Abstract
Backgroud
Recent literature suggests that three-dimensional magnetic resonance imaging (3D MRI) can replace 3D computed tomography (3D CT) when evaluating glenoid bone loss in patients with shoulder instability. We aimed to examine if 2D MRI in conjunction with a validated predictive formula for assessment of glenoid height is equivalent to the gold standard 3D CT scans for patients with recurrent glenohumeral instability.
Methods
Patients with recurrent shoulder instability and available imaging were retrospectively reviewed. Glenoid height on 3D CT and 2D MRI was measured by two blinded raters. Difference and equivalence testing were performed using a paired t-test and two one-sided tests, respectively. The interclass correlation coefficient (ICC) was used to test for interrater reliability, and percent agreement between the measurements of one reviewer was used to assess intrarater reliability.
Results
Using an equivalence margin of 1 mm, 3D CT and 2D MRI were found to be different (p = 0.123). The mean glenoid height was significantly different when measured on 2D MRI (39.09 ± 2.93 mm) compared to 3D CT (38.71 ± 2.89 mm) (p = 0.032). The mean glenoid width was significantly different between 3D CT (30.13 ± 2.43 mm) and 2D MRI (27.45 ± 1.72 mm) (p < 0.001). The 3D CT measurements had better interrater agreement (ICC, 0.91) than 2D MRI measurements (ICC, 0.8). intrarater agreement was also higher on CT.
Conclusions
Measurements of glenoid height using 3D CT and 2D MRI with subsequent calculation of the glenoid width using a validated methodology were not equivalent, and 3D CT was superior. Based on the validated methods for the measurement of glenoid bone loss on advanced imaging studies, 3D CT study must be preferred over 2D MRI in order to estimate the amount of glenoid bone loss in candidates for shoulder stabilization surgery and to assist in surgical decision-making.
Keywords: Images, Three dimensional imaging, Magnetic resonance imaging, Computed tomography dislocation, Glenohumeral
Recurrent shoulder instability may be associated with various degrees of glenoid bone loss.1,2) Based on the amount of glenoid bone loss, the surgeon should determine if a soft-tissue stabilization procedure is adequate to prevent recurrent shoulder instability or bony augmentation is necessary.2,3) A glenoid bone loss of greater than 20%–25% is predictive of poor clinical outcomes (recurrent shoulder instability and impaired shoulder function) following soft-tissue stabilization alone.4,5,6,7) This cutoff value for glenoid bone loss was found to be even lower in some studies, ranging from 13.5% to 17.5%.8,9)
Three-dimensional computed tomography (3D CT) is considered as the gold standard test for quantifying glenoid bone loss during preoperative planning in patients with recurrent glenohumeral instability. Magnetic resonance imaging (MRI) protocols were developed for the same purpose, with the advantage of avoiding the patient exposure to radiation.1,10,11) Based on the current literature, 2D and 3D MRI can be used to estimate the amount of glenoid bone loss in patients with recurrent shoulder instability; however, the 3D MRI seems to be more accurate.12) Unfortunately, 3D MRI is not widely available in the clinical setting.
Owens et al.13) developed a predictive formula to determine glenoid bone loss (glenoid height and width) based on the MRI scans of more than 1,200 shoulders, with only using a ruler and the 2D MRI of the injured shoulder.13) A similar formula has been developed for 3D CT scans.12,14) To our knowledge, there has not been a direct comparison of the accuracy and reliability in measuring glenoid bone loss using these predictive formulas between 2D MRI and 3D CT.12) Two previous studies that compared the glenoid bone loss on 2D MRI versus 3D CT scans used the Pico measurement technique,11,15) and showed that 2D MRI was as reliable as 3D CT for this purpose.
