Abstract
In Latin America, there has been tremendous progress towards eliminating canine rabies. Major components of rabies elimination programs leading to these successes have been constant and regular surveillance for rabid dogs and uninterrupted yearly mass dog vaccination campaigns. Unfortunately, vital measures to control COVID-19 have had the negative trade-off of jeopardizing these rabies elimination and prevention activities. We aimed to assess the effect of interrupting canine rabies surveillance and mass dog vaccination campaigns on rabies trends. We built a deterministic compartment model of dog rabies dynamics to create a conceptual framework for how different disruptions may affect rabies virus transmission. We parameterized the model for conditions found in Arequipa, Peru, a city with active rabies virus transmission. We examined our results over a range of plausible values for R0 (1.36–2.0). Also, we prospectively evaluated surveillance data during the pandemic to detect temporal changes. Our model suggests that a decrease in canine vaccination coverage as well as decreased surveillance could lead to a sharp rise in canine rabies within months. These results were consistent over all plausible values of R0. Surveillance data from late 2020 and early 2021 confirms that in Arequipa, Peru, rabies cases are on an increasing trajectory. The rising rabies trends in Arequipa, if indicative to the region as whole, suggest that the achievements made in Latin America towards the elimination of dog-mediated human rabies may be in jeopardy.
Author summary
Effective strategies to control and eliminate canine rabies (and thus dog-transmitted human rabies) are uninterrupted mass dog vaccination campaigns and surveillance for rabid dogs. However, due to the COVID-19 pandemic, these vital control activities have been diminished or suspended due to restrictions implemented to decrease the spread of SARS-CoV-2 and redirection of funds. Almost a year after Peru’s response to COVID-19 began, canine rabies cases in Arequipa, a city with ongoing rabies virus transmission, are increasing rapidly. In recent months, reported canine rabies cases have surpassed previous years’ averages despite lower than average sample submissions. A mathematical model describes the mechanisms that might have created this rising trend: COVID-19-associated disruptions of mass dog vaccination campaigns and surveillance activities. As the COVID-19 pandemic is presenting obstacles to rabies elimination programs across Latin America, it is very likely that the region will face an increased canine rabies burden in the coming months to years if control efforts continue to be delayed, diminished, or suspended.
Introduction
During the last decades, enormous progress has been achieved towards the elimination of canine rabies in the Americas [1–3]. By 2019, health authorities in the Americas felt that Latin America was closer than ever to achieving the elimination of human deaths by dog-mediated rabies. The Pan American Health Organization (PAHO) announced on the eve of World Rabies Day– 28 September that only five human cases were reported in the region in the previous 12 months [2]. These achievements were due mainly to a coordinated regional plan that involved multi-pronged strategies and continuous activities conducted by national governments and local communities [3]. The COVID-19 pandemic caused by the SARS-CoV-2 coronavirus has disrupted these strategies and activities in Latin America and jeopardizes the elimination prospects in the whole region.
Among the different strategies to prevent human rabies around the world, the most effective is mass dog vaccination [1,4,5]. In most Latin American countries, the Ministries of Health, Ministries of Agriculture, or other public health agencies organize annual or biannual mass canine rabies vaccination campaigns in areas affected and unaffected by canine rabies [3]. Surveillance is also a vital component of rabies control programs [6–8]. In Latin America, since 1983, rabies control programs have included regular surveillance [3]. Importantly, rabies surveillance also activates control measures in response to the report of a suspected or confirmed rabid dog, which include broad control and prevention measures such as removal of the rabid dog, dog vaccinations, administration of post-exposure prophylaxis, and removal of exposed (bitten) dogs [9–12]. Risk of SARS-CoV-2 transmission and sequential efforts to minimize that risk have presented barriers for implementation of rabies control strategies.
