Abstract
目的
探讨股骨转子间骨折髓内钉内固定术后内植物周围再骨折的发生情况、治疗方法及临床疗效。
方法
回顾分析 2014 年 4 月—2019 年 11 月收治且符合选择标准的 16 例股骨转子间骨折髓内钉内固定术后内植物周围再骨折患者临床资料。男 7 例,女 9 例;年龄 65~93 岁,平均 78.4 岁。初次单纯股骨转子间骨折 14 例,按国际内固定研究协会/美国骨创伤协会(AO/OTA)分型为 A1 型 5 例,A2 型 7 例,A3 型 2 例;股骨转子间合并转子下骨折 2 例,均为 Seinsheimer Ⅴ型。根据 Chan 等提出的非假体内植物周围再骨折分型标准,1 型 10 例(1A 型 6 例、1B 型 3 例、1C 型 1 例),2 型 6 例(2A 型 4 例、2B 型 2 例)。再骨折距初次手术时间为 1~52 个月,平均 14.6 个月。其中短钉组(髓内钉长度≤240 mm)再骨折发生率为 1.92%(11/573),长钉组(髓内钉长度≥340 mm)为 1.66%(5/301),比较差异无统计学意义(χ2=0.073,P=0.786)。分别予以加长髓内钉翻修(5 例)或增加微创内固定系统固定(11 例)。
结果
患者手术时间 78~168 min,平均 115.8 min;术中出血量 120~500 mL,平均 283.1 mL。1 例患者术后 3 个月发生心肌梗死而死亡;余 15 例均获随访,随访时间 9~46 个月,平均 16.8 个月。内植物周围再骨折于术后 14~20 周,平均 16.4 周达临床愈合。随访期间无切口感染、骨折不愈合、内植物松动断裂、螺钉切出等并发症发生,内植物周围未发生再次骨折。末次随访时,患肢均恢复行走功能,美国特种外科医院(HSS)评分为 56~92 分,平均 80.2 分,其中优 2 例、良 10 例、可 2 例、差 1 例,优良率 80%。
结论
髓内钉尖端及远端交锁螺钉周围应力集中是股骨转子间骨折髓内钉内固定术后内植物周围再骨折的主要原因,根据初次手术髓内钉长度及再骨折类型采用加长髓内钉翻修或增加微创内固定系统手术治疗,有望取得满意疗效。
Keywords: 股骨转子间骨折, 髓内钉, 再骨折, 应力集中
Abstract
Objective
To investigate the occurrence, treatment, and effectiveness of peri-implant refracture after intramedullary nail fixation for intertrochanteric fractures.
Methods
The clinical data of 16 patients with peri-implant refracture after intramedullary nail fixation for intertrochanteric fractures who met the inclusion criteria between April 2014 and November 2019 were retrospectively analyzed. There were 7 males and 9 females with an average age of 78.4 years (range, 65-93 years). The 14 cases of initial intertrochanteric fractures were classified according to the classification of AO/Orthopaedic Trauma Association (AO/OTA): 5 cases of type A1, 7 cases of type A2, and 2 cases of type A3; the other 2 cases were intertrochanteric combined with subtrochanteric fractures (Seinsheimer type Ⅴ). According to the classification of peri-implant refracture which was proposed by Chan et al., there were 10 cases of type 1 (6 cases of type 1A, 3 cases of type 1B, 1 case of type 1C) and 6 cases of type 2 (4 cases of type 2A and 2 cases of type 2B). The average interval between refracture and initial surgery was 14.6 months (range, 1-52 months). The incidence of peri-implant refracture in short nail group (the length of intramedullary nail used in initial surgery≤240 mm) was 1.92% (11/573), while the incidence of long nail group (the length of intramedullary nail used in initial surgery≥340 mm) was 1.66% (5/301), showing no significant difference between the two groups (χ2=0.073, P=0.786). The peri-implant refractures were revised with extended intramedullary nail (5 cases) or fixed with additional limited invasive stabilization system (11 cases).
