health care providers. In addition, culture and environment impact dietary behavior and are influential to both diet and health. Other lifestyle factors like activity, sleep, sedentary behavior, and their interplay over time may modify the effects of diet to health (Figure 1). Historically, few tools have been available to quantify the complexity of these varying factors simultaneously nor to consider their integration. Most data have been self-reported, and knowledge of assessment is also known to change behavior and bias self-reported information. Interventions to promote healthy dietary intake have also been limited to in-person sessions with a health provider, educator, or support group. Adherence, similar to data collection, has generally been self-reported. Mobile devices have the capacity to quantify all of these aspects in real time and create new platforms for interventions.
FIGURE 1.
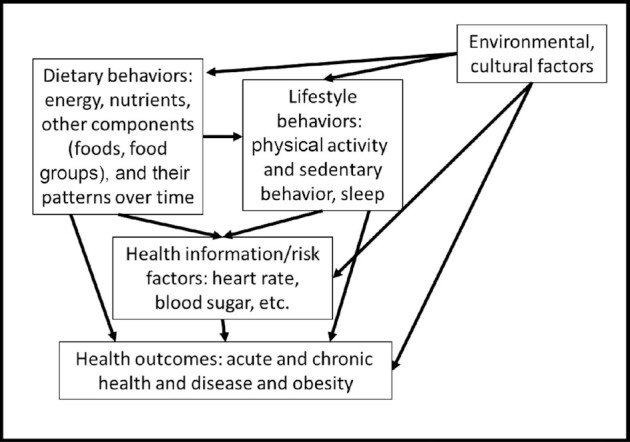
Factors and behaviors with influence on health outcomes.
In recent years, mobile applications have become extremely popular. Smartphone ownership is highly prevalent (>75%), particularly among young adults (92%), of all race/ethnicities (77% white, 72% black, and 75% Hispanic) (1) and even amongst low-income populations (>60%) (2, 3). About 77% of smartphone users download apps (4), with an average of 88.7 apps downloaded per person, and 7.6 used on a daily basis (5). Also, about 59% of smartphone users had downloaded health mobile apps, such as fitness and nutrition apps (6). The storage and recording capacity of apps enables participants to access the information on their phones at any time, anticipating frequent use to find needed information in a timely fashion. Therefore, although the opportunity for practical use of mobile apps to enhance nutrition research is high, consideration of the challenges and research gaps may guide future advances.
Mobile-based nutrition applications
Several different types of mobile apps related to diet and nutrition exist. In a wide search of the available mobile apps related to diet and nutrition performed in May 2020, we found 4 general categories of classification, those that: track consumption; score foods; generate a meal plan; and generate a healthy grocery list. We conducted a thorough search of the available apps for android phones and for iOS to quantify the number of apps using the following keywords: “track consumption”; “score foods”; “meal or diet plan”; and “healthy grocery list.” We reviewed each app to determine if it would fit into these 4 categories. We found that the availability of these various types of apps vary considerably, with >200 apps to track consumption available for android phones, whereas for iOS, we found <10 apps. For scoring foods, we found ∼100 apps for androids and only 2 for iOS. For generating a diet plan, we found ∼220 apps for androids and only ∼6 for iOS. Finally, for apps that generate a healthy grocery list, we found ∼30 for androids and only 2 for iOS.
Among the apps that track consumption (Figure 2), most of these allow users to input personal and health information, such as age, gender, current weight, level of physical activity, and other information to calculate personalized energy and nutrient requirements and based on input of what they consumed in the day, the app tracks if their caloric intake and intake of other nutrients is above or below the recommendation. With this information, users may adjust their diet to align with such recommendations. Some apps also provide specific recommendations and feedback on which food groups to cut back or which to increase. Other apps add the tracking of physical activity and estimate caloric balance to help users reach a specific goal; this goal could be to reduce weight or to gain weight, particularly in the case of athletes. In addition, some apps connect with or allow a dietitian to view the results and to provide feedback. Furthermore, some apps allow or encourage image capture of the food to be consumed before intake or before and after intake to allow estimation of the portion consumed, although the use of images to classify foods and to calculate the serving size is still in development. A few popular examples of these types of apps are MyFitnesspal, Fooducate, Sparkle People, Argus, Fat Secret, MyNetDiary, and Lose It.
FIGURE 2.
Examples of mobile applications that track consumption.
There are also apps that score foods to attempt to quantify their healthfulness (Figure 3). The scoring is based on certain attributes of the food or meal compared with a particular guideline, algorithm, or commercial diet. For some users, this scoring system may be helpful as it translates energy and nutrient composition information of that food to a single score with practical relevance. The drawback may be that the simple scoring of foods may prioritize certain nutrients or calories which may be of lesser importance compared with others for that individual. Some apps expand the comprehensiveness of their scoring system to include other information, such as dietary preferences, age, gender, level of processing and additives, first ingredient in the food, and even the environmentally friendliness of the product. Examples of these types of apps include Fooducate, Shopwell, GoodGuide, Smart - Food Score Calculator, Food score calculator, and Snackability.
FIGURE 3.
Examples of mobile applications that score foods.
The next category are apps that generate a meal plan (Figure 4). These apps recommend certain meals to consume depending on the goal of the user, such as healthy meals, vegetarian meals, gluten-free meals, etc. Some apps in this category generate a detailed meal plan including specific foods to consume for each meal or how to distribute food intake throughout the day. For each meal suggested in the app, the caloric and nutritional composition is included. Some apps in this category organize the recipes and the meals for the week. Others provide meal plans for a variety of caloric level goals. A few popular examples of these types of apps include Mealime, Food Planner, Paprika, Plate Joy, Make My Plate, and Meal Board.