SARS-CoV-2 has infected more than 46.2 million people in the Americas as of February 3, 2021, and the pandemic has required an unprecedented, coordinated effort among national public health ministries [13–15]. Public health ministries have necessarily shifted their focus and resources to implementing stay-at-home orders and ramping up emergency preparedness efforts. Moreover, in Peru, veterinarians and other authorities have considered dog vaccination a high-risk activity during the pandemic or a non-essential veterinary activity (e.g. non-urgent or non-emergency care) [16]. In the case of rabies in Peru, and other Latin American countries, the yearly mass dog vaccination campaigns, the cornerstone of rabies prevention, were postponed and downsized in 2020 [17–21]. Surveillance and focus control efforts have also been scaled back due to the COVID-19 pandemic. Here we use a deterministic compartment model to explore the long-term effects of short-term changes to the rabies prevention protocols that have been developed and maintained over the past three decades. Specifically, we investigate how a reduction in canine vaccination coverage, decreased rabies surveillance, and decreased focus control efforts can affect canine rabies dynamics in Arequipa, Peru. We report a considerable and sudden increase in the number of rabid dogs in Arequipa, consistent with model trends, after failure to implement yearly mass dog vaccination campaigns in an area with reemergent transmission of rabies virus.
Methods
Data
Data was collected from two sources. First, from 2015–2019, a door-to-door longitudinal survey was conducted in Arequipa, Peru to capture demographic data on the dog population and on vaccination campaign participation [22]. Second, collaborators at the Ministry of Health provided epidemic data on samples submitted to the Ministry of Health and subsequent focus control reports for the positive samples. Case counts and dates associated with cases were extracted from these data including: date of first clinical signs, date of death, date of sample submission, date of positive sample confirmation, and date of focus control activities.
Model description
We created a deterministic compartment model of canine rabies virus transmission in Arequipa, Peru. The model distributes the canine population between 4 population states- vaccinated (in yearly vaccination campaigns), susceptible, exposed (via the bite of a rabid dog) and infectious (Figure A in S2 Appendix). Equations depicting the movement between compartments can be expressed as:
| (1) |
| (2) |
| (3) |
| (4) |
Parameters were estimated based on population means obtained from dog population surveys conducted by our group and epidemic data provided by the Ministry of Health (Table 1). A full description of parameter estimation can be found in the supplementary information (Text A in S2 Appendix). Simulations were run for a range of plausible values of R0 (1.36–2.0). The model was fit with data collected prior to COVID-19 restrictions (Figure B in S2 Appendix), then simulations were run for 1 year from March 2020 to March 2021 and for 5 years from March 2020 to March 2025. The 1-year model simulation results were then compared with recent prospective surveillance data from that period (March 2020- March 2021) from the Ministry of Health. All computation was done using R [23].
Table 1. Model Parameters.
| Parameter | Definition | Estimate | Source |
|---|---|---|---|
| N | Total dog population (S+E+I+V) | 203183 | Arequipa Ministry of Health [24] |
| θ | Instantaneous per capita birth rate | θ = μN + α | Calculated to maintain a steady state equilibrium |
| μ | Instantaneous per capita death rate (not attributable to rabies) | 1/1099.20 | Calculated from survey data |
| γ | Instantaneous per capita rate of exposed dogs becoming infectious | 1/22.3 | Hampson, 2009 [25] |
| α | Instantaneous per capita death rate of rabid dogs attributable to rabies | 1/2.53 | Calculated from focus control data |
| ν1 | Per capita vaccination rates | Changes based on yearly vaccination coverage (Table A in S2 Appendix) | Calculated from survey data |
| ν2 | Instantaneous per capita loss of immunity rates | 1/365 | Nobivac and Peru Centro Nacional de Productos Biológicos [26,27] |
| β | Transmission coefficient | R0(γ+μ) (μ +α)/γ | Calculated based on next generation matrix methods [28] |
| R0 | Basic reproductive number | 1.44 (a range from 1.36 to 2 is presented) | Fit epidemic data |
Disruption of the rabies control program
The COVID-19 pandemic interrupted two key rabies elimination activities: mass dog vaccination and canine rabies surveillance. The disruption of each of these activities affects several parameters in the model. Many vaccination programs around the world have been affected by scarce funds already shifted towards pandemic response and fear of being infected with the COVID-19 virus [29]. Similarly, for canine rabies in Latin America, the yearly vaccination campaigns were skipped, delayed, and diminished in multiple countries in 2020 [17–21]. To examine the effects of vaccination interruption in the model we changed v1, the instantaneous per capita vaccination rate to reflect different scenarios: meeting the regional [30] and national goal of 80% coverage [11], a complete cancellation scenario of 0% coverage, and an intermediate effort of 58% coverage to match rates obtained previously (Table A in S2 Appendix) [22].
