Abstract
Background:
Health care workers (HCWs) experience increased occupational risk of contracting COVID-19, with temporal trends that might inform surveillance.
Methods:
We analyzed data from a Veterans Affairs hospital-based COVID-19 worker telephone hotline collected over 40 weeks (2020). We calculated the proportion of COVID-19+ cases among persons-under-investigation (PUIs) for illness compared to rates from a nearby large university-based health care institution.
Results:
We observed 740 PUIs, 65 (8.8%) COVID-19+. Time trends were similar at the study and comparison hospitals; only for the first of 10 four-week observation periods was the ratio for observed to expected COVID-19+ significant (P < 0.001).
Discussion:
These data suggest that employee health COVID-19+ to PUI ratios could be utilized as a barometer of community trends. Pooling experience among heath care facilities may yield insights into occupational infectious disease outbreaks.
Keywords: COVID-19, employee health, occupational infectious disease, person under investigation, surveillance
Health care workers (HCWs) comprise an occupational group closely monitored for coronavirus disease 2019 (COVID-19) incidence and can serve as a bellwether for wider community trends. This can be seen, for example, in HCWs juxtaposed with community COVID-19 incidence over time in Toronto, Canada.1 The earlier severe adult respiratory syndrome (SARS) experience in Toronto also showed that hospital-acquired incidence, for which a key contribution came from HCWs, was a harbinger of community trends.2
Compared to the general population, HCWs are presumed to be at greater risk of contracting COVID-19. Increased risk pertains to HCWs who have direct patient care duties, but may also extend to those who do not directly interface with patients. The incidence of disease among HCWs, even if elevated, nonetheless should mirror general population trends, assuming the risk of disease in HCWs relative to others is stable over time. This might not be the case, for example, in scenarios where HCWs over time adopt more effective protection relative to the general public. Conversely, were exposures among HCWs to worsen relative to the general population, temporal trends might also diverge. Furthermore, it is possible that the experiences of different hospitals vary widely, even within the same community, such that one better reflects population trends than another. For these reasons it has not been clear the extent to which public health inferences can be drawn accurately from trends in HCW COVID-19 incidence.
We wished to assess the extent to which population temporal trends of COVID-19 were reflected in HCW incidence and how such incidence differed between two healthcare centers in the same geographic locale. We tracked the frequencies of symptom reporting and testing results for COVID-19 within two separate medical facilities, quantifying the numbers of persons under investigation (PUI) and the positive cases identified within this group over 40 consecutive weeks in 2020. We qualitatively assessed the trend in rates, further testing whether the rates of test positivity differed statistically between the two occupational cohorts: the study healthcare facility and a larger, referent facility.
METHODS
Our primary data source (the study healthcare facility) was comprised of Employee Health Service COVID-19 case reporting at the San Francisco Veterans Affairs HealthCare System (SFVAHCS) which is comprised of the San Francisco VA Medical Center and its associated VA Community Based Outpatient Clinics. The latter are geographically distributed, largely drawing from California coastal counties north of San Francisco.
Since March 2020, the employees of the SFVAHCS have been instructed to call a dedicated Employee Health telephone hotline when experiencing any symptoms potentially related to COVID-19. Employees who contact the hotline and report symptoms are considered to be PUIs and are referred for COVID-19 testing using polymerase chain reaction (PCR) methodologies (either RT-PCR Abbott or rapid RT-PCR Cepheid, depending upon clinical scenario) by nasopharyngeal or oropharyngeal swab at SFVAHCS testing locations. Employees could choose to be tested at multiple other venues, including though their primary care provider or at public testing sites, although this occurred in a small minority of cases, likely because of relatively easy access to SFVAHCS testing. Without compensation (WOC) employees and trainees or students are encouraged to call the hotline as well. We include data for the former, but we have excluded trainees and students from this analysis. The data from all hotline calls are entered in real time into a custom formatted secure Microsoft Access database. Clinical staff later enter pertinent additional data, including follow-up results on pending tests.
This database also contains data on other employees who are being followed for a range of other COVID-19-related issues. For example, it includes data collected form a large surveillance program of asymptomatic HCWs who enter a congregate care facility and from asymptomatic persons with moderate to high risk exposure to a known COVID-19 case. We excluded those, limiting this analysis solely to PUIs due to symptoms potentially associated with COVID-19. Ultimately, we classified all PUIs as being either positive or negative for COVID-19.
