Abstract
Objective:
To investigate the accuracy of panoramic radiography (PR) in diagnosing maxillary sinus-root relationships (SRRs).
Materials and Methods:
PubMed, EMBASE, CENTRAL, Web of Science, ScienceDirect, CBM, Baidu Scholar, and SIGLE were searched. The studies comparing the diagnostic accuracy of PR and computed tomography/cone-beam computed tomography (CT/CBCT) for SRR were included.
Results:
Eleven studies were included. Meta-analyses showed that, for type I SRR, PR had the highest specificity, positive likelihood ratio (+LR), diagnostic odds ratio (DOR), and area under the curve (AUC), with a high sensitivity and a low negative LR (−LR). For type IV, PR had a high DOR and AUC, with the highest sensitivity but a low +LR, the lowest –LR, and the lowest specificity. For type II, PR had the lowest AUC, with a low sensitivity, +LR, and DOR and a high −LR. For type III, PR had the lowest sensitivity, +LR, and DOR and the highest −LR. The distance from root tips to the maxillary sinus floor on PR was significantly longer (mean difference: −1.88 mm; 95% confidence interval: −2.19 to −1.57; P < .0001) than that on CT/CBCT.
Conclusions:
Currently available evidence suggests PR could be reliable for detecting type I SRR. PR has a good ability to confirm true type IV SRR but a poor ability to rule out false type IV SRR. For type II and III SRR, PR shows poor accuracy and tends to overestimate the extent of protrusion of the roots into the maxillary sinus. When PRs display type II, III, or IV SRR and related treatment is needed, CBCT should be used for further examinations.
Keywords: Cone-beam computed tomography, Diagnosis, Maxillary sinus, Meta-analysis, Panoramic radiography, Systematic review
INTRODUCTION
The maxillary sinus (MS) is the largest paranasal sinus, located in the posterior maxilla, and it has a close relationship with adjacent structures. With pneumatization, the MS floor (MSF) extends into the posterior alveolar process, creating protrusions of root apices into the sinus.1 According to recent studies with cone-beam computed tomography (CBCT), individuals greatly vary regarding MSF morphology and sinus-root relationship (SRR). The incidence of roots protruding into the MS was 0% to 3.07%, 2.86% to 14.77%, 11.98% to 40.53%, and 9.6% to 44.70% for the first premolar, second premolar, first molar, and second molar, respectively.1–7
Complications regarding the SRR have been extensively reported in exodontia, endodontics, and implantology.1 An increasing number of studies regarding the influence of the SRR on orthodontic treatment have been conducted in recent years, reporting common complications such as tooth tipping, root resorption, prolonged treatment, and mini-screw risks.8–11 An accurate diagnosis of SRR is important for predicting the feasibility, quality, and duration of comprehensive treatment and helps in formulating appropriate techniques and remedies before providing orthodontic treatment.
Panoramic radiography (PR) is currently the most frequently prescribed radiography for orthodontists to obtain comprehensive information about the dentition and the relationship between the teeth and adjacent structures. PR has the advantages of being low cost, providing a low dose of radiation, and being able to show a full view of multiple structures bilaterally. However, it is two-dimensional and presents certain drawbacks such as superimposition, magnification, ghost images, blurring, and curved structure spreading. In contrast, CBCT is a three-dimensional, multiplanar, and thin-sliced radiography and overcomes the disadvantages of PR.1,12 The accuracy of linear measurements on CT/CBCT is comparable with that of macroscopic measurements.13,14 However, the cost and radiation dose of CT/CBCT are higher than those of PR.1,12
In the past decade, several studies comparing the diagnostic accuracy of PR and CT/CBCT for SRR have been conducted,12,15–24 but there has not been a systematic review. In the present study, CT/CBCT was used as the reference test, and a systematic review was carried out to investigate the diagnostic accuracy of PR for detecting SRR.
MATERIALS AND METHODS
This systematic review and meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) checklist.25 The literature search, data extraction, and quality assessment were performed independently by two authors. Any disagreements were resolved by discussion or by a third author.
Inclusion Criteria of Included Studies
Studies meeting the following criteria were considered eligible: (1) The study focused on permanent maxillary premolars and molars (except third molars) with fully formed apices and without periapical lesions. (2) The MSF was complete, not affected by disease or sinus augmentation. (3) The study compared the diagnostic accuracy of PR and CT/CBCT. (4) The study diagnosed SRR using the condensed classification proposed by Sharan and Madjar,12 namely, type I: the root tip is not in contact with the MSF; type II: the root tip and the MSF are at the same horizontal level, and the root tip is in contact with the MSF; type III: the root tip is above the bottom of MSF and is projecting laterally on or enveloped by the MSF, but the root tip is not protruding into the sinus; and type IV: the root tip is protruding into the sinus cavity. (5) The primary outcome was true-positive (index, reference both positive), false-positive (reference negative, index positive), false-negative (reference positive, index negative), and true-negative (index, reference both negative), and the secondary outcome was the distance measured from the root tip to the inferior wall of MS (“+” indicating the root into and “−” out of the MS). (6) The study was a clinical study.
Search Methods
An electronic search was undertaken in databases PubMed, EMBASE, CENTRAL, Web of Science, ScienceDirect, CBM, Baidu Scholar, and the System for Information on Grey Literature in Europe (SIGLE). MeSH terms were combined with free-text words optimized for each database. The electronic search was updated on November 29, 2017, and had no language restrictions (Table 1). In addition, a manual search of reference lists of relevant studies was carried out for supplemental information.
Table 1.
Search Strategies for All Databases (Updated on November 29, 2017)a
| Step |
PubMed, CENTRAL, EMBASE, CBM |
Web of Science, ScienceDirect, Baidu Scholar, SIGLE |
| 1 | “Maxillary Sinus”[Mesh]) OR maxillary sinus | Maxillary Sinus |
| 2 | Cone-Beam Computed Tomography[MeSH] OR Cone-Beam Computed Tomography OR Cone-beam CT OR CBCT | Cone-beam computed tomography OR Cone-beam CT OR CBCT |
| 3 | “Radiography, Panoramic”[Mesh] OR Panoramic* OR Pantomograph* OR Orthopantomograph* | Panoramic* OR Pantomograph* |
| 4 | 1 AND 2 AND 3 | 1 AND 2 AND 3 |
CENTRAL indicates Cochrane Central Register of Controlled Trials; CBM, Chinese Biomedical Literature Database; SIGLE, System for Information on Grey Literature in Europe; MeSH, Medical Subject Headings.