Results
The average operation time was 115.8 minutes (range, 78-168 minutes) and the average intraoperative blood loss was 283.1 mL (range, 120-500 mL). One patient died of myocardial infarction at 3 months after operation, and the other 15 patients were followed up 9-46 months (mean, 16.8 months). The peri-implant refractures healed at 14-20 weeks (mean, 16.4 weeks) after operation. There was no complications such as incision infection, nonunion, internal fixator loosening and rupture, screw cutting-out, and the second refracture during the follow-up. At last follow-up, all injured limbs regained walking function, and the Hospital for Special Surgery (HSS) score was 56-92 (mean, 80.2). The results were classified as excellent in 2 cases, good in 10, fair in 2, and poor in 1, with the excellent and good rate of 80%.
Conclusion
Stress concentration at the tip of initial intramedullary nail and distal interlocking screw aera is the main cause of peri-implant refracture after intramedullary nail fixation for intertrochanteric fractures. Revision with extended intramedullary nail or fixation with limited invasive stabilization system according to the length of initial intramedullary nail and the type of refracture can get satisfactory effectiveness.
Keywords: Intertrochanteric fracture, intramedullary nail, refracture, stress concentration
随着人口老龄化加剧,股骨转子间骨折发病率逐年上升,伤后 5 年内死亡率最高可达 30%[1]。内固定手术治疗可允许患者术后早期活动、减少卧床并发症及恢复关节功能,是治疗股骨转子间骨折的主要方法[2-3]。根据设计理念不同,内固定方式可分为髓内及髓外两大固定系统。髓内钉具有生物力学优势[4-5],可微创操作减少出血,尤其适用于外侧壁薄弱或不完整、小转子移位骨折、后内侧皮质粉碎、骨折线延伸至转子下以及逆转子骨折等不稳定股骨转子间骨折[6-8],越来越受到骨科医师青睐。但是,髓内钉治疗股骨转子间骨折术后内植物周围再骨折发生率高于动力髋螺钉[9],且再骨折多发生于高龄患者,常合并严重骨质疏松及多种内科疾病,骨折复杂多样,治疗困难。生物力学测试结果显示髓内钉固定股骨转子间骨折后,在轴向及扭转应力作用下,与长钉相比,短钉内植物周围再骨折风险并未增加[10],这与临床报道术后短钉内植物周围再骨折发生率高于长钉[11-15]有所不同。本研究回顾性分析 2014 年 4 月—2019 年 11 月成都市双流区第一人民医院/四川大学华西空港医院收治的股骨转子间骨折髓内钉固定术后内植物周围再骨折患者临床资料,结合初次髓内钉类型,探讨再骨折发生情况、治疗方法及临床疗效。报告如下。