Changes in city life during quarantine may also have impacted rabid dogs’ survival in several ways. First, fewer people left home; in Arequipa, many rabid dogs (25%) are reported by unrelated city dwellers as opposed to dog owners [31]. Fewer people out in public compounded with increased difficulty in travel to and from health posts and disrupted health post hours led to reports of suspected rabid dogs decreasing to almost zero. Second, even if rabid dogs were reported, COVID-19 protocols disrupted rabies response teams, delaying euthanization and removal of suspected rabid dogs. Third, a decrease in vehicle traffic during the COVID-19 lockdown led to increased survival time of disoriented dogs that otherwise would have been hit by cars. Hampson et al. found that rabid dogs died of the disease in an average of 3.7 days if they were not killed [25]. Therefore, to examine the effect of increased survival time of rabid dogs due to COVID we shifted the death rate (α) from reflecting a mean survival time of 2.5 days (calculated from focus control reports) to 3.7 days (the expected survival time without focus control).
Results
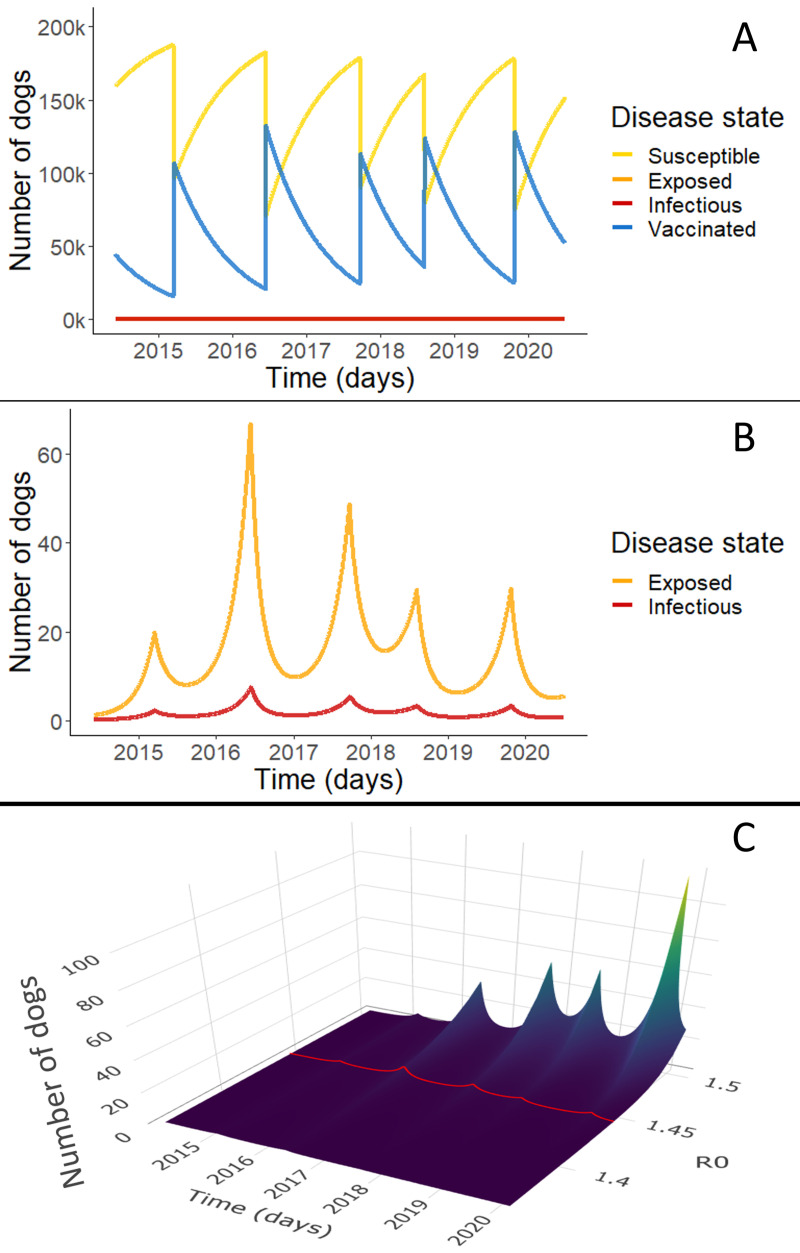
There were 214 reports of rabid dogs in the department of Arequipa from March 2015 to March 2020 out of 2,650 samples submitted over the period (Figure B and Figure C in S2 Appendix), on average a little less than one (0.93) per week. Our model has reasonable matching to the reported case data assuming a reporting rate of 10% and an R0 of 1.44 (Figure B in S2 Appendix). The full dynamics (without any scaling for underreporting) can be seen in Fig 1, clearly showing the cyclic nature of immunity and transmission caused by the yearly vaccination campaigns. Population immunity provided by the yearly vaccination campaign decays quickly due to high rates of population turnover (controlled by parameters μ and θ) and loss of vaccine-provided immunity (ν2) (Fig 1A). The proportion of the population affected by rabies virus transmission is so small that it is not apparent when shown together with the susceptible and vaccinated population (Fig 1A). However, the isolated exposed and infectious population dynamics follow a cyclic pattern (Fig 1B) caused by the pulses of immunity and subsequent decay: waves of exposed and infected dogs rise as population immunity falls. We also examined this behavior over a select range of possible values of R0 (Fig 1C) and though the amplitude of peaks may change, the rising trends remain the same. The trends are consistent for the full range of possible values of R0 from 1.36–2.0 (Figure D in S2 Appendix).