The aim of this present study was to retrospectively evaluate if 2D MRI in conjunction with validated predictive formulas for the assessment of the glenoid width was equivalent to 3D CT for patients with recurrent glenohumeral instability. If 2D MRI could replace 3D CT during the evaluation of candidates for shoulder stabilization surgery, it could protect the patient from an additional 2.06 mSv radiation exposure and decrease healthcare costs associated with redundant imaging tests.16)
METHODS
After receiving Institutional Review Board approval of the University of Southern California (IRB No. HS17-00155), we retrospectively identified any patient who had a diagnosis of recurrent glenohumeral joint instability and was evaluated with both a 2D MRI and a 3D CT osseous reconstruction study as part of the preoperative workup. Patients who had the imaging studies performed outside institutions were excluded. The 2D MRI image and 3D CT osseous reconstruction of the ipsilateral glenohumeral joint were analyzed by two readers (EW, a fellowship-trained musculoskeletal radiologist and AH, an orthopedic surgery trainee).
All images were analyzed preoperatively with an average time span of 93.06 days between two imaging tests. None of the patients sustained a shoulder dislocation during this period. Height measurements of the glenoid were attained using Vitrea Core ver. 6.9.68.1 (Vital Images, Minnetonka, MN, USA) for 3D CT images and Synapse 3D ver. 4.4.2 (Fujifilm Co., Tokyo, Japan) for 2D MRI images. MRI images with a slice thickness of 3–5 mm (3.54 on average) were captured using machines produced by 1 of 3 manufactures: GE Medical Systems' Signa Excite, Signa HDxt (Milwaukee, WI, USA), Siemens' Symphony (Erlangen, Germany), or Toshiba's Titan3T (Tokyo, Japan). All CT images were obtained using a Siemens Sensation 10 or Biograph 64 machine or a Toshiba Aquilion ONE machine (Tokyo, Japan) with a slice thickness of 0.5–2 mm (1.145 on average).
To make accurate measurements of the glenoid height after 3D CT osseous reconstruction, the humerus was subtracted using the sculpt function on the Vitrea Core software. Once the glenoid fossa was isolated, it was rotated to an en face position (sagittal oblique view). The ruler function was used to attain the height of the glenoid from the superior and inferior points of the articular surface of the glenoid (3D Euclidean distance), parallel to the scapular spine (Fig. 1) as described in the study by Moineau et al.17) After measuring the glenoid height, the glenoid width was calculated using the formulae proposed by Giles et al.,14) which differ slightly according to patient's sex (Table 1).
Fig. 1. Glenoid height measurement using three-dimensional reconstruction of glenoid fossa. After subtracting the humeral head, the glenoid fossa was rotated to an en face view. The glenoid fossa height was then measured and recorded along its longest axis from the superior articular surface to the inferior articular surface, in parallel to the scapular spine.
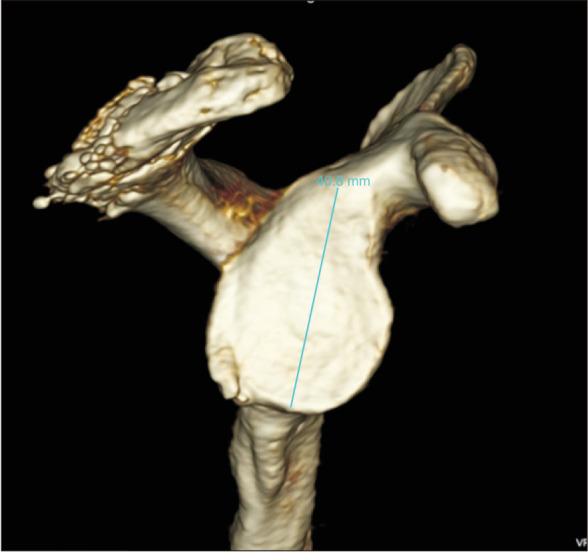
Table 1. Glenoid Width Based on Glenoid Height on CT.
| Variable | Formula |
|---|---|
| Male | W = 2 / 3 × H + 5 mm |
| Female | W = 2 / 3 × H + 3 mm |
CT: computed tomography, W: width, H: height.