1. 临床资料
1.1. 患者选择标准
纳入标准:① 既往行股骨转子间骨折髓内钉内固定手术;② 本次内植物周围再骨折为外伤导致的新鲜骨折。排除标准:① 病理性骨折;② 内植物取出后发生的再骨折;③ 因合并严重内科疾病不能耐受麻醉或选择保守治疗者。2014 年 4 月—2019 年 11 月成都市双流区第一人民医院/四川大学华西空港医院使用髓内钉治疗股骨转子间骨折 874 例[其中短钉组(髓内钉长度≤240 mm)573 例,长钉组(髓内钉长度≥340 mm)301 例],共 16 例(1.83%,16/874)患者符合上述选择标准纳入研究。
1.2. 一般资料
本组男 7 例,女 9 例;年龄 65~93 岁,平均 78.4 岁。左侧 9 例,右侧 7 例。再骨折原因:行走时摔伤 13 例,交通事故伤 2 例,站立时扭伤 1 例。初次单纯股骨转子间骨折 14 例,按国际内固定研究协会/美国骨创伤协会(AO/OTA)分型为 A1 型 5 例,A2 型 7 例,A3 型 2 例;股骨转子间合并转子下骨折 2 例,均为 Seinsheimer Ⅴ型。根据 Chan 等[16]提出的非假体内植物周围再骨折分型标准,1 型 10 例(1A 型 6 例、1B 型 3 例、1C 型 1 例),2 型 6 例(2A 型 4 例、2B 型 2 例)。再骨折距初次手术时间为 1~52 个月,平均 14.6 个月。其中短钉组发生再骨折 11 例(1.92%,11/573),长钉组发生再骨折 5 例(1.66%,5/301),两组再骨折发生率比较差异无统计学意义(χ2=0.073,P=0.786)。
1.3. 手术方法
1 型骨折中,5 例初次骨折使用短钉固定,取出原髓内钉,更换为股骨加长髓内钉固定;5 例初次骨折使用长钉固定,增加微创内固定系统(limited invasive stabilization system,LISS)桥接固定骨折端。2 型骨折中,6 例初次骨折均使用短钉固定,不取出原髓内钉,增加 LISS 桥接固定,尽可能采用微创技术操作,不显露骨折端间接复位,经皮插入钢板固定。使用 LISS 固定的 11 例患者中,6 例近端锁定螺钉需单皮质固定,必要时辅助钢丝环扎增强稳定性。
1.4. 术后处理及随访指标
术后常规使用抗生素 24 h 预防切口感染,规范性抗骨质疏松治疗,预防深静脉血栓形成及坠积性肺炎。术后即刻开始行踝及足趾主动锻炼、股四头肌等长收缩锻炼。采用股骨加长髓内钉翻修者术后第 2 天、LISS 固定者术后 6 周开始不负重下床活动,通常术后 3 个月 X 线片示骨折线模糊骨痂形成后再完全负重行走。
记录手术时间及术中出血量。术后 1、2、3、4、5、6、9、12 个月及之后每年随访 1 次,摄患侧 X 线片评价内植物位置及骨折愈合情况;采用美国特种外科医院(HSS)评分[17]评价术后膝关节功能;同时记录并发症发生情况。
1.5. 统计学方法
采用 SPSS24.0 统计软件进行分析。计数资料以率表示,组间比较采用 χ2 检验;检验水准 α=0.05。
2. 结果
本组患者手术时间 78~168 min,平均 115.8 min;术中出血量 120~500 mL,平均 283.1 mL。1 例患者术后 3 个月发生心肌梗死而死亡;余 15 例均获随访,随访时间 9~46 个月,平均 16.8 个月。内植物周围再骨折于术后 14~20 周,平均 16.4 周达临床愈合。随访期间无切口感染、骨折不愈合、内固定物松动断裂、螺钉切出等并发症发生,内植物周围未发生再次骨折。末次随访时,患肢均恢复行走功能,膝关节 HSS 评分为 56~92 分,平均 80.2 分,其中优 2 例、良 10 例、可 2 例、差 1 例,优良率 80%。见图 1、2。评价为差者为使用 LISS 桥接固定再骨折处,术后 20 周达骨性愈合,无静息痛,但行走时感膝关节处疼痛,功能较差,HSS 评分为 56 分。
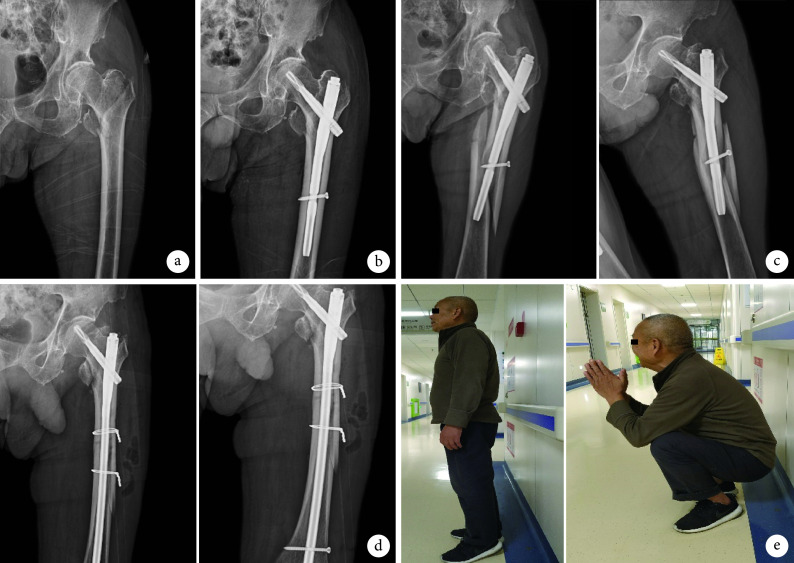
图 1.