FIGURE 4.
Examples of mobile applications that generate a diet plan.
Lastly, there are apps that generate a grocery list for the target diet (Figure 5). Many of the apps described in the previous categories do this based on the recipe chosen. But there are other apps that generate a healthy grocery list based on the energy and nutrient requirements of the user. Some apps explore connecting to an online store for grocery delivery. Examples include MyNutriCart, Eat This Much, Mealime, Make My Plate, and Plate Joy.
FIGURE 5.
Examples of mobile applications that generate a healthy grocery list.
Evaluation of mobile applications
Although there is high usage of health-related apps (6), we found through a PubMed review of studies published from 2013 to May 2020 that most of the apps mentioned in the previous section have not been properly evaluated. In this search, we specifically found a total of 17 apps that were evaluated through research, which included 4 developed by industry, 10 developed by researchers, and 3 developed in partnership between researchers and industry. This lack of evaluation may hinder the intended use of these apps as users may not know which ones are effective at aiding participants to achieve their desired outcomes or at quantifying dietary intake. In fact, there is limited guidance to identify which are effective in promoting healthy dietary behaviors. Previously published systematic reviews have found that effective apps in changing dietary behaviors have used a combination of techniques to achieve this, such as “providing instructions” (used in ∼70–80% of the apps), “providing general encouragement” (used in ∼70% of the apps), “providing contingent rewards” (used in ∼70% of the apps), “providing feedback on performance” (used in ∼50% of the apps), and “prompting self-monitoring” (used in 45–60% of the apps) (7, 8). Other systematic reviews reported that behavior change techniques were mainly utilized in the app interventions on nutrition behaviors and related health outcomes, including goal setting, feedback and self‐monitoring, shaping knowledge (information), and social support, which showed positive outcomes on individual and group‐based interventions (9). These behavioral change techniques connect to the constructs of nutrition education theories, such as observational learning, knowledge and skill to perform behavior, attitude, intention, goal setting, feedback on performance, self-efficacy, self-monitoring, self-regulation, and social support. These are all integrated to develop theory-based app interventions to reduce barriers, increase motivation and adherence, and facilitate behavior change. Also, app engagement, app use, and education had a significantly positive association with behavior change (10). However, despite the app interventional frameworks being grounded in behavior change theories, evaluation for effectiveness is a limitation.
Apps that monitor dietary intake: only a few studies have evaluated these types of apps for improving diet and/or body weight (11–26). For example, MyFitnessPal, a popular app designed by software engineers in collaboration with dietitians using an evidence-based and theory-based approach to weight loss, was evaluated for 6 mo in overweight adults (27). No significant difference between intervention and control groups was found for weight change. The TXT2BFiT app, which encourages self-monitoring of dietary intake, was evaluated in young adults with a high risk of weight gain (28). After 12 wk, there was a significant reduction in weight, sugar-sweetened beverage intake, energy-dense meals, and increased vegetable consumption as compared to a control group. The eBalance app, an app to monitor dietary intake and physical activity with real-time feedback on caloric intake and expenditure, was evaluated among healthy adults (29). The intervention group significantly lost weight and significantly increased their diet quality scores, knowledge scores, and success scores (score for maintaining a healthy lifestyle) compared with the control group. The My Meal Mate app, which was developed by researchers using an evidence-based behavioral approach, was also evaluated in overweight adults (20). BMI change at 6 mo was significantly greater in the intervention compared with those using a website to monitor diet. Another study evaluated the Mobile Food Record app, an app that easily records intake by taking pictures of the foods and beverages consumed, among young adults (30). There was a significant weight reduction in men and in sugary beverage intake in women in the app group compared with the control group. The Mobile Phone-Based Diabetes Prevention Program was also evaluated among overweight adults (15). The app allows for self-monitoring of weight, activity, and caloric intake but no significant improvements in food intake were found compared with the control group. Other apps to monitor diet have also found improvements in dietary patterns (16, 31, 32).
Apps that generate a meal plan: we found very limited studies that evaluated such apps. A study evaluated the SmartLoss app, an app developed based on the planned behavior, reasoned action, and social cognitive theories that includes a diet plan, goal setting, weight change monitoring, and automated feedback, in young healthy adults (33). After 12 wk, weight loss was significantly larger in the app group compared with the control group.
Apps that score foods: we found limited studies that evaluated such apps. The Snack Track School is an app developed by researchers to present a virtual high-school environment with a personal snack track tool and goal settings, for adolescents to search and select their snack based on a score (34). Evaluation among a large sample of adolescents revealed no significant positive intervention effects on the healthy snack ratio. Another study pilot tested the Snackability app, an app that scores snacks based on the USDA guidelines for healthy snacks, among 20 college students (23). Students reported that the app was a good way to help them select and consume healthy snacks and had high user ratings for feasibility, usability, and acceptability.
Apps that generate a healthy grocery list: similarly, we found limited studies that evaluated such apps. One of these studies evaluated MyNutriCart app, an app that generates a healthy grocery list based on the caloric and nutrient requirements of the household (24), among overweight adults for 3 mo (22). There were significant improvements in household purchasing, in individual intakes, and in the individual frequency of intake of certain healthy foods within the intervention group (P < 0.05) but no significant differences were found compared with the control group.