Data Extraction and Analysis
Information about the characteristics and outcomes of the included studies was extracted. Specifically, the study characteristics were author, publication year, country, age, gender, sample size, tooth type, SRR classification, extractable SRR type, synthesis unit, and the index and reference test. The outcomes were the items defined in the inclusion criteria above.
Quality Assessment
The Quality Assessment of Studies of Diagnostic Accuracy-2 (QUADAS-2) was adopted for the quality assessment.26 The assessment comprised the following four domains, all of which were evaluated for a risk of bias and the first three of which were assessed for applicability concerns: patient selection, index test, reference standard, and flow and timing.
Statistical Analysis
STATA 12.0 and RevMan 5.3 were used for meta-analyses. The outcomes, including sensitivity and specificity, were statistically pooled using a bivariate model and were adopted as effect measurements. The positive likelihood ratio (+LR), negative LR (−LR), and diagnostic odds ratio (DOR) were obtained according to the summary estimates of sensitivity and specificity. The summary reviewer-operator characteristic curve and the area under the curve (AUC) were used to reflect diagnostic efficiency. For continuous data, the meta-analysis was calculated by specifying mean difference (MD). The heterogeneity of the included studies was assessed with the I2 statistic. A random-effect model was used for the meta-analysis if the heterogeneity was high (I2 >50%). Otherwise (ie, I2 ≤50%), a fixed-effect model was employed. Subgroup analyses and meta-regression were used to determine the potential sources of heterogeneity. Sensitivity analyses were performed to evaluate the robustness of the pooled results. The publication bias was assessed using funnel plots and the Deeks test.27
RESULTS
Description of Included Studies
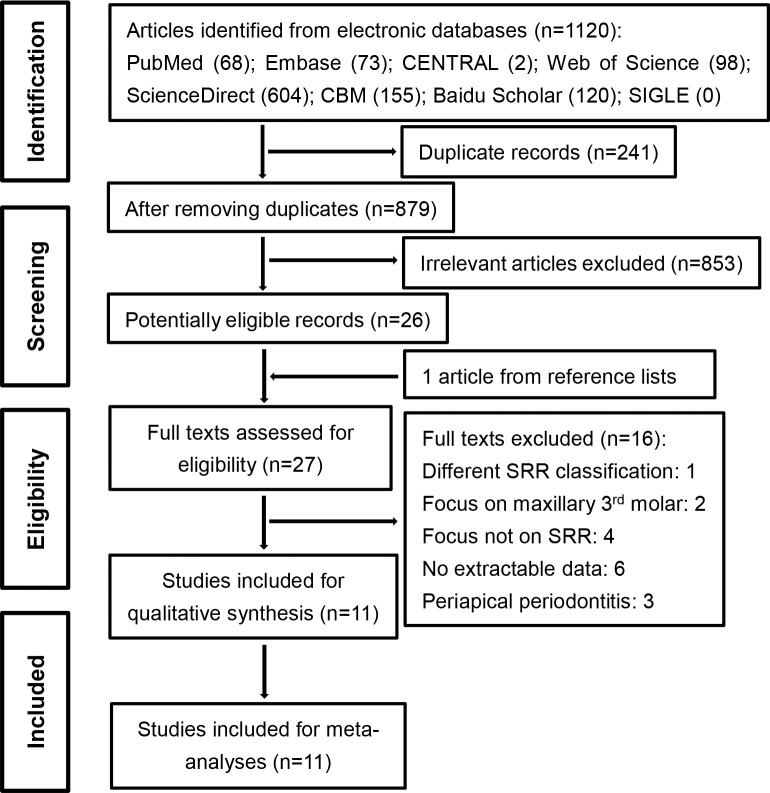
A total of 879 records were initially retrieved from the literature search. Finally, 11 studies12,15–24 were included in the systematic review and meta-analysis (Figure 1). Among the enrolled studies, 10 reported the diagnostic efficacy for type I, with a sample size of 1826 teeth and 4225 roots12,15–22,24; 10 investigated type II, with 1826 teeth and 4225 roots12,15–22,24; 8 investigated type III, with 1438 teeth and 3837 roots12,15,17,18,20–22,24; and 10 reported information on type IV, with 1658 teeth and 4225 roots.12,15,17–24 Among all studies, 9 used CBCT,15–19,21–24 while 212,20 used CT as the reference test. In addition, five studies reported the distance from the root tips to the MSF (Tables 2 and 3).12,15,17,20,24
Figure 1.
Flow diagram of the study inclusion process.
Table 2.