As part of a quality improvement project, we extracted from our COVID hotline database the date of testing and the outcome (test positive or negative for COVID) for all PUIs (other than trainees or students, as noted previously) for the 40-week period from March 17 through December 21, 2020. We summarized case incidence by 4-week intervals and calculated the proportion of COVID-19 positive PUIs to all PUIs for each of the 10 periods.
We obtained comparison rates of positive cases to total PUIs for the same period from the institution with which the SFVAHCS is academically affiliated, the University of California, San Francisco (UCSF), which served as our referent healthcare facility. This referent healthcare facility followed a similar protocol of instructing the employees to call the hotline when symptomatic and obtain testing onsite. The employee population at the SFVAHCS, including non-salaried personnel, is approximately 4000, while the UCSF employee cohort is approximately five times as large. The referent data were provided by the UCSF Occupational Health Services, which maintains its own COVID-19 telephone hotline service, completely separate from that of the SFVAHCS. Data for students and trainees were similarly excluded from the referent data UCSF provided for this analysis. We used the UCSF positive COVID-19 to PUI case rates to generate an expected value for case incidence at the SFVAHCS. We tested the ratio of observed to expected cases as the ratio of a Poison variable to its expectation. We performed all analyses using R statistical software.
RESULTS
The frequency of all PUIs and COVID-19 positive PUIs at the study healthcare facility for each study interval is shown in Figure 1. Over the entire observation period there were 740 reported PUIs of whom 65 (8.8%; 95% CI 8.1% to 9.4%) were COVID-19 positive. In the initial 4-week interval (March 17 to April 13), there were 13 COVID-19 cases among 104 PUIs. Over the next 12 weeks, the incidence of PUIs and of COVID-19 positive cases declined sharply, but then recrudesced over the next 4-week period, corresponding to the second week in July (ie, following the Fourth of July holiday) through the beginning of August. The number of PUIs and COVID-19 cases subsequently declined, with a lower plateau through the third week in October. November and December 2020 were marked by another sharp increase back to the peak observed earlier in July.
FIGURE 1.
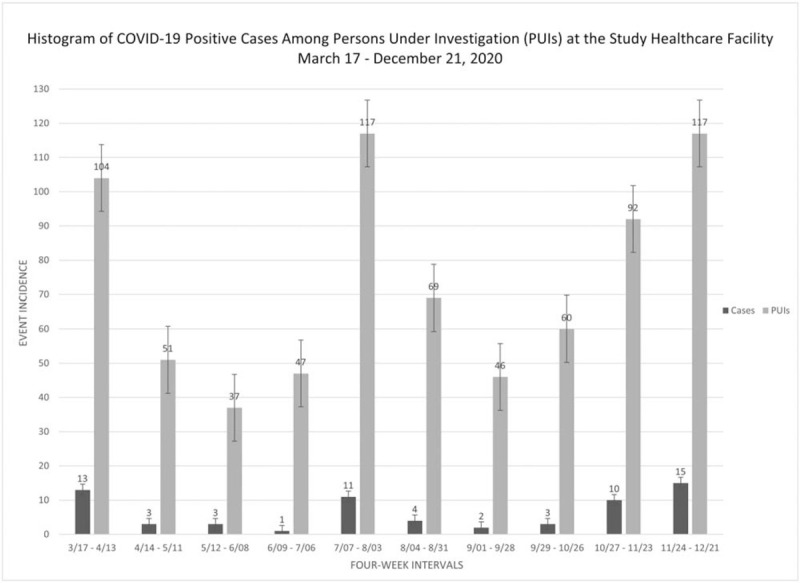
Incidence numbers for PUIs and among those, COVID-19 positive tests among healthcare workers at a single healthcare facility (the study hospital) over a 40-week observation period. PUIs, persons under investigation; COVID-19, Coronavirus Disease 2019.
Figure 2 shows the trend over time in the proportion of positive cases to total PUIs for both the study and referent healthcare facilities. Figure 2 demonstrates parallel temporal trends at the sites, most saliently, a peak in July, then a decline, followed by a second increase in the final 8 weeks of observation late in 2020. Table 1 presents the ratio of observed cases at the study facility to the expected value based on the referent-based expected value. In the first 4-week observation period, the ratio of observed to expected was elevated more than three-fold. This was the only period for which the ratio of observed to expected was statistically significant. Although none of the 10 P-values shown in Table 1 is adjusted for multiple comparisons, the unadjusted value for the first period (P = 0.00044), remains less than 0.05 even when Bonferroni-adjusted (P = 0.004). Overall, three ratios of observed to expected were less than 1.0 and did not cluster in time: periods 4, 6, and 10.