Fig 1. Rabies compartmental model results.
Simulations depict daily point prevalence of each disease state (S,E,I,V). Panel A shows the dynamics of all disease states in the best fit rabies model for Arequipa, Peru. The blue line shows the vaccinated dog population numbers over time and the yellow line shows the susceptible population dynamics. Because the proportion of rabies exposed (pink line) and infected dogs (red line) is so small, these dynamics are not apparent in Panel A. Panel B highlights these exposed and infectious dynamics with an adjusted scale. Panel C shows infected population dynamics for a range of R0 from 1.36–1.5. In other words, it represents the red line of infected population dynamics shown in B but for a range of R0. The trends extend for the full range of possible values of R0 [1.36, 2.0] which can be seen in the supplementary information (Figure D in S2 Appendix).
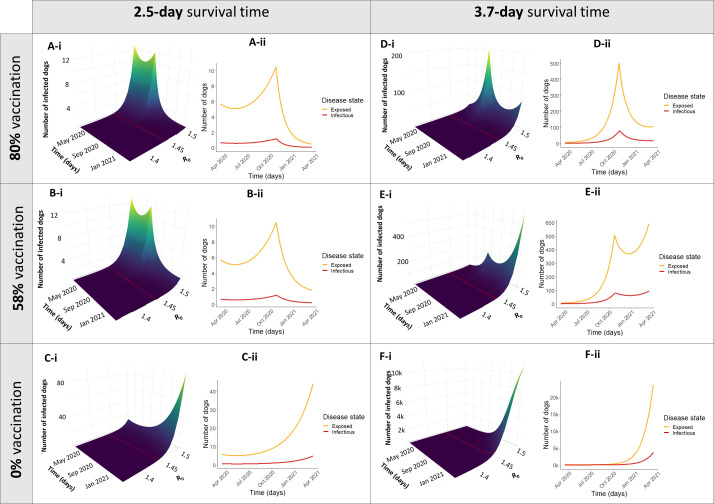
The effects of the disruption of mass vaccination and surveillance are displayed both as a surface plot with the full range of possible values of R0, and as a 2D line plot with R0 = 1.44, representing our best estimate for Arequipa, Peru (Fig 2). With zero dogs vaccinated in the city (due to a cancelled vaccination campaign), cases begin to grow exponentially (Fig 2C and 2F). In the ideal case that vaccine coverage reached the 80% recommended by PAHO, the numbers of infected dogs were suppressed to nearly 0 (Fig 2A and 2D). However, even intermediate coverage of 58% has a significant impact on suppressing the rise in infected numbers (Fig 2B and 2E) compared to no vaccination coverage at all (Fig 2C and 2F). The effect of decreased surveillance and subsequent focus control is postulated to result in increased rabid dog survival time from 2.5 to 3.7 days as seen in Fig 2D, 2E and 2F though incidence increases, the number of infected dogs can still be dampened by mass vaccination. The worst-case scenario, where all control activities, mass dog vaccination, surveillance, and focus control, cease, results in a marked exponential rise in rabies cases within a few months (Fig 2E).