Summary of Characteristics of Included Studiesa
| Study ID |
Country |
Age, Year |
Gender, M/F |
Tooth Type |
SRR Classification |
Index Test (Parameters) |
Reference Test (Parameters) |
| Sharan and Madjar (2006)12 | Israel | 40 | 55/25 | Pre-/molar | Sharan | PR (Gendex Orthoralix-S) | CT (Phillips Brilliance 40: 120 kVp, 60 mA, slice spacing 2 mm, slice thickness 1.3 mm) |
| Lin (2009)15 | Taiwan | 50.4 | 42/38 | Pre-/molar | Sharan | PR (Cranex Tome CEPH) | CBCT (i-CAT: 120 kVp, 8 mA, slice spacing 0.4 mm, slice thickness 0.4 mm) |
| Bokkasam et al. (2015)16 | India | — | — | Pre-/molar | Condensed Sharan | PR | CBCT (Kodak 9000C) |
| Roque-Torres et al. (2015)17 | Brazil | 22 | 78/31 | Pre-/molar | Sharan | PR (DOP 100: 57–60 kVp, 2 mA, 17.6 s) | CBCT (Classic i-CAT: 120 kVp, 8 mA, 40 s, voxel size 0.3 mm, FOV 23 × 17 cm) |
| Dehghani Tafti et al. (2015)18 | Iran | — | — | Pre-/molar | Sharan | PR | CBCT (Planmeca: 84 kVp, 12 mA, 14 s, FOV 8 × 8 cm) |
| Jung and Cho (2009)19 | Korea | 42.3 | 49/48 | Molar | Condensed Sharan | PR (Planmeca 2002 CC Proline) | CBCT (DCTPRO: 90 kVp, 4 mA, 24 s, FOV 20 × 14 cm) |
| Ali et al. (2012)20 | Iraq | 29 | 16/11 | Pre-/molar | Sharan | PR (Planmeca Dimax: 66 kVp, 10 mA, 18 s) | CT (Somatom: 130 kVp, 105 mA) |
| Fakhar et al. (2014)21 | Iran | — | — | Pre-/molar | Sharan | PR (Planmeca Proline: 64–68 kVp, 8-10 mA, 18 s) | CBCT (Planmeca 3D max: 82–84 kVp, 12–14 mA, 12 s) |
| Lopes et al. (2016)22 | Brazil | — | — | Pre-/molar | Condensed Sharan | PR (DOP100) | CBCT (Picasso Trio) |
| Mi et al. (2016)23 | China | 19.7 | 42/68 | Pre-/molar | Condensed Sharan | PR | CBCT (Morita Micro CT: 87 kVp, 5.5 mA, 17.5 s, slice spacing 0.125 mm, slice thickness 0.125 mm) |
| Kalkur et al. (2017)24 | India | 18-45 | 49/36 | Pre-/molar | Sharan | PR (Kodak 9000C: 70–74 kVp, 14.3–15.1 mA, 15.1 s) | CBCT (Kodak 9000C: 70–80 kVp, 10–10.8 mA, 24 s) |
M/F indicates male/female; SRR, maxillary sinus-root relationship; PR, panoramic radiography; CT, computed tomography; CBCT, cone-beam computed tomography; FOV, field of view.
Table 3.
Results of Individual Studiesa
| Study ID |
Sample Size |
Extractable SRR Type |
Diagnostic Outcomes |
Unit |
Distance Measure, Mean (SD), mm |
||||||
| People |
Teeth |
Roots |
TP |
FP |
FN |
TN |
PR |
CT/CBCT |
|||
| Sharan and Madjar (2006)12 | 80 | — | 422 | I | 85 | 2 | 20 | 315 | Root | 3.11 (2.54) | 1.48 (1.50) |
| II | 50 | 9 | 69 | 294 | |||||||
| III | 26 | 35 | 72 | 289 | |||||||
| IV | 93 | 122 | 7 | 200 | |||||||
| Lin (2009)15 | 80 | 324 | 723 | I | 337 | 14 | 85 | 287 | Root | 3.30 (2.45) | 2.10 (1.71) |
| II | 85 | 70 | 61 | 507 | |||||||
| III | 5 | 16 | 58 | 644 | |||||||
| IV | 79 | 117 | 13 | 514 | |||||||
| Bokkasam et al. (2015)16 | 30 | 388 | I | 59 | 19 | 36 | 274 | Root | — | — | |
| II | 205 | 34 | 71 | 78 | |||||||
| IV | 15 | 56 | 2 | 315 | |||||||
| Roque-Torres et al. (2015)17 | 109 | 872 | 1875 | I | 307 | 41 | 196 | 1331 | Root | 0.44 (3.06) | −1.56 (3.70) |
| II | 356 | 235 | 299 | 985 | |||||||
| III | 21 | 96 | 616 | 1142 | |||||||
| IV | 59 | 760 | 21 | 1035 | |||||||
| Dehghani Tafti et al. (2015)18 | 55 | 440 | 817 | I | 273 | 69 | 79 | 396 | Root | — | — |
| II | 148 | 65 | 147 | 457 | |||||||
| III | 85 | 34 | 19 | 679 | |||||||
| IV | 54 | 89 | 12 | 662 | |||||||
| Jung and Cho (2009)19 | 97 | 388 | — | I | 150 | 0 | 14 | 224 | Teeth | — | — |
| II | 39 | 13 | 9 | 327 | |||||||
| Ali et al. (2012)20 | 27 | 146 | — | I | 38 | 6 | 16 | 86 | Teeth | 4.65 (1.17) | 2.55 (1.20) |
| II | 34 | 12 | 36 | 64 | |||||||
| III | 3 | 21 | 14 | 108 | |||||||
| IV | 8 | 24 | 2 | 112 | |||||||
| Fakhar et al. (2014)21 | 117 | 452 | — | I | 154 | 10 | 18 | 270 | Teeth | — | — |
| II | 76 | 29 | 54 | 293 | |||||||
| III | 12 | 51 | 100 | 289 | |||||||
| IV | 19 | 101 | 19 | 313 | |||||||
| Lopes et al. (2016)22 | 46 | 330 | — | I | 85 | 11 | 24 | 210 | Teeth | — | — |
| II | 38 | 30 | 51 | 211 | |||||||
| III | 2 | 6 | 4 | 318 | |||||||
| IV | 111 | 47 | 15 | 157 | |||||||
| Mi et al. (2016)23 | 110 | 220 | 1119 | IV | 293 | 148 | 7 | 671 | Teeth | — | — |
| Kalkur et al. (2017)24 | 85 | 510 | — | I | 50 | 9 | 83 | 368 | Teeth | 6.30 (2.39) | 4.06 (2.27) |
| II | 73 | 59 | 116 | 262 | |||||||
| III | 9 | 28 | 128 | 345 | |||||||
| IV | 45 | 237 | 6 | 222 | |||||||
SRR indicates maxillary sinus-root relationship; TP, true-positive; FP, false-positive; FN, false-negative; TN, true-negative; PR, panoramic radiography; CT, computed tomography; CBCT, cone-beam computed tomography; SD, standard deviation; “+”,root into the MS; “−”, the root out of the MS.
Quality of Included Studies
Among the 11 included studies, one was assessed to have a low risk of bias17; five, a medium risk of bias15,18,20,22,23; and five, a high risk of bias.12,16,19,21,24 In terms of applicability, all studies were assessed to have low applicability concerns (Table 4).
Table 4.