A 67-year-old male patient with initial intertrochanteric fracture combined with subtrochanteric comminuted fracture (Seinsheimer type Ⅴ) at 2 years after fixation with long intramedullary nail, who suffered from a right peri-implant femoral refracture (type 1A) due to a fall while walking. The original intramedullary nail was retained and the peri-implant refracture was fixed with limited invasive stabilization system (LISS)
患者,男,67 岁,右侧股骨转子间骨折合并转子下粉碎性骨折(Seinsheimer Ⅴ型)行长髓内钉固定术后 2 年,因行走时摔伤致内植物周围再骨折(1A 型),保留原髓内钉,内植物周围再骨折处使用 LISS 桥接固定
a. 初次骨折术前正侧位 X 线片;b. 初次骨折髓内钉内固定术后即刻正侧位 X 线片;c. 初次术后 2 年正侧位 X 线片示内植物周围再骨折;d. 发生再骨折时原骨折处正侧位 X 线片;e. LISS 桥接固定术后即刻正侧位 X 线片;f. LISS 桥接固定术后 3 年正侧位 X 线片示骨折已愈合;g. LISS 桥接固定术后 3 年关节功能
a. Anteroposterior and lateral X-ray films of the initial fracture; b. Anteroposterior and lateral X-ray films at immediate after the internal fixation of intramedullary nail for initial fracture; c. Anteroposterior and lateral X-ray films at 2 years after the initial intramedullary nail fixation, showed the peri-implant femoral refracture; d. Anteroposterior and lateral X-ray films at the original aera when the refracture occurred; e. Anteroposterior and lateral X-ray films at immediate after operation, showed the refracture area that was fixed with LISS; f. Anteroposterior and lateral X-ray films at 3 years after LISS fixation, showed the refracture had healed; g. The joint function at 3 years after LISS fixation
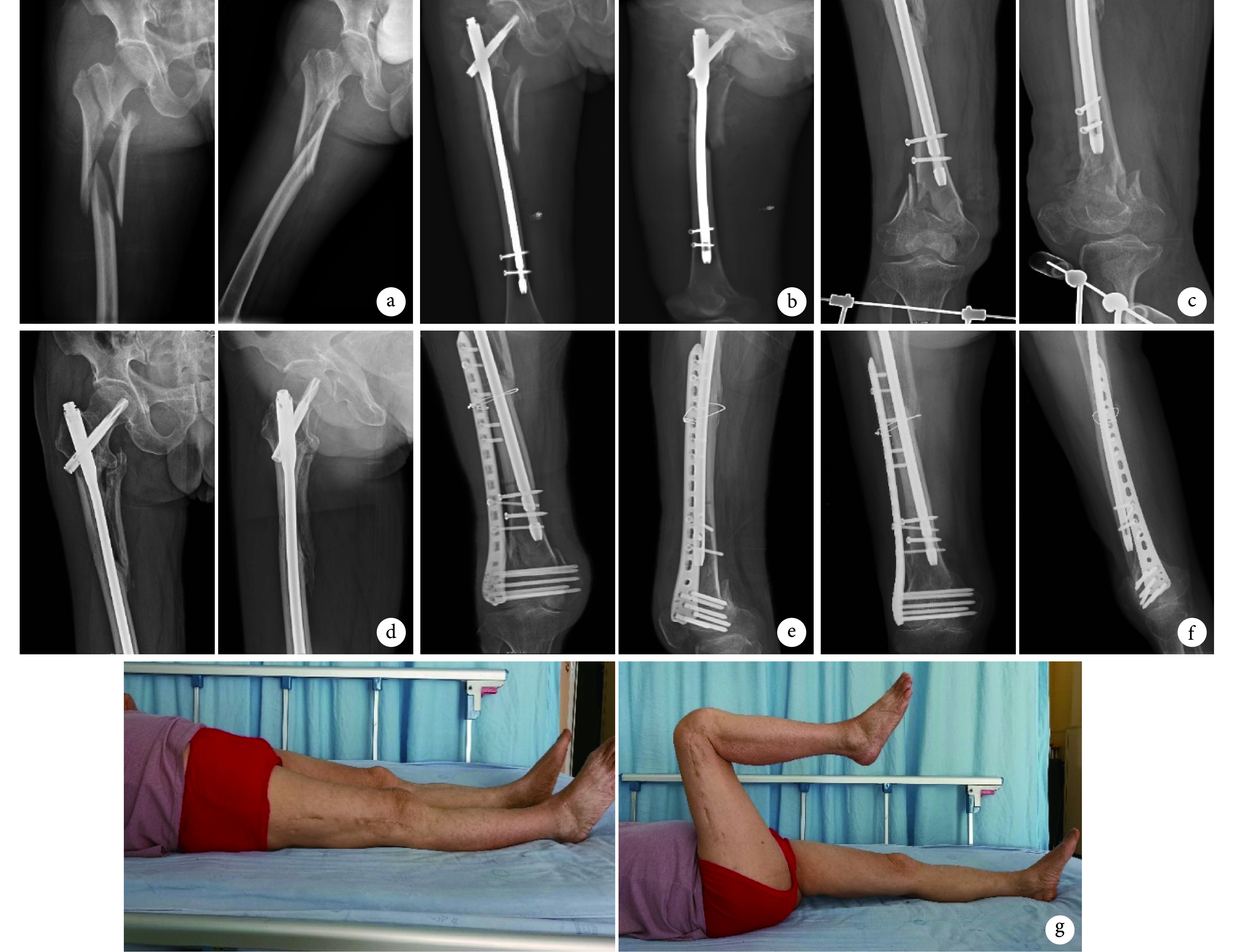
图 2.
A 74-year-old male patient with initial left intertrochanteric fracture (type A2) at 2 months after fixation with short intramedullary nail, who suffered from a left peri-implant refracture (type 1B) due to a fall while walking. The refracture aera was revised with an extended intramedullary nail
患者,男,74 岁,左侧股骨转子间骨折(A2 型)行短髓内钉固定术后 2 个月,因行走时摔伤致内植物周围再骨折(1B 型),更换股骨加长髓内钉固定
a. 初次骨折术前正位 X 线片;b. 初次骨折髓内钉内固定术后即刻正位 X 线片;c. 初次骨折术后 2 个月正斜位 X 线片示内植物周围再骨折;d. 更换股骨加长髓内钉固定术后即刻正位 X 线片示原骨折及再骨折处复位及内固定物位置满意;e. 更换股骨加长髓内钉固定术后 1 年关节功能