Capabilities of traditional versus mobile-based nutrition research and intervention
The ubiquitous carrying and use of mobile devices by nearly all in the population has normalized digital monitoring and recording behaviors. As a result, including similar behaviors in protocols for research participants does not feel unique to research but rather, integrates easily to “normal” daily activities in a free-living context. Mobile app monitoring throughout the day allows for more comprehensive recording and communication with participants compared with traditional methods of relying on memory, paper-pencil recording, photographs, or communication via phone calls. Thus, mobile-based nutrition applications foster an expansive potential for research and intervention delivery. An added potential exists for self-monitoring behaviors related to nutrition and health and provision of this information to health care providers (35). Although some traditional nutrition research and interventions have provided information on dietary behavior and health back to participants and providers, no additional automated platforms have been available for individualized health monitoring (Table 1).
TABLE 1.
Capabilities of traditional versus mobile-based nutrition research and intervention
| Traditional | Mobile-based | |
|---|---|---|
| Assessment method | Paper and pencil or interview | Cell-phone application |
| Communication | Researchers | Participant, researchers, health care providers |
| Goals | Research (estimate intake, dietary adherence, link to health) | Research and individualized health monitoring |
| Assessment capability | Self-reported diet and lifestyle behaviors, environmental factors, times | Image-based and automated capture of diet and lifestyle behaviors, health, environmental factors, timestamped |
| Dietary assessment user burden | Up to 45 min per dietary assessment | Potential for quick image capture with machine learning from user input |
| Time to process and use data | Weeks to months | Potentially real time |
| Dietary assessment accuracy | Up to 30% error and estimation difficulty | Similar or better than 30% error, limited estimation with image capture |
| Researcher burden | Time consuming, erroneous data processing and transfer | Limited time, potential for automated processing |
| Interventions | Resource-intensive, often involve face-to-face or phone contact | Automated, electronically delivered, potential automated reminders, and compliance monitoring |
Along with “who” monitoring of nutrition- and health-related behaviors may be shared with, the assessment capabilities are also enhanced in mobile-based applications compared with traditional assessment. With regards to dietary intake, images may be used to capture types and amounts of food and beverages before and after dietary intake, as described above (36). Although these images are still self-reported, objectivity is improved with the presence of image capture (36). Other data recorded may include timestamps, location, additional information about the environment, who is present, lifestyle factors, and other health information (heart rate, activity monitoring, blood sugar, etc.) occurring simultaneously. The capture of these assessments may also allow indirect quantification of other important lifestyle factors without input from the individual, for example deriving sleep duration from activity and heart rate (37). In contrast, traditional assessment for many of these nutrition- and health-related factors was reliant on self-reports with a heavy estimation burden making the capture of so many diverse factors that occurred simultaneously unrealistic to assess.
The time required to report behaviors represents another capability for dramatic improvement using mobile applications compared with traditional methods. Automated assessment, as in the integration of activity monitors with mobile-based applications, are possible for some data capture without time or extra effort on the part of the participant (38). In other cases, the speed of assessment is enhanced, for example, image capture of dietary intake either paired with automated food identification or expert review, may shorten the time to complete dietary assessment from 45 min for recording dietary intake in a day to 10 min or less to capture images before and after eating. Machine learning from user input may also minimize user burden over time as the daily habits of the participant are captured, the system may predict upcoming assessment occasions and simply require review or confirmation. Similarly, the time required for researchers to prepare the data may be reduced using mobile-based compared with traditional nutrition assessment methods. Electronic data capture can be sent to a server where automated processing transforms the data to uniform digital records ready for analysis (39).
Errors influence the accuracy of the data and represent another construct that may be improved using mobile-based applications compared with traditional methods for nutrition assessment in research. Errors in memory, bias related to reporting undesirable behaviors or self-perceived “nonnormal” behaviors, and inaccuracy in amount estimation are all common in traditional self-reported assessment. Conversely, bias related to over-reporting desirable behaviors may also exist. Estimation of amount may be difficult to conceptualize. Sometimes estimation of the average amount over a period of time is requested presenting a further challenge. Up to 30% error in calculating total energy has been estimated in various studies of traditional recall (36, 40). Similar errors may not be completely avoidable in mobile-based assessment as participants may still need to take images of food or report on how much they consumed. However, evaluation of accuracy using mobile apps has shown similar or better estimates of error in participant records compared with traditional dietary assessment (36, 40). Errors may also be avoided on the researcher side of collecting mobile data. Traditional forms of assessment include human input or transfer of data from one form to another that are rife with opportunities where error may influence record keeping. Sometimes multiple steps of data processing are required for preparation before analysis, and in each step additional errors may be accrued.
The time from assessment to data use or to data feedback may be dramatically shortened with mobile-based compared with traditional nutrition research. Mobile platforms can collect assessments and instantaneously send information to a server where it may be processed and sent to researchers, users, and health care providers. The potentially real-time use of data allows for enhanced research capacity, monitoring adherence to study protocol, and potential correction before exclusion is necessary. Similarly, opportunities for intervention while individuals are engaging in certain behaviors is possible as constant monitoring in real time allows for detection of the behavior and alert or communication back to the individual as a reminder to change the behavior.
Another opportunity for mobile applications is intervention delivery and advancing the measure of adherence to intervention protocols. Traditional nutrition interventions have several limitations that can be overcome using mobile-based interventions. For example, traditional nutrition interventions are resource-intensive, often including face-to-face contacts that entail expense to participants and investigators with generally low participant compliance (41). These interventions are often not sustainable over time or easily translatable to the community or health care settings, where time and resources are limited. Leveraging technology in interventions could overcome barriers in research as they eliminate the need for face-to-face interviews, making these interventions more cost-effective and easier to translate to other settings. Also, using mobile apps may improve retention and compliance compared with those not using an app (20, 41).