Quality Assessment of the Included Studies According to the Quality Assessment of Studies of Diagnostic Accuracy-2a
| Study |
Risk of Bias |
Total |
Applicability Concerns |
Total |
|||||
| Patient Selection |
Index Test |
Reference Standard |
Flow and Timing |
Patient Selection |
Index Test |
Reference Standard |
|||
| Sharan and Madjar (2006)12 | High | Unclear | Unclear | Low | High | Low | Low | Low | Low |
| Lin (2009)15 | Unclear | Unclear | Unclear | Low | Medium | Low | Low | Low | Low |
| Jung and Cho (2009)19 | High | Unclear | Unclear | Low | High | Low | Low | Low | Low |
| Ali et al. (2012)20 | Unclear | Unclear | Unclear | Low | Medium | Low | Low | Low | Low |
| Fakhar et al. (2014)21 | High | Unclear | Unclear | Low | High | Unclear | Low | Low | Low |
| Bokkasam et al. (2015)16 | High | Unclear | Unclear | Low | High | Unclear | Low | Low | Low |
| Roque-Torres et al. (2015)17 | Low | Low | Low | Low | Low | Low | Low | Low | Low |
| DehghaniTafti et al. (2015)18 | Unclear | Unclear | Unclear | Low | Medium | Unclear | Low | Low | Low |
| Lopes et al. (2016)22 | High | Low | Low | Low | Medium | Unclear | Low | Low | Low |
| Mi et al. (2016)23 | Unclear | Unclear | Unclear | Low | Medium | Low | Low | Low | Low |
| Kalkur et al. (2017)24 | High | Unclear | Unclear | Low | High | Low | Low | Low | Low |
High indicates high risk; medium, medium risk; low, low risk.
SYNTHESIZED RESULTS OF DIAGNOSTIC ACCURACY
Qualitative Results of Diagnostic Accuracy
Synthesized results of diagnostic accuracy.
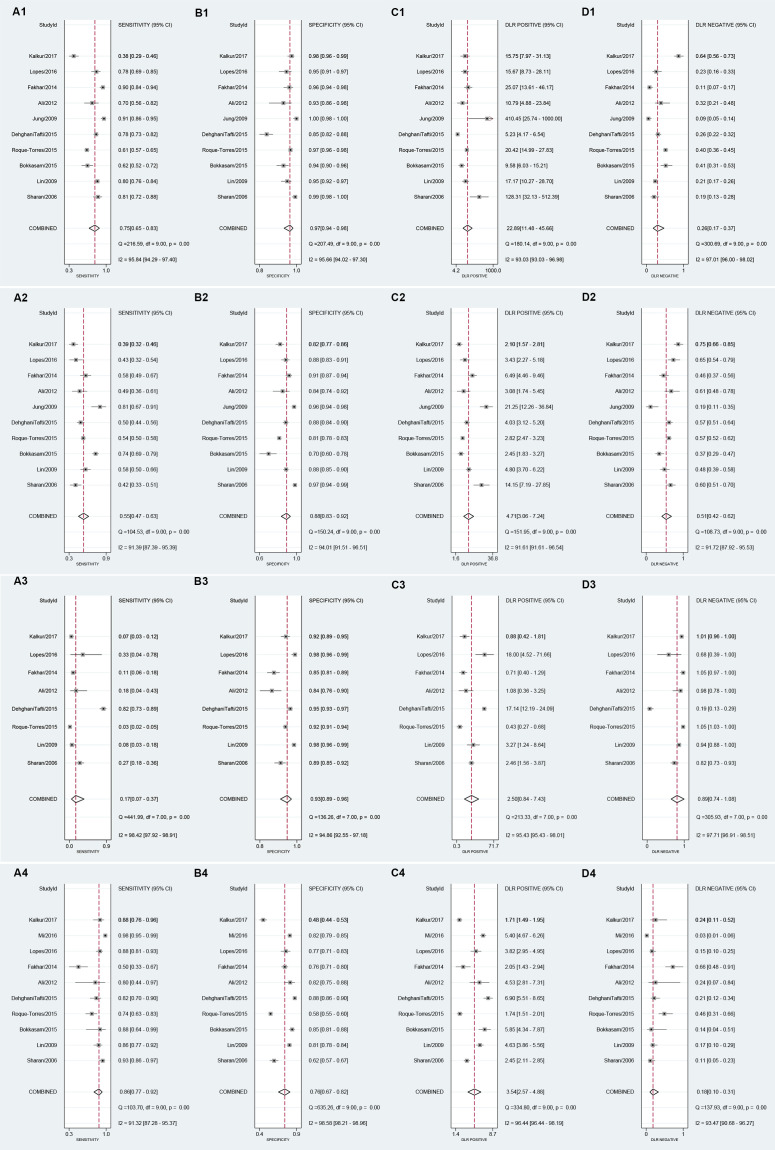
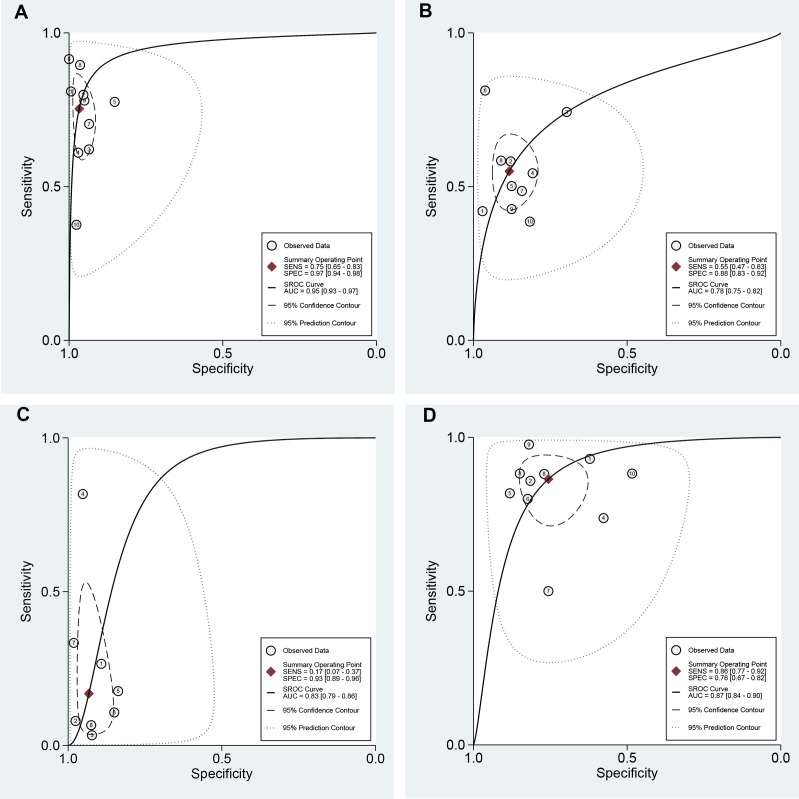
The pooled statistics (sensitivity, specificity, +LR, −LR, AUC, and DOR) are summarized in Table 5 and Figures 2 and 3.