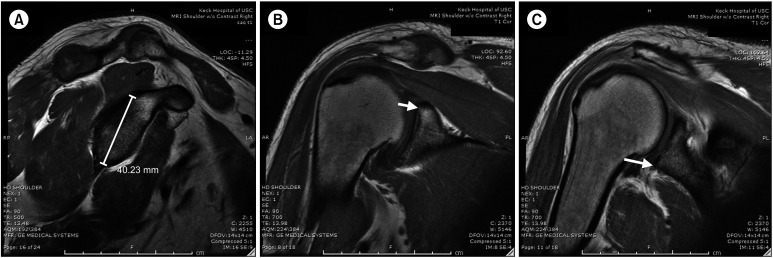
To measure the height of the glenoid fossa using 2D MRI images, measurements were taken using sagittal T1-weighted or sagittal T1-weighted fat-saturated images. A sagittal series does not always provide a single image in which the superior and inferior glenoid are both visualized. In order to accurately measure the glenoid height on the sagittal series, the superior and inferior articular surfaces of the glenoid fossa were localized and confirmed on the coronal images of the glenoid. The crosshatch feature in the Synapse 3D software allows localization (can accurately display a given point on the sagittal images on both the coronal and axial series). This permits the reader to accurately determine that the ruler head is at the superior and inferior articular surfaces of the glenoid (Fig. 2). Once the height of the glenoid was attained, the glenoid width was calculated according to the formulae proposed by Owens et al.13)
Fig. 2. (A) Sagittal T1-weighted magnetic resonance imaging (MRI) with glenoid height. The ruler head was measured from the superior to inferior articular surfaces of the glenoid on the coronal image for confirmation. (B) Coronal T1-weighted MRI with superior glenoid labelled. The superior glenoid is indicated by the white arrow. Using the crosshatch localization feature, confirmation of the glenoid height was attained on the sagittal image. (C) Coronal T1-weighted MRI with inferior glenoid labelled. The inferior glenoid is indicated by the white arrow. Using the crosshatch localization feature, confirmation of the glenoid height was attained on the sagittal image.
Statistical Analysis
Using the statistical techniques of Stillwater et al.1) as reference, two one-sided tests (TOST) for equivalence were used with an equivalence margin of 1 mm for measurement and 1% for percentage bone loss. The equivalence margin of −1 to +1 was decided prior to including any patients in order to avoid any potential bias. Statistical significance was determined using p < 0.05. Paired t-tests were performed in order to determine if there was a statistical difference between the two measurement techniques (3D CT vs. 2D MRI). Significance for the paired t-tests was determined using p < 0.1.11) The interclass correlation coefficient (ICC) was used to test for interrater reliability (Table 2). The intrarater reliability (Table 2) was reported as percent agreement between two separate measurements performed by one of the reviewers.
Table 2. Accepted Threshold Values for Strength of Agreement Based on ICC.
| Value of ICC | Reliability |
|---|---|
| < 0.50 | Poor |
| 0.50–0.74 | Moderate |
| 0.75–0.90 | Good |
| > 0.90 | Excellent |
ICC: interclass correlation coefficient.
RESULTS
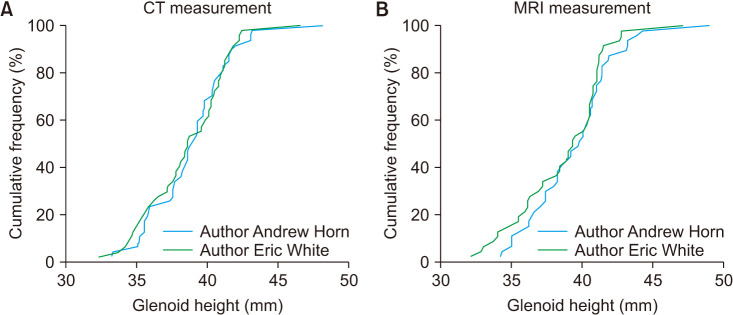
Forty-seven patients (31 men and 16 women) met the inclusion criteria and 47 shoulders were analyzed. The mean patient age was 45.1 ± 19.9 years (range, 15–87 years) at the time of examination. Using a null hypothesis whereby the 3D CT and 2D MRI techniques were not equivalent for determining the glenoid height, the TOST analysis failed to reject the null hypothesis since the calculated confidence interval (CI) of the TOST fell outside of the preset equivalence margin (95% CI, −1.075 to 0.475; upper and lower bounds, −1 to +1; p = 0.123). The mean glenoid height was significantly different when measured on 2D MRI (39.09 ± 2.93 mm) compared to 3D CT (38.71 ± 2.89 mm) (p = 0.032). Further, the calculated mean glenoid width was significantly different between 3D CT (30.13 ± 2.43 mm) and 2D MRI (27.45 ± 1.72 mm) examinations (p < 0.001). There was no difference in the calculated mean glenoid width and the glenoid width measured directly on the CT scan (30.13 ± 2.43 and 30.04 ± 2.4 respectively, p = 0.857). The calculated mean glenoid width and the glenoid width measured directly on MRI were also similar (27.45 ± 1.72 mm and 27.23 ± 1.6 mm, respectively, p = 0.522). The ICC between the two raters in measuring the glenoid height on 3D CT was 0.91 (excellent interrater reliability) and on MRI was 0.8 (good interrater reliability) (Fig. 3). The intrarater agreement was 92% for CT scan and 91% for MRI measurement.