Fig 2. Different simulations of disruption scenarios for 1 year.
Simulations depict daily point prevalence of each disease state (S,E,I,V). Simulations were run for 1 year after the beginning of COVID-19 control measures in Arequipa, Peru (March 16, 2020- March 16, 2021). Panels A-C depict different vaccination scenarios with normal levels of surveillance and control measures leading to an average survival time (ST) of rabid dogs to be 2.5 days. Panels D-F show the same vaccination scenarios with decreased surveillance leading to an increased survival time of rabid dogs to 3.7 days. The vaccination scenarios depicted correspond to yearly vaccination campaigns reaching the optimal goal of 80% coverage (Panels A, D), a sub-optimal level of 58% coverage (Panels B, E), and a complete cancellation of the vaccination campaign where coverage is 0% (Panels C, F). Both the surface plots with a range of values of R0 (i) and a transect where R0 = 1.44 (ii) are displayed).
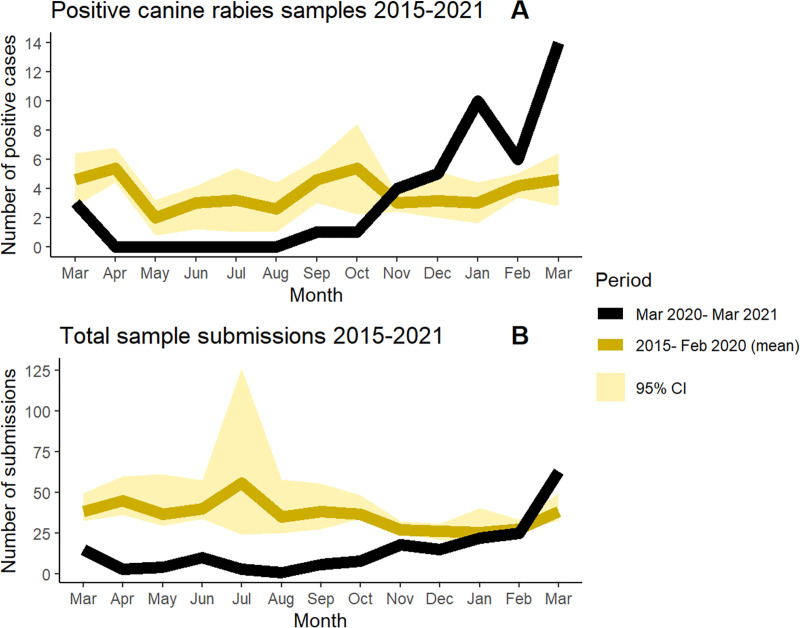
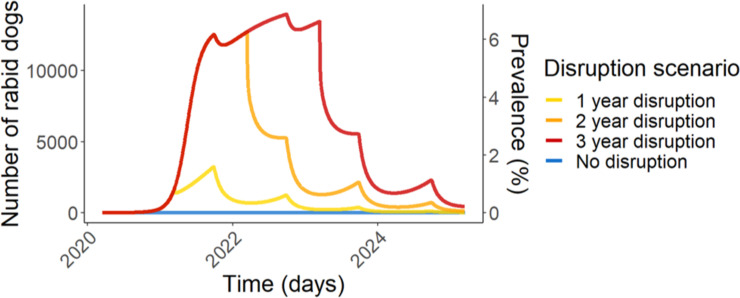
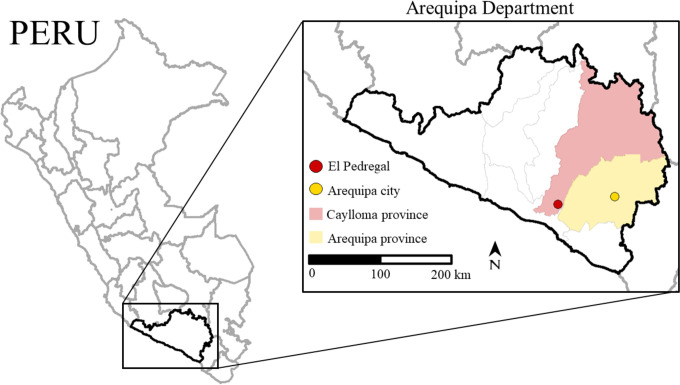
In Arequipa, the 2020 vaccination campaign was severely reduced, reaching a city-wide coverage of only 12.3%. Surveillance, measured by number of samples submitted to the ministry of health was also severely reduced in 2020 compared to previous years averages (Fig 3). Under these conditions model trends predict an exponential rise in rabies cases within months, a prediction that has been unfortunately corroborated through preliminary surveillance results from December 2020 through March 2021. From November 2020 to February 2021 higher than average numbers of cases were detected despite continued reduced surveillance effort and only a small number of sample submissions compared to previous years (Fig 3). March 2021 had the largest number of canine rabies cases detected (14 cases) since the virus was re-introduced in 2015. Intermediate-term effects (5 years) were simulated in Fig 4, showing continued dramatically increased simulated rabies burden due to COVID-19 disruptions. Moreover, the rabies affected area has extended. From 2015 to January 2021, dog rabies cases were contained within the city of Arequipa, province of Arequipa (Fig 5). Since February 2021, rabies has expanded within the department of Arequipa to a neighboring province; at least 7 rabid dogs have been detected in the province of Caylloma (Fig 5).