Table 5.
Summary of Diagnostic Efficacy of PR for Different SRR Types
| Item |
Type I |
Type II |
Type III |
Type IV |
| Sen [95% CI] | 0.75 [0.65–0.83] | 0.55 [0.47–0.63] | 0.17 [0.07–0.37] | 0.86 [0.77–0.92] |
| Spe [95% CI] | 0.97 [0.94–0.98] | 0.88 [0.83–0.92] | 0.93 [0.89–0.96] | 0.76 [0.67–0.82] |
| +LR [95% CI] | 22.9 [11.5–45.7] | 4.7 [3.1–7.2] | 2.5 [0.8–7.4] | 3.5 [2.6–4.9] |
| −LR [95% CI] | 0.26 [0.17–0.37] | 0.51 [0.42–0.62] | 0.89 [0.74–1.08] | 0.18 [0.10–0.31] |
| AUC [95% CI] | 0.95 [0.93–0.97] | 0.78 [0.75–0.82] | 0.83 [0.79–0.86] | 0.87 [0.84–0.90] |
| DOR [95% CI] | 90 [35–229] | 9 [5–16] | 3 [1–10] | 20 [9–42] |
CI indicates confidence interval; Sen, sensitivity; Spe, specificity; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve; DOR, diagnostic odds ratio.
Figure 2.
Pooled indices for the diagnostic efficacy of panoramic radiography (PR) for type I SRR: (A1) sensitivity, (B1) specificity, (C1) positive likelihood ratio, (D1) negative likelihood ratio; for type II SRR: (A2) sensitivity, (B2) specificity, (C2) positive likelihood ratio, (D2) negative likelihood ratio; for type III SRR: (A3) sensitivity, (B3) specificity, (C3) positive likelihood ratio, (D3) negative likelihood ratio; and for type IV SRR: (A4) sensitivity, (B4) specificity, (C4) positive likelihood ratio, (D4) negative likelihood ratio.
Figure 3.
Summary receiver-operating characteristic (SROC) curves of panoramic radiography (PR) for (A) type I SRR, (B) type II SRR, (C) type III SRR, and (D) type IV SRR.
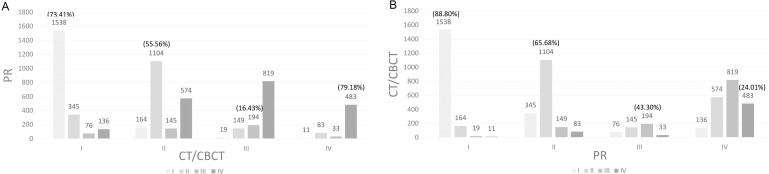
Classification change between index and reference test.
The pooled results indicated that, for the SRR diagnosed by CT/CBCT, PR showed an agreement of 73.41% for type I and 79.18% for type IV. However, 36.19% of type II and 69.35% of type III were given a higher SRR value on PR (Figure 4A). Comparatively, for the SRR diagnosed by PR, 88.80% of type I and 65.68% of type II were verified by CT/CBCT, but 49.33% of type III and 75.99% of type IV SRR were given a lower SRR value on CT/CBCT (Figure 4B).
Figure 4.
Classification changes in the sinus-root relationship between panoramic radiography and CBCT.
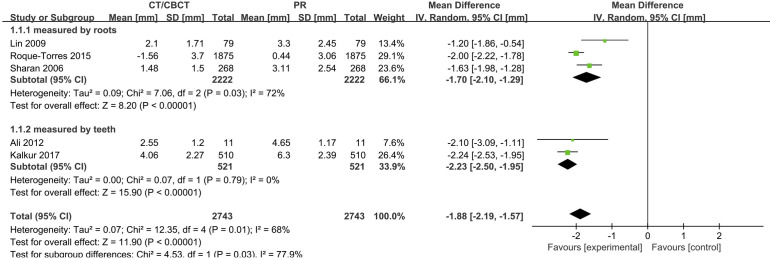
Distance From Root Tips to the MSF
The meta-analysis showed that the pooled MD [95% confidence interval (CI)] was −1.88 mm [−2.19, −1.57 mm], P = 0.00. The distance from the root tips to the MSF on CT/CBCT was significantly shorter than that on PR (Figure 5).
Figure 5.
Forest plot showing the mean difference (MD) of the distance from root tip to maxillary sinus floor between panoramic radiography and CBCT.
Subgroup Analysis and Meta-regression
First, the threshold effects were assessed. The Spearman correlation coefficients were −0.321 (P = .365), −0.042 (P = .907), −0.190 (P = .651), and −0.018 (P = .96) for type I, II, III, and IV, respectively. Therefore, no substantial threshold effects existed for any SRR types. Moreover, sources of heterogeneity among the enrolled studies were determined using meta-regression and subgroup analyses. The sample size (<50 subjects; >50 subjects), synthesis unit (root; tooth), SRR classification (Sharan's; condensed Sharan's), tooth type (premolar and molar; molar), reference test (CT; CBCT), publication year (in/before 2012; after 2012), and country (mid-east Asia; east Asia; south Asia; south America) were investigated with single covariate meta-regression. The results suggested only the tooth type significantly affected the diagnostic efficacy for type I SRR (P = .0081). A sensitivity analysis was performed by omitting the studies focusing on molars alone,19 and no significant changes were observed for the overall estimates (Table 6).
Table 6.