Considering all of these facets of nutrition research and interventions, mobile-based nutrition applications offer new discovery and potential to improve health. The simultaneous collection of multiple types of dietary, lifestyle, and health information in addition to contextual information on the environment, timing, and duration of activities, and the movement of individuals over space and time and in real time provides new horizons to explore regarding the relation of how these multiple factors influence behavior and health. Yet, there are also challenges.
Challenges in using diet mobile apps in research
Lack of user ratings and experiences: most apps are not evaluated for user ratings and experiences. It is important to understand how users engage with these health apps. Apps that promote healthy lifestyles or promote smoking cessation in which they engage participants and provide personalized feedback have shown to improve user engagement and adherence (29, 42). However, few studies have evaluated if user rating and experience with the app is correlated to the quality of the app. A survey among various experts to rate 137 patient-facing mHealth apps found that consumers' ratings were poor indications of apps' perceived quality. Therefore, more research is needed relating nutritional apps user rating and quality (43).
Compliance issues: several studies have shown that health-related mobile apps have a 30-d threshold use. This means, that after 30 d, the use of the app starts declining (44). A cross-sectional study on the use of the Lose It! app among 1,011,008 users found that the average length of engagement with the app was 29 d, varying from 3.5 to 172 d (45). The study evaluating the eBalance app found that the frequency of app use was 2.7 (SD 1.9) d/wk and the adherence rate was 56% (29). A review of web-based interventions found that the general adherence rate to mobile apps was about 50% (46). Another study using a self-monitoring app for vegetable intake showed that app engagement declined over time which limited the overall usage and intervention effectiveness (41). Similarly, the study evaluating the MyFitnessPal found that most users reported high satisfaction but logins dropped sharply after the first month (33). Also, the study evaluating the Snack Track School found that only 268 adolescents started using the app, of whom only 55 (21%) still logged in after 4 wk (47).
Lack of personalized feedback and support: feedback improves user engagement and adherence (29, 41, 45). Also, social support can help achieve behavioral changes (48). Often, studies personalized the feedback separately through social media or short text messages, and did not integrate the feedback to the app. Studies suggested that personal support with the app and tailored or personalized incentives matched with user preference are important to increase the adherence which, in turn, would probably improve outcomes even more. The more the app was personalized, the more users engaged. However, more studies validating these app components are needed.
An example of integrating data to inform health for future data collection from mobile apps
The many new opportunities presented in assessment and intervention using mobile-based applications expand possibilities for discovery in the diet-health relation. Simultaneous measure of multiple dietary, health, and environmental factors and how these may change over time bring the aspect of timing of these behaviors and activities to the forefront as the uniting continuum of their relations. The timing of dietary intake and other lifestyle behaviors has recently received greater attention as an important factor in health. For example, with regard to dietary intake, breakfast-skipping behavior and dietary intake later in the day has been linked with poor metabolic alterations (49, 50) and increased risk of diabetes type 2 (51–54). Physical activity is another behavior that occurs throughout the day and for which time may be an important factor to its link with weight and metabolic control (55, 56). Several studies have evaluated the relation of health with the timing of exercise relative to a single meal or over a single day (57–62). A recent review of the joint consideration of the timing of dietary intake and physical activity showed that exercise performed after a meal throughout the day had a beneficial impact on postprandial glycemia and supports hypotheses that the timing of multiple health behaviors may be important in a relation to health, or may link to health synergistically in ways that their independent consideration does not reveal (63, 64).
The data available from mobile-based assessment and monitoring may be utilized to integrate behaviors such as dietary intake and physical activity along with other important lifestyle factors such as sleep, sedentary behavior, and emotional factors that may be related to health like anger, fear, anxiety, contentedness, relaxation, and others which could also be quantified using heart rate or other bioindicators. Further, the duration, amount, or quality of these factors may also be quantified and integrated to patterning the data. Yet, few attempts have been made to integrate lifestyle behaviors over time despite the data currently being generated from mobile-based applications.
An example of integrating multiple aspects of dietary behavior to create temporal dietary patterns, however, was contributed by Eicher-Miller et al. (65) and Aqeel et al. (66). The distribution of time was used as a uniting factor to temporally pattern dietary intake, specifically the amount (kcal) of energy per eating occasion, the sequence of eating occasions, and their frequency over a 24-h day. The results showed that temporal dietary patterns characterized by moderate and proportionally equivalent energy consumed at evenly spaced eating events throughout a 24-h day were associated with higher dietary quality among US adults aged 20–65 y (1627) compared with participants exhibiting other temporal dietary patterns (65). Evaluation of these temporal dietary patterns with health outcomes (66) showed further benefits for the adults with patterns of evenly spaced and energy-balanced eating events in a 24-h day. This group had statistically significant and clinically meaningful lower mean BMI (P < 0.0001), waist circumference (P < 0.0001), and 75% lower odds of obesity compared with 3 other groups representing patterns with more dramatic energy peaks either earlier or later in the day (66). This study provided evidence that incorporating time with other aspects of a dietary pattern is related to health status and holds promise for further integration of lifestyle factors.