FIGURE 2.
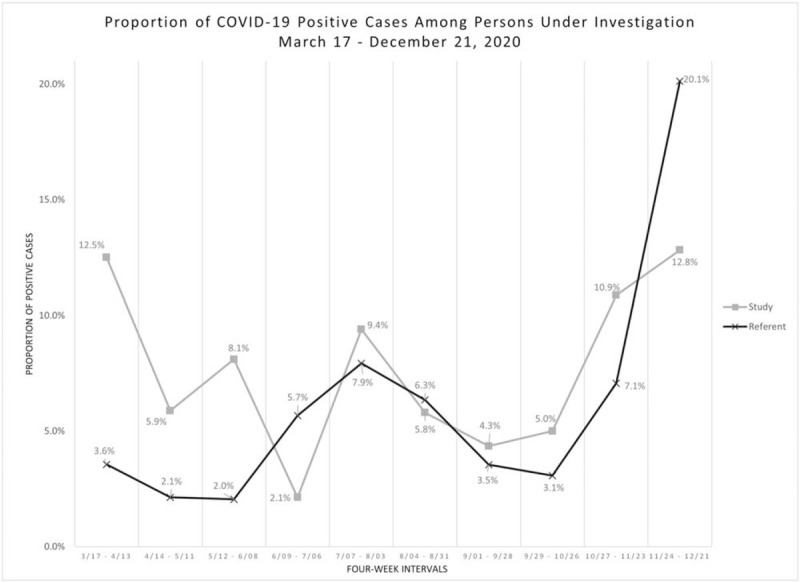
Rates of COVID-19 positivity among PUIs as two different healthcare centers located in the same city over the same 40-week time period. PUIs, persons under investigation; COVID-19, Coronavirus Disease 2019.
TABLE 1.
Ratio of COVID-19 Test Positive Incidence to That Expected Based on the Case Rate of an Affiliated Institution Over 40 Consecutive Weeks in 2020
| Four Week PeriodCalendar Year 2020 | Ratio of Observed to Expected Cases | 95% CI | P |
| 3/17–4/13 | 3.51 | 1.7–6.8 | <0.05 |
| 4/14–5/11 | 2.75 | 0.49–10.4 | 0.13 |
| 5/12–6/08 | 3.96 | 0.66–17.4 | 0.07 |
| 6/09–7/06 | 0.38 | 0.01–2.30 | 0.5 |
| 7/07–8/03 | 1.19 | 0.56–2.29 | 0.6 |
| 8/04–8/31 | 0.91 | 0.24–2.49 | >0.9 |
| 9/01–9/28 | 1.23 | 0.14–4.92 | 0.7 |
| 9/29–10/26 | 1.63 | 0.31–5.39 | 0.4 |
| 10/27–11/23 | 1.54 | 0.71–3.00 | 0.2 |
| 11/24–12/21 | 0.64 | 0.35–1.08 | 0.09 |
DISCUSSION
Our data are consistent with overall temporal COVID-19 trends in San Francisco City and County, which showed a summer rise (peak incidence July 7, 2020), a subsequent decline (nadir October 8, 2020) and then an unrelenting uptick through the following 2 months.3 Moreover, since both healthcare facilities draw their employee populations from a number of surrounding counties with varying COVID-19 rates, the comparison to San Francisco alone is imprecise, even if informative.