Results of Sensitivity Analysis and Subgroup Analysisa
| Item |
Sen [95% CI] |
Spe [95% CI] |
+LR [95% CI] |
−LR [95% CI] |
AUC [95% CI] |
DOR [95% CI] |
| Type I | ||||||
| Original estimate | 0.75 [0.65–0.83] | 0.97 [0.94–0.98] | 22.9 [11.5–45.7] | 0.26 [0.17–0.37] | 0.95 [0.93–0.97] | 90 [35–229] |
| Omitting molar alone | 0.73 [0.62–0.81] | 0.96 [0.93–0.97] | 17.4 [10.6–28.6] | 0.29 [0.20–0.40] | 0.95 [0.92–0.96] | 61 [31–118] |
| Omitting high-risk bias | 0.74 [0.67–0.80] | 0.94 [0.90–0.97] | 12.5 [7.6–20.5] | 0.28 [0.22–0.35] | 0.90 [0.87–0.93] | 45 [28–74] |
| Type II | ||||||
| Original estimate | 0.55 [0.47–0.63] | 0.88 [0.83–0.92] | 4.7 [3.1–7.2] | 0.51 [0.42–0.62] | 0.78 [0.75–0.82] | 9 [5–16] |
| Omitting molar alone | 0.52 [0.45–0.59] | 0.87 [0.81–0.91] | 4.0 [2.9–5.5] | 0.55 [0.48–0.63] | 0.75 [0.71–0.78] | 7 [5–11] |
| Omitting high-risk bias | 0.52 [0.48–0.55] | 0.86 [0.83–0.88] | 3.7 [3.0–4.4] | 0.56 [0.52–0.60] | 0.63 [0.59–0.67] | 7 [5–8] |
| Type III | ||||||
| Original estimate | 0.17 [0.07–0.37] | 0.93 [0.89–0.96] | 2.5 [0.8–7.4] | 0.89 [0.74–1.08] | 0.83 [0.79–0.86] | 3 [1–10] |
| Omitting molar alone | 0.17 [0.07–0.37] | 0.93 [0.89–0.96] | 2.5 [0.8–7.4] | 0.89 [0.74–1.08] | 0.83 [0.79–0.86] | 3 [1–10] |
| Omitting high-risk bias | 0.20 [0.05–0.55] | 0.95 [0.90–0.98] | 4.0 [0.9–18.8] | 0.84 [0.61–1.17] | 0.89 [0.86–0.91] | 5 [1–31] |
| Type IV | ||||||
| Original estimate | 0.86 [0.77–0.92] | 0.76 [0.67–0.82] | 3.5 [2.6–4.9] | 0.18 [0.10–0.31] | 0.87 [0.84–0.90] | 20 [9–42] |
| Omitting molar alone | 0.86 [0.77–0.92] | 0.76 [0.67–0.82] | 3.5 [2.6–4.9] | 0.18 [0.10–0.31] | 0.87 [0.84–0.90] | 20 [9–42] |
| Omitting high-risk bias | 0.88 [0.78–0.94] | 0.79 [0.71–0.85] | 4.2 [2.9–6.2] | 0.15 [0.08–0.30] | 0.90 [0.87–0.92] | 28 [11–72] |
Mean difference of distance from root tip to floor of maxillary sinus (mm): original estimate: −1.88 [−2.19, −1.57], P < .0001; omitting molar alone: −1.88 [−2.19, −1.57], P < .0001; omitting high-risk bias: −1.78 [−2.32, −1.23], P < .0001; changing random to fixed model: −1.96 [−2.11, −1.81], P < 0.0001. CI indicates confidence interval; Sen, sensitivity; Spe, specificity; +LR, positive likelihood ratio; −LR, negative likelihood ratio; AUC, area under the curve; DOR, diagnostic odds ratio.
Sensitivity Analysis
Studies with a high risk of bias12,16,19,21,24 were omitted, and no significant changes were observed for the overall results (Table 6). In addition, the random-effect model was changed to a fixed-effect model for the pooling of continuous data, and no significant changes were observed for the overall MD estimates. Therefore, this study showed a good robustness (Table 6).
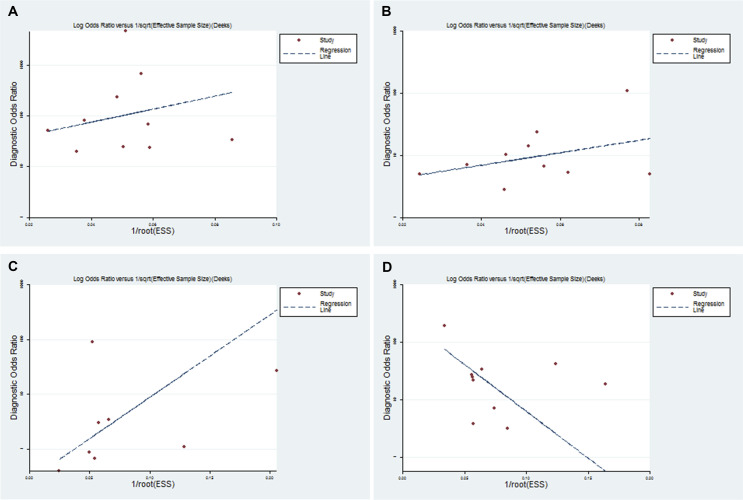
Publication Bias
Although the funnel plots for publication bias showed slight asymmetry, no statistical significance of the publication bias was observed for all types of SRR (P = .438, .136, .218, and .072 for type I, type II, type III, and type IV, respectively; Figure 6).
Figure 6.
Funnel plots of potential publication bias for (A) type I SRR, (B) type II SRR, (C) type III SRR, and (D) type IV SRR.
DISCUSSION
Complications related to the MS have long been a concern in dental clinics.1,10 Although CBCT was recommended to evaluate implant sites and MSF in implantology,28 only 49.6% of academic centers and 59.1% of private practices in America have adopted CBCT for implants preoperatively.29 Currently, clear guidance on assessing SRR in orthodontics is not available.30 The present study is the first systematic review and meta-analysis investigating the diagnostic efficacy of PR for determining the SRR. Overall, 11 studies were included and synthesized with good robustness.