Fig. 3. (A) Interclass correlation coefficient (ICC) for computed tomography (CT) measurement of the glenoid height (ICC, 0.91). (B) ICC for magnetic resonance imaging (MRI) measurement of the glenoid height (ICC, 0.8).
DISCUSSION
This study showed that 2D MRI is not equivalent to 3D CT reconstruction for estimating glenoid bone loss in patients with recurrent glenohumeral instability. Our measurements were based on previously published methodologies and formulas where the glenoid width was calculated based on the glenoid height measurement.13,14) Our results revealed superior interrater reliability for glenoid height measurement on 3D CT reconstruction (ICC, 0.91) as compared to 2D MRI (ICC, 0.8).
Several MRI (2D and 3D) and CT (2D and 3D) protocols have been proposed for the evaluation of glenoid bone loss in patients with recurrent glenohumeral joint instability.3,12,18,19,20) However, in a recent systematic review, 3D MRI seemed to be more accurate than 2D MRI (100% and 71%, respectively) for the measurement of glenoid bone loss in patients with anterior glenohumeral instability.12) In the study, 3D CT was used as the reference test in the majority of cases.12) According to the authors, the two most commonly reported imaging techniques across the included articles were the glenoid width and Pico surface area.12) In the current study, we focused on the comparison of glenoid height and calculated width between 2D MRI and 3D CT and no agreement between the two imaging modalities was observed. It was found that 3D CT, which is currently the gold standard for estimating glenoid bone loss in shoulder instability, was superior.
Only a few clinical studies have compared the amount of glenoid bone loss on 2D MRI versus 3D CT. Stecco et al.15) found a similar percentage of glenoid bone loss using the Pico technique on 2D MRI and 3D CT scans (4.38% and 4.34%) in a group of 23 patients who had experienced one or more posttraumatic glenohumeral dislocations. In addition, the authors reported a good interobserver agreement (k > 0.81) for both imaging studies. Using the Pico technique, Markenstein et al.11) also compared 3D CT and 2D MRI arthrography in measuring the amount of glenoid bone loss in patients with anterior shoulder instability. Their results showed a moderate agreement between CT and MRI, with the Bland-Altman plot showing 89% of measured differences within 1 standard deviation. In this study, the interobserver agreement was good to excellent for both 3D CT and 2D MRI; however, 3D CT had superior intraobserver reliability.
Our results did not agree with the findings of these last two studies.11,15) We found that 2D MRI was inferior to 3D CT in estimating the glenoid height and width in patients with recurrent shoulder instability. Both of these previous studies used the Pico technique for calculating the percentage glenoid bone loss.11,15) We measured the glenoid height on 3D CT using the ruler function within Vitrea Core software following humeral head subtraction, while the glenoid height for 2D MRI was measured using the ruler function in Synapse 3D software for 2D MRI. As mentioned above, the glenoid width was calculated based on previously validated formulas for both MRI and 3D CT. The percentage of glenoid bone loss was not calculated in our study, which precludes any direct comparison with previous reports. Further, the interrater reliability (Lin's concordance correlation coefficient) was higher when the glenoid height was measured on 3D CT (0.92, moderate agreement) than on 2D MRI (0.79, poor agreement). Accordingly, Markenstein et al.11) reported a slightly superior interrater reliability for the 3D CT compared to 2D MRI when measuring glenoid bone loss.