a. Anteroposterior X-ray film of the initial intertrochanteric fracture; b. Anteroposterior X-ray film at immediate after the internal intramedullary nail fixation for treating the initial intertrochanteric fracture; c. Anteroposterior and oblique X-ray films at 2 months after the initial operation, showed the peri-implant femoral refracture; d. Anteroposterior X-ray films at immediate after revision operation with extended intramedullary nail, showed the reduction of the initial fracture and the refracture were satisfactory and the internal fixation position was good; e. The joint function at 1 year after revision with extended intramedullary nail
3. 讨论
髓内钉内固定已广泛应用于股骨转子间骨折的治疗,术后内植物周围再骨折也不再罕见。Norris 等[11]报道一组股骨转子间骨折髓内钉内固定术后内植物周围再骨折发生率为 1.7%,分析可能与髓内钉的材质及设计有关,第 3 代 Gamma 钉再骨折发生率显著低于前两代 Gamma 钉,长钉再骨折发生率低于短钉,但两者并无统计学差异。尸体标本生物力学测试显示股骨转子间骨折髓内钉内固定术后,引起短钉组固定失效的载荷高于长钉组,提示短钉固定术后再骨折可能性并不高于长钉[10]。本研究统计显示股骨转子间骨折髓内钉内固定术后内植物周围再骨折发生率为 1.83%(16/874),长钉组发生率低于短钉组,但两组间差异亦无统计学意义,与其他文献结果相同[11-15]。髓内钉尖端及远端交锁螺钉周围应力集中是导致内植物周围再骨折的主要原因[10-11, 18-22]。长钉可有效降低骨干部再骨折风险,其再骨折多发生于干骺端,可能与远端交锁螺钉植入导致局部应力集中有关[10];由于老年人股骨前弓较大,使用短钉尤其是 240 mm 长度髓内钉时,主钉尖端常紧贴股骨前侧皮质,导致局部应力集中而易于发生骨干部位骨折。此外,骨质疏松、跌倒等低能量暴力、骨代谢异常等亦是再骨折发生相关因素,因此术后预防跌倒、规范治疗骨质疏松,对防止内植物周围再骨折非常重要。
由于内植物周围再骨折特点的多样性,要准确分类比较困难。与股骨髓内钉周围再骨折分类近似的是股骨假体周围骨折的 Vancouver 分型[23],其将骨折部位、假体稳定性与骨质条件相结合,便于规范选择治疗方法及评价结果,在国际上得到了广泛认可。目前关于非假体股骨内植物周围再骨折的分类报道较少,Chan 等[16]通过对多中心 60 例患者资料进行研究,根据骨折相对于内植物的解剖位置关系,将非假体内植物周围再骨折分为 1 型(内植物尖部附近)和 2 型(远离内植物);根据原骨折愈合情况又分为 3 个亚型(A 型,骨折已愈合;B 型,骨折未愈合;C 型,原内固定失效)。
为了早期活动避免卧床并发症和远期骨折愈合恢复肢体功能,股骨转子间骨折术后内植物周围再骨折多需手术治疗,骨量降低及骨脆性增加是手术两大难点[24],高龄患者合并多种内科疾病,对围术期管理也提出了更高要求。手术方式可选择股骨加长髓内钉翻修或增加 LISS 桥接固定再骨折端。Ruchholtz 等[25]报道使用解剖锁定钢板治疗 11 例股骨髓内钉周围再骨折均达骨性愈合,微创使用长锁定钢板固定再骨折可减少软组织并发症和内固定失败。Müller 等[9]对 18 例股骨近端骨折术后内植物周围再骨折使用长锁定钢板固定、4 例使用加长股骨近端髓内钉翻修治疗,结果显示长锁定钢板是治疗股骨内植物周围再骨折的有效且可靠方法。陈挺等[26]报道使用 LISS 治疗股骨近端骨折术后髓内钉远端再骨折 12 例,术后 3 个月骨折均获愈合,术后 6 个月膝关节 HSS 评分平均为 84 分。
根据 Chan 等分型标准,1 型骨折通常是由于应力集中引起,若初次手术使用短钉,可更换为股骨加长髓内钉固定原骨折部位与新骨折区域;若初次手术使用长钉,则可增加 LISS 桥接固定再骨折端。2 型骨折若原有髓内钉未失效则可保留,增加 LISS 桥接固定再骨折端;应考虑骨缺损及局部骨质量的降低,但新鲜内植物周围再骨折多无需一期植骨[9]。Kim 等[27]报道 1 例股骨转子间骨折髓内钉内固定术后再骨折,使用锁定钢板固定再骨折端,因钢板长度不够而发生局部应力集中致再次断裂,提示我们注意钢板需重叠原内植物,并且选择足够长度以避免造成明显应力集中。锁定钢板在髓内钉占据髓腔时双皮质固定比较困难,可选择单皮质螺钉附加钢丝固定,开放手术钢丝环扎可能导致周围骨膜血管绞榨、破坏血运、引起骨坏死及骨不连[28],可小切口经皮植入钢丝以减少对局部骨膜血运的破坏[29]。本组 16 例内植物周围再骨折,5 例采用股骨加长髓内钉翻修,11 例增加 LISS 桥接固定,6 例辅助微创钢丝环扎,术后获随访的 15 例患者再骨折均获骨性愈合。