The diagnostic accuracy of PR was assessed by comprehensively combining sensitivity, specificity, +LR, −LR, DOR, and AUC.31 First, it was found that, for type I SRR, PR had the highest specificity, +LR, DOR, and AUC, with a high sensitivity and a low −LR, indicating that PR had the highest diagnostic efficiency for type I SRR. Second, for type IV SRR, PR had a high DOR and AUC, with the highest sensitivity but a low +LR, the lowest –LR, and the lowest specificity, indicating a good ability to confirm true type IV SRR but a poor ability to rule out false type IV SRR. Third, PR had the lowest AUC, with a low sensitivity, +LR, and DOR and a high −LR for type II SRR, showing that the diagnostic efficiency for type II is poor. Last, PR had the lowest sensitivity, +LR, and DOR and the highest −LR for type III, indicating the lowest diagnostic efficiency for type III SRR. In addition, it was found that, for the cases diagnosed by CT/CBCT, PR tended to give a higher value of SRR for 36.19% of type II and 69.35% of type III cases. For the cases diagnosed by PR, 49.33% of type III and 75.99% of type IV cases were verified to have a lower SRR value by CT/CBCT. Furthermore, the distance from root tips to the MSF on CT/CBCT was significantly shorter (−1.88 mm) than that on PR.
The differences in diagnostic accuracy are caused by the two-dimensional characteristics of PR, which lacks cross-sectional and coronal-sectional information. CBCT showed 86.52%–97.03% and 71.56%–81.06% of the inferior MSF horizontally located between the buccal and palatal roots of the first and second molars, respectively, with the rest mainly located buccal to the buccal roots.4,5,32,33 However, on PR, this characteristic could not be observed. Because of superimposition, the buccolingual distance between the root tip and MSF (type I SRR) could be judged as type II, III, or IV SRRs. Similarly, a type III SRR is easily judged as type IV SRR on PR. Moreover, the overestimation of the degree of protrusion may also be attributed to the vertical enlargement of PR.12,22,34
The diagnosis of SRR has great implications for orthodontic control. First, when developing a treatment plan, SRR should be considered as an important factor since orthodontic tooth movement through the MS (OTMTMS) may be accompanied by uncertainty and complications of tooth tipping, root resorption, and prolonged treatment.9–11 Second, a tooth with a high value of SRR (type IV) may not be chosen as a priority to be extracted because of the high surgical risk.1 Third, if OTMTMS is to be performed, for type I and II SRR, mesiodistal OTMTMS may be safe. For type III SRR, a force system to relieve the sinus-root contact before mesiodistal movement may be suggested, whereas for type IV SRR, OTMTMS should be performed cautiously and observed carefully. Fourth, a clear quantitative assessment of SRR is important for determining the insertion position and angle of mini-implants.
The present review suggests PR is a precise technique for the diagnosis of type I SRR, but for type II, III, and IV SRR, the diagnostic accuracy is insufficient or poor, and CT/CBCT may be recommended in these situations. However, dental practitioners must adhere to the ALARA principles that every effort should be made to reduce the patient's effective radiation dose to “as low as reasonably achievable.”34 CT/CBCT should always be chosen as an adjunct to conventional radiography and should never be prescribed routinely or periodically, especially for children.34 Thus, it is suggested that the SRR be first evaluated with conventional dental radiography (PR or intraoral radiographs).28–30,34 When a type II, III, or IV SRR is displayed and OTMTMS, extraction of a tooth, or mini-screw insertion is indicated, CBCT should be used for further examination.
Although this study was conducted carefully following the PRISMA standards, there were some limitations that must be addressed. First, although high concerns regarding applicability were not found for the included studies, five of the 11 included studies showed relatively high risk of bias. Second, heterogeneity existed among the included studies. Although the statistical analyses indicated the stability of the results, some confounding factors could not be assessed quantitatively, such as the diagnostic ability and subjective factors of examiners. Third, the radiographic facilities and parameters were not all the same among studies. Fourth, there is currently no cost-effective evaluation of this topic, and thus, a comprehensive evaluation of the benefits including cost and radiation is not available. These limitations should be taken into consideration to better interpret the results of this study.
CONCLUSIONS
Currently available evidence suggests that PR could be reliable for detecting type I SRR in clinical practice.
In addition, PR has a good ability to confirm true type IV SRR but a poor ability to rule out false type IV SRR.
However, for type II and III SRR, PR shows poor accuracy and tends to overestimate the extent of protrusion of the roots into the MS.
When PRs show type II, III, or IV SRR and orthodontic tooth movement through the maxillary sinus, extraction of teeth, or mini-screw insertion is indicated, CBCT should be used for further examination.
ACKNOWLEDGMENT
This work was supported by the National Natural Science Foundation of China, Nos. 81470722 and 81201379.
REFERENCES
- 1.von Arx T, Lozanoff S. Clinical Oral Anatomy: A Comprehensive Review for Dental Practitioners and Researchers. Cham, Switzerland: Springer International Publishing; 2017. [Google Scholar]
- 2.Jang JK, Kwak SW, Ha JH, Kim HC. Anatomical relationship of maxillary posterior teeth with the sinus floor and buccal cortex. J Oral Rehabil. 2017;44:617–625. doi: 10.1111/joor.12525. [DOI] [PubMed] [Google Scholar]
- 3.Tian XM, Qian L, Xin XZ, Wei B, Gong Y. An analysis of the proximity of maxillary posterior teeth to the maxillary sinus using cone-beam computed tomography. J Endod. 2016;42:371–377. doi: 10.1016/j.joen.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 4.Estrela C, Nunes CA, Guedes OA, et al. Study of anatomical relationship between posterior teeth and maxillary sinus floor in a subpopulation of the brazilian central region using cone-beam computed tomography: part 2. Braz Dent J. 2016;27:9–15. doi: 10.1590/0103-6440201600679. [DOI] [PubMed] [Google Scholar]
- 5.Kang SH, Kim BS, Kim Y. Proximity of posterior teeth to the maxillary sinus and buccal bone thickness: a biometric assessment using cone-beam computed tomography. J Endod. 2015;41:1839–1846. doi: 10.1016/j.joen.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 6.von Arx T, Fodich I, Bornstein MM. Proximity of premolar roots to maxillary sinus: a radiographic survey using cone-beam computed tomography. J Endod. 2014;40:1541–1548. doi: 10.1016/j.joen.2014.06.022. [DOI] [PubMed] [Google Scholar]