Fig 3. Canine rabies diagnostic samples submitted from 2015–2021.
Averages for monthly canine rabies case counts (monthly cumulative incidence) confirmed by laboratory diagnosis (Panel A) and for total canine diagnostic sample submissions to the Peru Ministry of Health for Arequipa Department (Panel B) were calculated by aggregating monthly data from March 2015 (when rabies was first reported in Arequipa city) to February 2020 (the last month that Peru was operating under non-COVID conditions) and compared to pandemic time surveillance data (March 2020 to March 2021). 95% confidence intervals were computed via bootstrap methods by resampling 2000 times. A full timeline is available in the supplementary information (Figure C in S2 Appendix).
Fig 4. Disruption scenario simulations for 5 years.
Rabies dynamics in Arequipa were simulated for five years under four different scenarios. The “No disruption” scenario depicts a counterfactual no-covid scenario where vaccination campaigns were conducted at pre-pandemic normal (58% coverage) and average surveillance remained normal (average survival time of rabid dogs = 2.5 days) throughout the simulated time period (March 2020-March 2025). The disruption scenarios simulate 1–3 years of COVID-19 disruptions with vaccination coverage reduced to 12.3% and average survival time of rabid dogs increased to (3.7 days) before returning to pre-pandemic normal.
Fig 5. Map of Arequipa Department.
Arequipa Department consists of 8 provinces. Prior to February 2021, rabies cases were contained in Arequipa province (the province containing Arequipa city). In February 2021, cases spread to the neighboring province of Caylloma, primarily in the city of El Pedregal. Seven cases have since been detected in El Pedregal. Shapefiles used to create maps are from Peru’s National Geo-referenced Data Platform Geo Peru [32].