COVID-19 incidence among healthcare facility employees has been reported in multiple studies. For example, a study of COVID-19 incidence among 10,000 staff at a UK hospital was able to draw inferences about the relative risks of different job groups within the hospital.4 That study, which included test positive cases among symptomatic and asymptomatic HCWs over a 3-month period, showed that incidence paralleled COVID-19 patient admissions to the same hospital. A study of a 6000 member workforce at an Italian hospital, similarly based on screening of symptomatic and asymptomatic employees, also identified job-associated risks, but did not compare HCW rates to others.5 A population-based study carried out in Wuhan, China established that HCWs were at increased risk of contracting COVID-19 and that the risk within HCWs differed by job duties.6 It has been estimated that HCWs experience more than three-fold increased odds of COVID-19 infection.7 These studies do not directly assess whether or not hospital-specific passive surveillance based on symptomatic case reporting among HCWs reasonably reflects community-wide trends and thus can inform management, for example, for surge planning. A national US study of COVID-19 rates over time among nursing home HCWs observed that these incidence data paralleled community trends.8 The Toronto-based analysis cited previously also showed the HCW rates paralleled and even preceded wider population trends.1
Our findings suggest that data could be pooled among multiple heath care facilities in order to gain better insights into differences in testing and positivity rates among various employee groups within the HCW sector. Such pooled data have the potential to serve as a barometer of community trends or even be a bellwether of evolving surges in infection, although fully assessing the predictive utility of employee health surveillance would require additional study. We did note that early in the pandemic, the employee positivity rates among PUIs did differ significantly between facilities. This may reflect rapidly changing factors driving self-report of symptoms or differential characterization of potential symptoms by healthcare providers. That the observed difference between the two sites did not persist over time is consistent with the supposition that identification of PUIs became a more standardized process across facilities.
The limitations of our data should be borne in mind. We did not analyze COVID positivity among asymptomatic persons, which might be more relevant to comparisons of broader population screening. Although we observed trends consistent with data local to San Francisco, the labor forces of both the study and referent healthcare facilities draw employees from farther afield, as previously noted. Furthermore, the two healthcare facilities that contributed data to this analysis are likely to vary considerably from each other in employee demographics. This latter limitation could explain observed differences in positive rates for PUIs, even though we could not reject these differences being due to chance. Although the employee health units made efforts to harmonize protocols between the two facilities, for example, in PUI-defining symptoms, differences in practices between them nonetheless likely contributed to variability and potential selection biases. Other limitations arise from potentially unreported symptoms among employees, reluctance to seek testing, or failure to report positive test results. We do not have reason to believe that such factors led to differential outcome misclassification.
In summary, the incidence of COVID-19 cases among symptomatic PUIs observed at two separate healthcare facilities varied over time consistent with wider population trends. This underscores the potential value in HCW COVID-19 surveillance in prevention efforts within and across facilities in geographic proximity as well as the potential for wider public health insights such data can provide.
Footnotes
Health Research Services Administration (HRSA) training award D33HP31668 (Dr McNicholas).
Ethical considerations and disclosures: This report is based on quality improvement efforts.
The authors report no conflicts of interest.
Clinical significance: Employee health services for health workers have been on the frontlines of COVID-19 detection and occupational case reporting. The experience of employee health units could be utilized as a barometer of community trends and can yield insights into COVID-19 and other occupational infectious disease outbreaks.
REFERENCES
- 1.Schwartz KL, Achonu C, Buchan SA, et al. Epidemiology, clinical characteristics, household transmission, and lethality of severe acute respiratory syndrome coronavirus-2 infection among healthcare workers in Ontario, Canada. PLoS One 2020; 15:e0244477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fowler RA, Lapinsky SE, Hallett D, et al. Critically ill patients with severe acute respiratory syndrome. JAMA 2003; 290:367–373. [DOI] [PubMed] [Google Scholar]
- 3. Data SF COVID-19 cases and deaths. Available at: https://data.sfgov.org/stories/s/dak2-gvuj Accessed January 18, 2021. [Google Scholar]
- 4.Eyre DW, Lumley SF, O’Donnell D, et al. Differential occupational risks to healthcare workers from SARS-CoV-2 observed during a prospective observational study. Elife 2020; 9:e60675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Porru S, Carta A, Monaco MGL, et al. Health surveillance and response to SARS-CoV-2 Mass testing in health workers of a large Italian hospital in Verona, Veneto. Int J Environ Res Public Health 2020; 17: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wei J-T, Liu Z-D, Fan Z-W, Zhao L, Cao W-C. Epidemiology of and risk factors for COVID-19 infection among health care workers: a multi-centre comparative study. Int J Environ Res Public Health 2020; 17:7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 2020; 5:e475–e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bagchi S, Mak J, Li Q, et al. Rates of COVID-19 among residents and staff members in nursing homes—United States, May 25–November 22, 2020. MMWR Morb Mortal Wkly Rep 2021; 70:52–55. [DOI] [PMC free article] [PubMed] [Google Scholar]