Temporal physical activity patterns were also created (67) using activity counts, representing the intensity of physical activity, captured throughout a 24-h day with physical activity accelerometers (n = 1999 adults 20–65 y). The group with a temporal physical activity pattern of high physical activity counts later in the day (between 16:00 and 21:00), had lower mean BMI (P < 0.001), waist circumference (P < 0.01), and 60% lower odds of obesity relative to normal weight status (OR: 0.4; 95% CI: 0.2, 0.8), compared with the group with the lowest activity counts throughout the day. Another group had high activity counts earlier in the day (between 08:00 and 11:00) and lower BMI and waist circumference compared to those formerly mentioned with the lowest activity counts (both P < 0.05). Thus, significantly lower mean BMI and waist circumference were associated with adults who had temporal physical activity patterns of higher activity counts performed early or late in the day compared with adults with a temporal pattern with the lowest physical activity counts (67).
Finally, the temporal patterns of diet and physical activity were integrated to form joint temporal dietary and physical activity patterns in 1836 adults aged 20–65 y (68). Results showed that a cluster, representing joint temporal dietary and physical activity patterns with proportionally equivalent average energy consumed at 2 main eating occasions (at 13:00 and 20:00), and high physical activity counts, had significantly lower BMI (P < 0.0001), waist circumference (P = 0.0002), total cholesterol (P = 0.01), and odds of obesity (OR = 0.26, P < 0.0001) compared to a cluster with greater energy consumed at 2 main eating occasions (at 13:00 and 20:00), and low physical activity counts. The temporally and jointly patterned sequence of diet and physical activity throughout a 24-h day had significant associations to BMI, waist circumference, total cholesterol, and obesity (68). The integration of multiple types of lifestyle factors like diet and physical activity is possible and has a relation with health, holding promise for the future development of lifestyle patterns that integrate additional temporal and contextual activities.
This example of integrating dietary and activity data in time could be expanded to integrate other time-bound behaviors and health data or status indicators. Expansion of the patterns over multiple days and periods is another area that requires investigation and is likely to yield important discoveries as it is behaviors over years that lead to chronic health conditions. Clarification of the role of the timing and duration of behaviors, with development of stronger evidence, could be translated to population guidelines. Mobile-based applications may then be enriched with interventions that promote or monitor such lifestyle patterns and guide individuals when behaviors diverge from healthy patterns.
Summary
Mobile apps quantifying behaviors and offering interventions to improve dietary, lifestyle, and health behaviors expand the capacities of traditional dietary behavior assessment, translation of the quantified information, time burden and ease of data share, potential accuracy, and platforms for real-time interventions. However, challenges include demonstration of successful intervention efficacy, user enjoyment and engagement, participant adherence, and personalized feedback and support. Many new opportunities for discovery in the diet-health relation are presented with mobile app capacity to quantify multiple types of data at one time, to process and communicate rapidly between the user and server or with other outlets. Mobile apps may collect an expanded range of behavioral and health data that has the potential to be integrated in its relation to the timing of activities over days, weeks, and months. Other environmental, cultural, personal, and even emotional factors may also potentially be integrated and used to discover (63) how the interactive effects of these various components contribute to health outcomes. Mobile apps provide new platforms for prevention and disease management. Individualized guidance and feedback may be provided as apps learn patterns. Finally, the ubiquitous use of mobile devices among the population offers a practical and inexpensive way to reach groups at risk.
Acknowledgments
The authors’ responsibilities were as follows—HAE-M, LP, and CP: were responsible for the design, writing and final content; and all authors: read and approved the final manuscript.
Notes
HAE-M received support for this work by the National Cancer Institute of the NIH under award number R21CA224764.
Author disclosures: HAE-M receives or has received funding from the USDA, the NIH, the US Federal Office of Rural Health, the University of Kentucky Center for Poverty Research, Eli Lilly and Company, and Purdue University. She has served as a consultant to Colletta Consulting, Mead Johnson, the National Dairy Council, the Indiana Dairy Association, and the American Egg Board. She has previously received travel support to present research findings from the Institute of Food Technologists and International Food Information Council. CP received funding from Robert Wood Johnson Foundation, the USDA, the NIH, WHO, and from the RCMI Translational Research Network. However, these organizations had no role in this article. All other authors report no conflicts of interest.
Contributor Information
Heather A Eicher-Miller, Department of Nutrition Science, Purdue University, West Lafayette, IN, USA.
Lukkamol Prapkree, Department of Dietetics and Nutrition, Robert Stempel College of Public Health & Social Work, Florida International University, Miami, FL, USA.
Cristina Palacios, Department of Dietetics and Nutrition, Robert Stempel College of Public Health & Social Work, Florida International University, Miami, FL, USA.