- 7.Pagin O, Centurion BS, Rubira-Bullen IR, Alvares Capelozza AL. Maxillary sinus and posterior teeth: accessing close relationship by cone-beam computed tomographic scanning in a Brazilian population. J Endod. 2013;39:748–751. doi: 10.1016/j.joen.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Ahn NL, Park HS. Differences in distances between maxillary posterior root apices and the sinus floor according to skeletal pattern. Am J Orthod Dentofacial Orthop. 2017;152:811–819. doi: 10.1016/j.ajodo.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Motoyoshi M, Sanuki-Suzuki R, Uchida Y, Saiki A, Shimizu N. Maxillary sinus perforation by orthodontic anchor screws. J Oral Sci. 2015;57:95–100. doi: 10.2334/josnusd.57.95. [DOI] [PubMed] [Google Scholar]
- 10.Oh H, Herchold K, Hannon S, et al. Orthodontic tooth movement through the maxillary sinus in an adult with multiple missing teeth. Am J Orthod Dentofacial Orthop. 2014;146:493–505. doi: 10.1016/j.ajodo.2014.03.025. [DOI] [PubMed] [Google Scholar]
- 11.Wehrbein H, Bauer W, Wessing G, Diedrich P. The effect of the maxillary sinus floor on orthodontic tooth movement [in German] Fortschr Kieferorthop. 1990;51:345–351. doi: 10.1007/BF02167543. [DOI] [PubMed] [Google Scholar]
- 12.Sharan A, Madjar D. Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:375–381. doi: 10.1016/j.tripleo.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 13.Howe RB. First molar radicular bone near the maxillary sinus: a comparison of CBCT analysis and gross anatomic dissection for small bony measurement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:264–269. doi: 10.1016/j.tripleo.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 14.Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol. 1992;73:345–346. doi: 10.1016/0030-4220(92)90133-b. [DOI] [PubMed] [Google Scholar]
- 15.Lin CN. Agreement Between Maxillary Sinus Floor Topography and Related Root Position of Posterior Teeth Using Panoramic and Cone Beam Computed Tomography Imaging. Taiwan: Kaohsiung Medical University Institutional Repository; 2009. [Google Scholar]
- 16.Bokkasam VK, Muddepalli P, Jayam R, Devaki SB, Pakerla A, Koduri S. Comparison of panoramic radiograph with cone-beam computed tomography in assessment of maxillary sinus floor and nasal floor. J Indian Acad Oral Med Radiol. 2015;27:194–197. [Google Scholar]
- 17.Roque-Torres GD, Ramirez-Sotelo LR, De Almeida SM, Bovi Ambrosano GM, Bóscolo FN. 2D and 3D imaging of the relationship between maxillary sinus and posterior teeth. Braz J Oral Sci. 2015;14:141–148. [Google Scholar]
- 18.Dehghani Tafti M, Ghane S, NavabAzam A, Ezzodini F, Motallebi E. Investigating the correlation between panoramic and cbct of roots of posterior upper teeth with maxillary sinus floor. J Shahid Sadoughi Univ Med Sci. 2015;23:570–579. [Google Scholar]
- 19.Jung YH, Cho BH. Comparison of panoramic radiography and cone beam computed tomography for assessing the relationship between the maxillary sinus floor and maxillary molars. Korean J Oral Maxillofac Radiol. 2009;39:69–73. [Google Scholar]
- 20.Ali SM, Hawramy FA, Mahmood KA. The relation of maxillary posterior teeth roots to the maxillary sinus floor using panoramic and computed tomography imaging in a sample of Kurdish people. Tikrit J Dent Sci. 2012;1:81–88. [Google Scholar]
- 21.Fakhar HB, Kaviani H, Panjnoosh M, Shamshiri AR. Accuracy of panoramic radiographs in determining the relationship of posterior root apices and maxillary sinus floor by cone-beam CT. J Dent Med Tehran Univ Med Sci. 2014;27:108–117. [Google Scholar]
- 22.Lopes LJ, Gamba TO, Bertinato JV, Freitas DQ. Comparison of panoramic radiography and CBCT to identify maxillary posterior roots invading the maxillary sinus. Dentomaxillofac Radiol. 2016;45:20160043. doi: 10.1259/dmfr.20160043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mi XH, Liu JQ, Wu Y. Condylar morphological changes before and after orthodontic treatment for angle Class I malocclusion adult patients [in Chinese] Shanghai Kou Qiang Yi Xue. 2016;25:306–309. [PubMed] [Google Scholar]
- 24.Kalkur C, Sattur AP, Guttal KS, Naikmasur VG. Burde K. Correlation between maxillary sinus floor topography and relative root position of posterior teeth using orthopantomograph and digital volumetric tomography. Asian J Med Sci. 2017;8:26–31. [Google Scholar]
- 25.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009. 339:b2535. [PMC free article] [PubMed]
- 26.Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155:529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 27.Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol. 2005;58:882–893. doi: 10.1016/j.jclinepi.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 28.Tyndall DA, Price JB, Tetradis S, Ganz SD, Hildebolt C, Scarfe WC. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:817–826. doi: 10.1016/j.oooo.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Carter JB, Stone JD, Clark RS, Mercer JE. Applications of cone-beam computed tomography in oral and maxillofacial surgery: an overview of published indications and clinical usage in United States academic centers and oral and maxillofacial surgery practices. J Oral Maxillofac Surg. 2016;74:668–679. doi: 10.1016/j.joms.2015.10.018. [DOI] [PubMed] [Google Scholar]
- 30.American Academy of Oral and Maxillofacial Radiology. Clinical recommendations regarding use of cone beam computed tomography in orthodontics. [corrected]. Position statement by the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:238–257. doi: 10.1016/j.oooo.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 31.Cronin P, Kelly AM, Altaee D, Foerster B, Petrou M, Dwamena BA. How to perform a systematic review and meta-analysis of diagnostic imaging studies. Acad Radiol. 2018;25:573–593. doi: 10.1016/j.acra.2017.12.007. [DOI] [PubMed] [Google Scholar]
- 32.Jung YH, Cho BH. Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography. Imaging Sci Dent. 2012;42:219–224. doi: 10.5624/isd.2012.42.4.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kwak HH, Park HD, Yoon HR, Kang MK, Koh KS, Kim HJ. Topographic anatomy of the inferior wall of the maxillary sinus in Koreans. Int J Oral Maxillofac Surg. 2004;33:382–388. doi: 10.1016/j.ijom.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 34.American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902. doi: 10.14219/jada.archive.2012.0295. [DOI] [PubMed] [Google Scholar]