Stillwater et al.1) proposed that 3D MRI osseous reconstruction of the glenohumeral joint using a 3D isotropic volumetric interpolated breathhold examination sequencing is equivalent to 3D CT reconstruction of the glenohumeral joint. In this study, multiple measurements were attained for both the 3D MRI and 3D CT scan: glenoid height and width, humeral head height and width, Hill-Sachs lesion side (if present), percent humeral head loss (if present), size of glenoid bone loss (if present), and percent glenoid bone loss (if present). Though results proved there to be no statistically significant difference between 3D MRI and 3D CT for any of the measurements attained, the 3D MRI technique detailed by Stillwater et al.1) required extra time for construction due to additional sequencing and post-processing. We examined if a previously validated but simpler technique could be used for the measurement of glenoid height on 2D MRI, while the glenoid width could be calculated using previously validated formulas. We found that 2D MRI was not equivalent to the 3D CT scan in measuring the glenoid height, with 3D being more reliable. As mentioned above, the glenoid width and Pico methods are mostly used to estimate the amount of glenoid bone loss on CT (2D and 3D) and MRI (2D and 3D).
Several limitations might have affected the validity of our results. First, this was a retrospective analysis of a small patient sample, which was identified through medical record search, and some participants were probably missed. Second, there was a risk of inaccurate osseous assessment due to poor image quality on 2D MRI. Measurements may be improved with a universal thickness of 3 mm. With increased quality, there may be less variance between raters and the glenoid height may be more equivalent to what is measured using 3D CT. Further, we focused on the glenoid height and width without estimating the percentage of glenoid bone loss and, therefore, our results were not comparable with those of previous studies. Finally, although we identified statistically significant differences in the measurement of glenoid bone loss between 3D CT and 2D MRI, we are unsure if these differences were clinically meaningful. Further research is necessary to answer this question. Lastly, the result of this study might have been affected by the inferior quality of 2D MRI images compared to 3D CT scan. Therefore, clinicians should always consider the image quality of each study during the interpretation of the results from the existing studies.
Measurements of the glenoid height using 3D CT and 2D MRI, with subsequent calculation of the glenoid width using validated methodology, were not equivalent. Compared to 2D MRI, 3D CT provided the more reliable and accurate measurement of glenoid bone loss. Based on the validated methods for the measurement of glenoid bone loss on advanced imaging studies, 3D CT study must be preferred over 2D MRI in order to estimate the amount of glenoid bone loss in candidates for shoulder stabilization surgery and to assist in surgical decision making.
