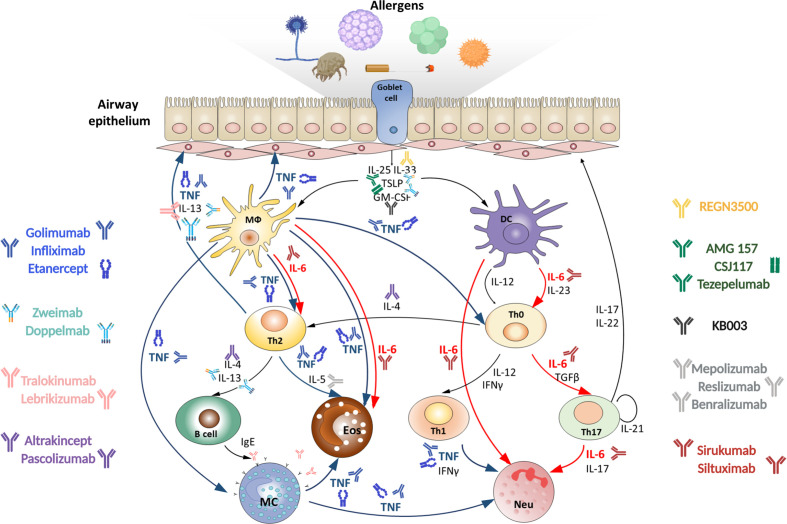
Figure 1.
Targeting TNF, IL-6 and other cytokines in acute severe asthma. Severe asthma pathogenesis: epithelial cells exposed to pro‐inflammatory and allergic stimuli release mediators such as TSLP, IL-33 and IL-25, which activate dendritic cells. Within the airway lumen allergens can be captured by dendritic cells, which process antigenic molecules and present them to naïve (Th0) T helper cells. The consequent activation of allergen-specific Th2 cells is responsible for the production of IL-4 and IL-13 that promote B-cell operated synthesis of IgE antibodies and IL-5, which induces eosinophil maturation and survival. Eosinophils activated by IL-5 contribute to oxidative stress. On the other hand, in the presence of IL-23 and IL-6 upon dendritic cell activation Th0 cells differentiate into Th17 cells or into Th1 cells in the presence of IL-12. Th1 and Th17 cells stimulate and induce neutrophilic inflammation, characteristic of severe asthma. Combined pharmacological inhibition of TNF and IL-6 in acute allergic asthma may more effectively reduce the severity of inflammatory response in the lungs as compared to inhibition of these cytokines individually, since it blocks multiple pathogenic mechanisms. MФ, macrophage; DC, dendritic cell; Th, T helper; MC, mast cell; Eos, eosinophil; Neu, neutrophil.