References
- 1. Demographics of mobile device ownership and adoption in the United States | Pew Research Center. [Internet]. [Cited 20 Oct, 2020]. Available from: https://www.pewresearch.org/internet/fact-sheet/mobile/. [Google Scholar]
- 2. 10 facts about smartphones | Pew Research Center. [Internet]. [Cited 28 Oct, 2020]. Available from: https://www.pewresearch.org/fact-tank/2017/06/28/10-facts-about-smartphones/. [Google Scholar]
- 3. Bensley RJ, Hovis A, Horton KD, Loyo JJ, Bensley KM, Phillips D, Desmangles C. Accessibility and preferred use of online web applications among WIC participants. J Nutr Educ Behav. 2014;46(3S):S87–92. [DOI] [PubMed] [Google Scholar]
- 4. Kelley PG, Consolvo S, Cranor LF, Jung J, Sadeh N, Wetherall D. A conundrum of permissions: installing applications on an android smartphone. Financial Cryptography and Data Security. Lecture Notes in Computer Science, vol. 7398. Berlin, Heidelberg, Springer. 2012;68–79. [Google Scholar]
- 5. U.S. app installation & use by device 2016 | Statista[Internet]. [Cited 20 Oct, 2020]. Available from: https://www.statista.com/statistics/681206/us-app-installation-usage-device/. [Google Scholar]
- 6. Krebs P, Duncan DT. Health app use among US mobile phone owners: a national survey. JMIR mHealth uHealth. 2015;3(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Direito A, Pfaeffli Dale L, Shields E, Dobson R, Whittaker R, Maddison R. Do physical activity and dietary smartphone applications incorporate evidence-based behaviour change techniques?. BMC Public Health. 2014;14(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schoeppe S, Alley S, Rebar AL, Hayman M, Bray NA, Van Lippevelde W, Gnam JP, Bachert P, Direito A, Vandelanotte C. Apps to improve diet, physical activity and sedentary behaviour in children and adolescents: a review of quality, features and behaviour change techniques. Int J Behav Nutr Phys Act. 2017;14(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Villinger K, Wahl DR, Boeing H, Schupp HT, Renner B. The effectiveness of app-based mobile interventions on nutrition behaviours and nutrition-related health outcomes: a systematic review and meta-analysis. Obes Rev. 2019;20(10):1465–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. West JH, Belvedere LM, Andreasen R, Frandsen C, Hall PC, Crookston BT. Controlling your “App”etite: how diet and nutrition-related mobile apps lead to behavior change. JMIR mHealth uHealth. 2017;5(7):e95–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Flores Mateo G, Granado-Font E, Ferré-Grau C, Montaña-Carreras X. Mobile phone apps to promote weight loss and increase physical activity: a systematic review and meta-analysis. J Med Internet Res. 2015;17(11):e253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Toro-Ramos T, Lee D-H, Kim Y, Michaelides A, Oh TJ, Kim KM, Jang HC, Lim S. Effectiveness of a smartphone application for the management of metabolic syndrome components focusing on weight loss: a preliminary study. Metabolic Syndrome and Related Disorders. 2017;15(9):465–73. [DOI] [PubMed] [Google Scholar]
- 13. Spring B, Pellegrini CA, Pfammatter A, Duncan JM, Pictor A, McFadden HG, Siddique J, Hedeker D. Effects of an abbreviated obesity intervention supported by mobile technology: the ENGAGED randomized clinical trial. Obesity. 2017;25(7):1191–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Balk-Møller NC, Poulsen SK, Larsen TM. Effect of a nine-month web- and app-based workplace intervention to promote healthy lifestyle and weight loss for employees in the social welfare and health care sector: a randomized controlled trial. J Med Internet Res. 2017;19(4):e108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fukuoka Y, Gay CL, Joiner KL, Vittinghoff E. A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am J Prev Med. 2015;49(2):223–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gilliland J, Sadler R, Clark A, O'Connor C, Milczarek M, Doherty S. Using a smartphone application to promote healthy dietary behaviours and local food consumption. Biomed Res Int. 2015:841368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ipjian M, Johnston C, Shepard C, Johnson M. The popular calorie counter app, MyFitnessPal, used to improve dietary sodium intake: a four-week randomized parallel trial | ASU Digital Repository. [Internet]. 2016[Cited 20 Oct, 2020]. Available from: https://repository.asu.edu/items/34752. [Google Scholar]
- 18. Eyles H, McLean R, Neal B, Jiang Y, Doughty RN, McLean R, Ni Mhurchu C. A salt-reduction smartphone app supports lower-salt food purchases for people with cardiovascular disease: findings from the SaltSwitch randomised controlled trial. Eur J Prev Cardiolog. 2017;24(13):1435–44. [DOI] [PubMed] [Google Scholar]
- 19. Eyles H, McLean R, Neal B, Doughty RN, Jiang Y, Ni Mhurchu C. Using mobile technology to support lower-salt food choices for people with cardiovascular disease: protocol for the SaltSwitch randomized controlled trial. BMC Public Health. 2014;14:950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Carter MC, Burley VJ, Nykjaer C, Cade JE. Adherence to a smartphone application for weight loss compared to website and paper diary: pilot randomized controlled trial. J Med Internet Res. 2013;15(4):e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abreu OJ, Tatakis DN, Elias-Boneta AR, López Del Valle L, Hernandez R, Pousa MS, Palacios C. Low vitamin D status strongly associated with periodontitis in Puerto Rican adults. BMC Oral Health. 2016;16(1):89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Palacios C, Torres M, López D, Trak-Fellermeier MA, Coccia C, Pérez CM. Effectiveness of the nutritional app “MyNutriCart” on food choices related to purchase and dietary behavior: a pilot randomized controlled trial. Nutrients. 