ACKNOWLEDGEMENTS
Authors would like to acknowledge The Cappo Family Research Fund for the continuous support in our research efforts.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Stillwater L, Koenig J, Maycher B, Davidson M. 3D-MR vs. 3D-CT of the shoulder in patients with glenohumeral instability. Skeletal Radiol. 2017;46(3):325–331. doi: 10.1007/s00256-016-2559-4. [DOI] [PubMed] [Google Scholar]
- 2.Baudi P, Rebuzzi M, Matino G, Catani F. Imaging of the unstable shoulder. Open Orthop J. 2017;11:882–896. doi: 10.2174/1874325001711010882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beaulieu-Jones BR, Peebles LA, Golijanin P, et al. Characterization of posterior glenoid bone loss morphology in patients with posterior shoulder instability. Arthroscopy. 2019;35(10):2777–2784. doi: 10.1016/j.arthro.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 5.Levy DM, Cole BJ, Bach BR., Jr History of surgical intervention of anterior shoulder instability. J Shoulder Elbow Surg. 2016;25(6):e139–e150. doi: 10.1016/j.jse.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Yamamoto N, Itoi E, Abe H, et al. Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med. 2009;37(5):949–954. doi: 10.1177/0363546508330139. [DOI] [PubMed] [Google Scholar]
- 7.Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000;82(1):35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Shaha JS, Cook JB, Song DJ, et al. Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43(7):1719–1725. doi: 10.1177/0363546515578250. [DOI] [PubMed] [Google Scholar]
- 9.Shin SJ, Kim RG, Jeon YS, Kwon TH. Critical value of anterior glenoid bone loss that leads to recurrent glenohumeral instability after arthroscopic Bankart repair. Am J Sports Med. 2017;45(9):1975–1981. doi: 10.1177/0363546517697963. [DOI] [PubMed] [Google Scholar]
- 10.Vopat BG, Cai W, Torriani M, et al. Measurement of glenoid bone loss with 3-dimensional magnetic resonance imaging: a matched computed tomography analysis. Arthroscopy. 2018;34(12):3141–3147. doi: 10.1016/j.arthro.2018.06.050. [DOI] [PubMed] [Google Scholar]
- 11.Markenstein JE, Jaspars KC, van der Hulst VP, Willems WJ. The quantification of glenoid bone loss in anterior shoulder instability; MR-arthro compared to 3D-CT. Skeletal Radiol. 2014;43(4):475–483. doi: 10.1007/s00256-013-1780-7. [DOI] [PubMed] [Google Scholar]
- 12.Walter WR, Samim M, LaPolla FW, Gyftopoulos S. Imaging quantification of glenoid bone loss in patients with glenohumeral instability: a systematic review. AJR Am J Roentgenol. 2019;212(5):1096–1105. doi: 10.2214/AJR.18.20504. [DOI] [PubMed] [Google Scholar]
- 13.Owens BD, Burns TC, Campbell SE, Svoboda SJ, Cameron KL. Simple method of glenoid bone loss calculation using ipsilateral magnetic resonance imaging. Am J Sports Med. 2013;41(3):622–624. doi: 10.1177/0363546512472325. [DOI] [PubMed] [Google Scholar]
- 14.Giles JW, Owens BD, Athwal GS. Estimating glenoid width for instability-related bone loss: a CT evaluation of an MRI formula. Am J Sports Med. 2015;43(7):1726–1730. doi: 10.1177/0363546515581468. [DOI] [PubMed] [Google Scholar]
- 15.Stecco A, Guenzi E, Cascone T, et al. MRI can assess glenoid bone loss after shoulder luxation: inter- and intra-individual comparison with CT. Radiol Med. 2013;118(8):1335–1343. doi: 10.1007/s11547-013-0927-x. [DOI] [PubMed] [Google Scholar]
- 16.Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91(8):1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 17.Moineau G, Levigne C, Boileau P, Young A, Walch G French Society for Shoulder & Elbow (SOFEC) Three-dimensional measurement method of arthritic glenoid cavity morphology: feasibility and reproducibility. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S139–S145. doi: 10.1016/j.otsr.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Dekker TJ, Peebles LA, Goldenberg BT, Millett PJ, Bradley JP, Provencher MT. Location of the glenoid defect in shoulders with recurrent posterior glenohumeral instability. Am J Sports Med. 2019;47(13):3051–3056. doi: 10.1177/0363546519876282. [DOI] [PubMed] [Google Scholar]
- 19.Lansdown DA, Cvetanovich GL, Verma NN, et al. Automated 3-dimensional magnetic resonance imaging allows for accurate evaluation of glenoid bone loss compared with 3-dimensional computed tomography. Arthroscopy. 2019;35(3):734–740. doi: 10.1016/j.arthro.2018.10.119. [DOI] [PubMed] [Google Scholar]
- 20.Parada SA, Paynter JW, Pare DW, et al. Use of the contralateral glenoid for calculation of glenoid bone loss: a cadaveric anthropometric study. Arthroscopy. 2020;36(6):1517–1522. doi: 10.1016/j.arthro.2020.01.049. [DOI] [PubMed] [Google Scholar]