Discussion
Our model results predicted that disruptions to rabies control programs caused by the COVID-19 pandemic would substantially increase the number of cases of canine rabies with an associated increased risk of human rabies within a few months. Preliminary surveillance trends from Arequipa, Peru suggest that an increased rise in canine rabies cases is already occurring. This crisis has the potential to reverse strides towards the regional goal of zero canine-mediated human deaths of rabies by 2030 [33]. Given that COVID-19 will continue to challenge public health departments in the short- and medium-term as public health officials work to immunize populations worldwide, it is essential to create a strategy for rabies surveillance and prevention during the COVID-19 pandemic. This strategy should consider new approaches to dog vaccination that can accommodate social distancing and other COVID-19 prevention measures. New dog vaccination approaches, even with suboptimal coverage, could reduce canine rabies cases in the short term and prevent dog-mediated human rabies.
Our analysis and the sharp rise in canine rabies cases in Peru have broad implications regionally for Latin America. Our model of canine rabies in Arequipa demonstrates the effects of COVID-19 on the spread of canine rabies in a city with a medium to large human population (about 1 million), active immigration and emigration, continuous but suboptimal efforts to control rabies, and a fairly large free-roaming dog population [22,31,34]; many of these characteristics are shared with other Latin American urban areas. Also, Arequipa represents an area of rabies reintroduction and rabies re-establishment [34], both undesired and rare events. Modeling a city with these characteristics and continuous rabies virus transmission may provide insight into rabies-endemic Latin American cities during the COVID-19 pandemic and also into the risk of expansion to non-endemic neighboring cities.
In rabies-affected areas in Latin America, the COVID-19 pandemic has disrupted the multi-pronged rabies control program at several points, the full effects of which may not become apparent for several years. The first prong of rabies control programs that may be affected by COVID-19 is the rabies surveillance system. Because rabies surveillance systems rely heavily on submission of samples from dogs reported to exhibit clinical signs of rabies by the public, the absence of people leaving home to observe these dogs has caused greatly decreased reporting rates. In Arequipa, from April 2020 to September 2020, an average of 4.7 samples were submitted per month, compared to an average of 35.7 previously. We postulate that dogs may live longer and transmit rabies virus to a larger number of dogs before they die, as reflected by a decreased parameter α, the death rate due to rabies.
The second prong of rabies control in Arequipa is yearly vaccination campaigns. Due to COVID-19, the yearly dog vaccination campaign in Arequipa in 2020 was severely reduced to a coverage rate of 12.3%, and similar disruptions occurred across Latin America [17–21]. COVID-19 poses challenges to rabies vaccination campaigns in a few ways. First, geographic areas with high rates of canine rabies in particular need of vaccination points also tend to be areas with high rates of COVID-19 due to population density, which leads to concern for the safety of healthcare personnel and dog owners. Second, public health organizations are focusing their energy and resources on the COVID-19 crisis at hand. Diverting scarce public health resources towards a crisis is often necessary for some amount of time; however, our model suggests that reducing or postponing vaccination campaigns could have detrimental consequences on the spread of dog rabies and, ultimately, public health. The 2020 vaccination campaign in Arequipa covered only 4 districts out of 14 in the city; patchy, heterogeneous coverage likely further exasperates case surges seen from low vaccination rates [7,22,35–37]. Our results correspond with other studies around the world of the detrimental effects of disrupting rabies mass vaccination campaigns. A modeling study in Chad found that vaccination campaigns needed to be repeated due to imported cases [38], another modeling study in Bali, Indonesia, simulated a rise in cases after control activities were halted [36], and such a rise in rabies cases were observed in South Africa after vaccination campaigns were halted [39]. Even if the recommended 80% vaccination coverage goals may be unattainable, our model indicates that an intermediate (suboptimal) effort can still have a tremendous effect in curbing the rise of canine rabies.