2018;10(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Prapkree L, Sadjadi M, Huffman F, Palacios C. Development and pilot testing of the Snackability smartphone application to identify healthy and unhealthy snacks. Healthc Inform Res. 2019;25(3):161–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. López D, Torres M, Vélez J, Grullon J, Negrón E, Pérez CM, Palacios C. Development and evaluation of a nutritional smartphone application for making smart and healthy choices in grocery shopping. Healthc Inform Res. 2017;23(1):16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mummah S, Robinson TN, Mathur M, Farzinkhou S, Sutton S, Gardner CD. Effect of a mobile app intervention on vegetable consumption in overweight adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2017;14(1):125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hales S, Turner-McGrievy GM, Wilcox S, Fahim A, Davis RE, Huhns M, Valafar H. Social networks for improving healthy weight loss behaviors for overweight and obese adults: a randomized clinical trial of the social pounds off digitally (Social POD) mobile app. Int J Med Inf. 2016;94:81–90. [DOI] [PubMed] [Google Scholar]
- 27. Laing BY, Mangione CM, Tseng C-H, Leng M, Vaisberg E, Mahida M, Bholat M, Glazier E, Morisky DE, Bell DS. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients: a randomized, controlled trial. Ann Intern Med. 2014;161(10):S5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Partridge SR, McGeechan K, Hebden L, Balestracci K, Wong AT, Denney-Wilson E, Harris MF, Phongsavan P, Bauman A, Allman-Farinelli M. Effectiveness of a mHealth lifestyle program with telephone support (TXT2BFiT) to prevent unhealthy weight gain in young adults: randomized controlled trial. JMIR mHealth uHealth. 2015;3(2):e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Naimark SJ, Madar Z, Shahar DR. The impact of a web-based app (eBalance) in promoting healthy lifestyles: randomized controlled trial. J Med Internet Res. 2015;17(3):e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kerr DA, Harray AJ, Pollard CM, Dhaliwal SS, Delp EJ, Howat PA, Pickering MR, Ahmad Z, Meng X, Pratt ISet al. . The connecting health and technology study: a 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int J Behav Nutr Phys Act. 2016;13:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013;20(3):513–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Duncan M, Vandelanotte C, Kolt GS, Rosenkranz RR, Caperchione CM, George ES, Ding H, Hooker C, Karunanithi M, Maeder AJet al. . Effectiveness of a web- and mobile phone-based intervention to promote physical activity and healthy eating in middle-aged males: randomized controlled trial of the Manup study. J Med Internet Res. 2014;16(6):e136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Martin CK, Miller AC, Thomas DM, Champagne CM, Han H, Church T. Efficacy of SmartLoss, a smartphone-based weight loss intervention: results from a randomized controlled trial. Obesity. 2015;23(5):935–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Van Lippevelde W, Vangeel J, De Cock N, Lachat C, Goossens L, Beullens K, Vervoort L, Braet C, Maes L, Eggermont Set al. . Using a gamified monitoring app to change adolescents’ snack intake: the development of the REWARD app and evaluation design. BMC Public Health. 2016;16:725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shieh YY, Tsai FY, Anavim A, Shieh M, Wang MD, Lin C-MC. Mobile healthcare: the opportunities and challenges. IJEH. 2008;4(2):208–19. [DOI] [PubMed] [Google Scholar]
- 36. Boushey CJ, Spoden M, Zhu FM, Delp EJ, Kerr DA. New mobile methods for dietary assessment: review of image-assisted and image-based dietary assessment methods. Proc Nutr Soc. 2017;76(3):283–94. [DOI] [PubMed] [Google Scholar]
- 37. Phillips SA, Ali M, Modrich C, Oke S, Elokda A, Laddu D, Bond S. Advances in health technology use and implementation in the era of healthy living: implications for precision medicine. Prog Cardiovasc Dis. 2019;62(1):44–9. [DOI] [PubMed] [Google Scholar]
- 38. Six BL, Schap TE, Zhu FM, Mariappan A, Bosch M, Delp EJ, Ebert DS, Kerr DA, Boushey CJ. Evidence-based development of a mobile telephone food record. J Am Diet Assoc. 2010;110(1):74–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kim S, Schap T, Bosch M, Maciejewski R, Delp EJ, Ebert DS, Boushey CJ. Development of a mobile user interface for image-based dietary assessment. Proceeding of Int Conf Mob Ubiquitous Multimedia. 2010; Dec;13. [DOI] [PMC free article] [PubMed]
- 40. Ho DKN, Tseng S-H, Wu M-C, Shih C-K, Atika AP, Chen Y-C, Chang J-S. Validity of image-based dietary assessment methods: a systematic review and meta-analysis. Clin Nutr. 2020;39(10):2945–59. [DOI] [PubMed] [Google Scholar]
- 41. Nour M, Chen J, Allman-Farinelli M. Young adults’ engagement with a self-monitoring app for vegetable intake and the impact of social media and gamification: feasibility study. JMIR Form Res. 2019;3(2):e13324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hoeppner BB, Hoeppner SS, Seaboyer L, Schick MR, Wu GWY, Bergman BG, Kelly JF. How smart are smartphone apps for smoking cessation? A content analysis. NICTOB. 2016;18(5):1025–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Singh K, Drouin K, Newmark LP, Lee JH, Faxvaag A, Rozenblum R, Pabo EA, Landman A, Klinger E, Bates DW. Many mobile health apps target high-need, high-cost populations, but gaps remain. Health Aff. 2016;35(12):2310–8. [DOI] [PubMed] [Google Scholar]