综上述,髓内钉尖端及远端交锁螺钉周围应力集中是股骨转子间骨折术后内植物周围再骨折的主要原因,治疗方式首选内固定手术,根据初次手术髓内钉长度及再骨折类型采用加长髓内钉翻修或增加 LISS 固定再骨折端,有望取得满意疗效。但本研究为回顾性研究,证据级别相对较低;由于存在失访病例,对疗效评价存在一定偏倚,且随访时间尚短,随着股骨转子间骨折髓内钉内固定术后时间延长,内植物周围再骨折发生率会升高,甚至可能出现第 2 次术后再骨折。因此,还需要多中心、大样本的长期随访研究,证实股骨转子间骨折髓内钉内固定术后内植物周围再骨折治疗的临床疗效。
作者贡献:滕林、钟刚负责手术实施、收集资料、撰写论文;肖永川负责统计分析;钟刚对文章的知识性内容作批评性审阅。
利益冲突:所有作者声明,在课题研究和文章撰写过程中不存在利益冲突。
机构伦理问题:研究方案经成都市双流区第一人民医院医学伦理委员会批准。患者均签署医学伦理知情同意书。
References
- 1.Lee SH, Chen IJ, Li YH, et al Incidence of second hip fractures and associated mortality in Taiwan: A nationwide population-based study of 95, 484 patients during 2006-2010. Acta Orthop Traumatol Turc. 2016;50(4):437–442. doi: 10.1016/j.aott.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.杨明辉, 朱仕文, 李庭, 等 老年股骨转子间骨折诊疗指南. 中华创伤骨科杂志. 2020;22(2):93–99. doi: 10.3760/cma.j.issn.1671-7600.2020.02.001. [DOI] [Google Scholar]
- 3.Arslan A, Utkan A, Koca TT Results of a compression pin alongwith trochanteric external fixation in management of high risk elderly intertrochanteric fractures. Indian J Orthop. 2016;50(6):636–640. doi: 10.4103/0019-5413.193479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anglen JO, Weinstein JN American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg (Am) 2008;90(4):700–707. doi: 10.2106/JBJS.G.00517. [DOI] [PubMed] [Google Scholar]
- 5.张雨, 杨旭辉, 曾秋铭 长型和短型髓内钉用于不稳定转子间骨折疗效比较的 meta 分析. 重庆医学. 2020;49(14):2390–2395, 2403. [Google Scholar]
- 6.Roberts KC, Brox WT, Jevsevar DS, et al Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–137. doi: 10.5435/JAAOS-D-14-00432. [DOI] [PubMed] [Google Scholar]
- 7.Matre K, Havelin LI, Gjertsen JE, et al Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian Hip Fracture Register. Injury. 2013;44(6):735–742. doi: 10.1016/j.injury.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 8.Yu X, Wang H, Duan X, et al Intramedullary versus extramedullary internal fixation for unstable intertrochanteric fracture, a meta-analysis. Acta Orthop Traumatol Turc. 2018;52(4):299–307. doi: 10.1016/j.aott.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Müller F, Galler M, Zellner M, et al Peri-implant femoral fractures: The risk is more than three times higher within PFN compared with DHS. Injury. 2016;47(10):2189–2194. doi: 10.1016/j.injury.2016.04.042. [DOI] [PubMed] [Google Scholar]
- 10.Daner WE, Owen JR, Wayne JS, et al Biomechanical evaluation of the risk of secondary fracture around short versus long cephalomedullary nails. Eur J Orthop Surg Traumatol. 2017;27(8):1103–1108. doi: 10.1007/s00590-017-1989-6. [DOI] [PubMed] [Google Scholar]
- 11.Norris R, Bhattacharjee D, Parker MJ Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: a systematic review of 13, 568 patients. Injury. 2012;43(6):706–711. doi: 10.1016/j.injury.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 12.Boone C, Carlberg KN, Koueiter DM, et al Short versus long intramedullary nails for treatment of intertrochanteric femur fractures (OTA 31-A1 and A2) J Orthop Trauma. 2014;28(5):e96–e100.96-100. doi: 10.1097/BOT.0b013e3182a7131c. [DOI] [PubMed] [Google Scholar]
- 13.Kleweno C, Morgan J, Redshaw J, et al Short versus long cephalomedullary nails for the treatment of intertrochanteric hip fractures in patients older than 65 years. J Orthop Trauma. 2014;28(7):391–397. doi: 10.1097/BOT.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 14.Lindvall E, Ghaffar S, Martirosian A, et al Short versus long intramedullary nails in the treatment of pertrochanteric hip fractures: Incidence of ipsilateral fractures and costs associated with each implant . J Orthop Trauma. 2016;30(3):119–124. doi: 10.1097/BOT.0000000000000420. [DOI] [PubMed] [Google Scholar]
- 15.Dunn J, Kusnezov N, Bader J, et al Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31-A1, A2 and A3): a systematic review . J Orthop Traumatol. 2016;17(4):361–367. doi: 10.1007/s10195-016-0405-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan LWM, Gardner AW, Wong MK, et al Non-prosthetic peri-implant fractures: classification, management and outcomes. Arch Orthop Trauma Surg. 2018;138(6):791–802. doi: 10.1007/s00402-018-2905-1. [DOI] [PubMed] [Google Scholar]
- 17.Insall JN, Ranawat CS, Aglietti P, et al A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg (Am) 1976;58(6):754–765. doi: 10.2106/00004623-197658060-00003. [DOI] [PubMed] [Google Scholar]