- 44. Edney S, Ryan JC, Olds T, Monroe C, Fraysse F, Vandelanotte C, Plotnikoff R, Curtis R, Maher C. User engagement and attrition in an app-based physical activity intervention: secondary analysis of a randomized controlled trial. J Med Internet Res. 2019;21(11):e14645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Serrano KJ, Coa KI, Yu M, Wolff-Hughes DL, Atienza AA. Characterizing user engagement with health app data: a data mining approach. Behav Med Pract Policy Res. 2017;7(2):277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen J. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14(6):e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. De Cock N, Van Lippevelde W, Vangeel J, Notebaert M, Beullens K, Eggermont S, Deforche B, Maes L, Goossens L, Verbeken Set al. . Feasibility and impact study of a reward-based mobile application to improve adolescents’ snacking habits. Public Health Nutr. 2018;21(12):2329–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Samoggia A, Riedel B. Assessment of nutrition-focused mobile apps’ influence on consumers’ healthy food behaviour and nutrition knowledge. Food Res Int. 2020;128:108766. [DOI] [PubMed] [Google Scholar]
- 49. Kollannoor-Samuel G, Chhabra J, Fernandez ML, Vega-López S, Pérez SS, Damio G, Calle MC, D'Agostino D, Perez-Escamilla R. Determinants of fasting plasma glucose and glycosylated hemoglobin among low income Latinos with poorly controlled type 2 diabetes. J Immigrant Minority Health. 2011;13(5):809–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Marinac CR, Sears DD, Natarajan L, Gallo LC, Breen CI, Patterson RE. Frequency and circadian timing of eating may influence biomarkers of inflammation and insulin resistance associated with breast cancer risk. PLoS One. 2015;10(8):e0136240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang JB, Patterson RE, Ang A, Emond JA, Shetty N, Arab L. Timing of energy intake during the day is associated with the risk of obesity in adults. J Hum Nutr Diet. 2014;27(2):255–62. [DOI] [PubMed] [Google Scholar]
- 52. Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity. 2013;21(12):2504–12. [DOI] [PubMed] [Google Scholar]
- 53. St-Onge M-P, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, Varady K. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135(9):e96–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Reutrakul S, Hood MM, Crowley SJ, Morgan MK, Teodori M, Knutson KL. The relationship between breakfast skipping, chronotype, and glycemic control in type 2 diabetes. Chronobiol Int. 2014;31(1):64–71. [DOI] [PubMed] [Google Scholar]
- 55. Chomistek AK, Shiroma EJ, Lee I-M. The relationship between time of day of physical activity and obesity in older women. J Phys Act Health. 2016;13(4):416–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Park S, Jastremski CA, Wallace JP. Time of day for exercise on blood pressure reduction in dipping and nondipping hypertension. J Hum Hypertens. 2005;19(8):597–605. [DOI] [PubMed] [Google Scholar]
- 57. Huang T, Lu C, Schumann M, Le S, Yang Y, Zhuang H, Lu Q, Liu J, Wiklund P, Cheng S. Timing of exercise affects glycemic control in type 2 diabetes patients treated with metformin. J Diabetes Res. 2018;2483273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Francois ME, Baldi JC, Manning PJ, Lucas SJE, Hawley JA, Williams MJA, Cotter JD. Exercise snacks before meals: a novel strategy to improve glycaemic control in individuals with insulin resistance. Diabetologia. 2014;57(7):1437–45. [DOI] [PubMed] [Google Scholar]
- 59. Farah NMF, Gill JMR. Effects of exercise before or after meal ingestion on fat balance and postprandial metabolism in overweight men. Br J Nutr. 2013;109(12):2297–307. [DOI] [PubMed] [Google Scholar]
- 60. Erickson ML, Little JP, Gay JL, McCully KK, Jenkins NT. Effects of postmeal exercise on postprandial glucose excursions in people with type 2 diabetes treated with add-on hypoglycemic agents. Diabetes Res Clin Pract. 2017;126:240–7. [DOI] [PubMed] [Google Scholar]
- 61. Terada T, Wilson BJ, Myette-Côté E, Kuzik N, Bell GJ, McCargar LJ, Boule NG. Targeting specific interstitial glycemic parameters with high-intensity interval exercise and fasted-state exercise in type 2 diabetes. Metabolism. 2016;65(5):599–608. [DOI] [PubMed] [Google Scholar]
- 62. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JAC. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Aqeel M, Forster A, Richards EA, Hennessy E, McGowan B, Bhadra A, Guo J, Gelfand S, Delp E, Eicher-Miller HA. The effect of timing of exercise and eating on postprandial response in adults: a systematic review. Nutrients. 2020;12(1):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Aqeel M, Forster A, Richards EA, Hennessy E, McGowan B, Bhadra A, Guo J, Gelfand S, Delp E, Eicher-Miller HA. Correction: Marah Aqeel et al. “The effect of timing of exercise and eating on postprandial response in adults: a systematic review.” Nutrients. 2020;12:221. Nutrients. 2020;12(5):1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Eicher-Miller HA, Khanna N, Boushey CJ, Gelfand SB, Delp EJ. Temporal dietary patterns derived among the adult participants of the National Health and Nutrition Examination Survey 1999–2004 are associated with diet quality. Journal of the Academy of Nutrition and Dietetics. 2016;116(2):283–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Aqeel MM, Guo J, Lin L, Gelfand SB, Delp EJ, Bhadra A, Richards EA, Hennessy E, Eicher-Miller HA. Temporal dietary patterns are associated with obesity in US adults. J Nutr. 2020;150(12):3259–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Aqeel M, Guo J, Lin L, Gelfand S, Delp E, Bhadra A, Richards EA, Hennessy E, Eicher-Miller HA. Temporal physical activity patterns are associated with obesity in U.S. adults. 28 Aug, 2020, Preprint (version 1). [Cited 24 Oct, 2020] [Internet]. Available from: 10.21203/rs.3.rs-67153/v1. [DOI] [PMC free article] [PubMed]
- 68. Lin L, Aqeel M, Guo J, Gelfand S, Delp E, Bhadra A, Richards EA, Hennessy E, Eicher-Miller HA. Joint temporal dietary and physical activity patterns: associations with health status indicators and chronic diseases. Curr Dev Nutr. 2020;4(2):590. [DOI] [PMC free article] [PubMed] [Google Scholar]