- 18.Pagnani MJ, Lyden JP Postoperative femoral fracture after intramedullary fixation with a Gamma nail: case report and review of the literature. J Trauma. 1994;37(1):133–137. doi: 10.1097/00005373-199407000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Bridle SH, Patel AD, Bircher M, et al Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg (Br) 1991;73(2):330–334. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 20.Socci AR, Casemyr NE, Leslie MP, et al Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99-B(1):128–133. doi: 10.1302/0301-620X.99B1.BJJ-2016-0134.R1. [DOI] [PubMed] [Google Scholar]
- 21.Osnes EK, Lofthus CM, Falch JA, et al More postoperative femoral fractures with the Gamma nail than the sliding screw plate in the treatment of trochanteric fractures. Acta Orthop Scand. 2001;72(3):252–256. doi: 10.1080/00016470152846574. [DOI] [PubMed] [Google Scholar]
- 22.Wang CJ, Brown CJ, Yettram AL, et al Intramedullary nails: some design features of the distal end. Med Eng Phys. 2003;25(9):789–794. doi: 10.1016/S1350-4533(03)00098-5. [DOI] [PubMed] [Google Scholar]
- 23.Duncan CP, Masri BA Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 24.Dhar SA, Halwai MA, Wani MI, et al Operative management of a subtrochanteric fracture in severe osteoporosis. A case report. Cases J. 2008;1(1):193. doi: 10.1186/1757-1626-1-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruchholtz S, El-Zayat B, Kreslo D, et al Less invasive polyaxial locking plate fixation in periprosthetic and peri-implant fractures of the femur—a prospective study of 41 patients. Injury. 2013;44(2):239–248. doi: 10.1016/j.injury.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 26.陈挺, 田立杰, 汤欣 LISS 治疗股骨近端骨折术后髓内钉远端再骨折. 实用骨科杂志. 2017;23(8):736–738. [Google Scholar]
- 27.Kim HK, Noh KC, Chung KJ, et al Use of Huckstep nail in the periimplant femoral shaft fracture. Indian J Orthop. 2012;46(6):718–720. doi: 10.4103/0019-5413.104240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perren SM, Fernandez Dell’Oca A, Lenz M, et al Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech. 2011;78(3):190–199. [PubMed] [Google Scholar]
- 29.Apivatthakakul T, Phornphutkul C, Bunmaprasert T, et al Percutaneous cerclage wiring and minimally invasive plate osteosynthesis (MIPO): a percutaneous reduction technique in the treatment of Vancouver type B1 periprosthetic femoral shaft fractures. Arch Orthop Trauma Surg. 2012;132(6):813–822. doi: 10.1007/s00402-012-1489-4. [DOI] [PubMed] [Google Scholar]