The model presented above has many sources of uncertainty, perhaps the most significant is a likely massive underreporting of canine rabies cases leading to lack of accurate data and bias in parameterized data around which the model is constructed. Inadequate surveillance can exacerbate underreporting—a common problem in rabies- affected areas [3,8,34,40–42]—and lead to more cases as the virus spreads undetected. Additionally, we made several assumptions about the model parameters, that: 1) in Arequipa, 10% of canine rabies cases are detected, 2) the majority of dog bites transmitting rabies virus occur after the onset of rabies clinical signs in the biting (rabid) dog, and 3) vaccination immunity decay follows the conservative licensure estimate though the true decay rate of immunity may be slower. The COVID-19 pandemic likely has caused many changes in both human and dog behavior not captured in our model, such as varied movement and behavior patterns of humans leading to varied scavenging patterns and contact networks by dogs. Finally, our models are not intended for use in predicting exact values on specific dates but rather as tools to assess trends resulting from different control strategies.
The effects of stopping or pausing rabies prevention activities have had serious effects on cases of canine rabies, and consequently, on the risk of human rabies. This problem is not unique to rabies in Latin America; worldwide, COVID-19 is disrupting control efforts in a plethora of infectious disease programs. Already reported in the literature are flagging efforts to control measles and Hepatitis B Virus, decreased surveillance jeopardizing poliovirus eradication goals, and predicted surges in malaria and Dengue fever cases following pandemic neglect [29,43–47]. Animal disease control programs including African Swine Fever and tuberculosis surveillance systems are also at risk [48]. Parallels can be drawn to other public health crises such as Ebola, where protocols to contain Ebola interrupted screening and diagnosis of malaria, tuberculosis, and HIV [49,50]. Adequate surveillance, especially animal disease surveillance, is one essential piece of infectious disease control programs that is often neglected for more immediate emergencies [51–53]. COVID-19 has had a devastating toll on health through serious to fatal cases and economic hardships. However, the true extent of the damage caused by the pandemic may not be observed for years to decades as previously under-control diseases surge due to neglected control programs.
Supporting information
(DOCX)
(DOCX)
Acknowledgments
We gratefully acknowledge the contributions of and the work done by the Gerencia Regional de Salud de Arequipa, the Red de Salud Arequipa Caylloma, the Laboratorio Referencial Regional Arequipa, and the Centro de Salud de Alto Selva Alegre. We acknowledge the work of the members of the Zoonotic Disease Research Laboratory, One Health Unit, and their contribution collecting part of the data used in this study.
Data Availability
Code used to create the model is publicly available at https://github.com/bhraynor/Rabies_CovidDisruption_Model. All the parameters and parameter methods necessary to replicate our results are shared in both manuscript and code. Surveillance data are available at the Peruvian Ministry of Health upon request and should be requested directly from the local Health Office in Arequipa (amesadepartes@saludarequipa.gob.pe).
Funding Statement
This project was supported by NIH-NIAID grant 1K01AI139284 (RCN) and by NIH-NIAID grant 1R01AI146129-01 (MZL). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Franka R, Smith TG, Dyer JL, Wu X, Niezgoda M, Rupprecht CE. Current and future tools for global canine rabies elimination. Antiviral Res. 2013;100:220–225. doi: 10.1016/j.antiviral.2013.07.004 [DOI] [PubMed] [Google Scholar]
- 2.Reyes O. PAHO/WHO | World Rabies Day: Latin America and the Caribbean on the cusp of eliminating rabies deaths. In: Pan American Health Organization / World Health Organization; [Internet]. 25 Sep 2019. [cited 18 Jun 2020]. Available from: https://www.paho.org/hq/index.php?option=com_content&view=article&id=15452:world-rabies-day-latin-america-and-the-caribbean-on-the-cusp-of-eliminating-rabies-deaths&Itemid=1926&lang=en. [Google Scholar]
- 3.Vigilato MAN, Clavijo A, Knobl T, Silva HMT, Cosivi O, Schneider MC, et al. Progress towards eliminating canine rabies: policies and perspectives from Latin America and the Caribbean. Philos Trans R Soc B Biol Sci. 2013;368. doi: 10.1098/rstb.2012.0143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lavan RP, King AIM, Sutton DJ, Tunceli K. Rationale and support for a One Health program for canine vaccination as the most cost-effective means of controlling zoonotic rabies in endemic settings. Vaccine. 2017;35:1668–1674. doi: 10.1016/j.vaccine.2017.02.014 [DOI] [PubMed] [Google Scholar]
- 5.Zinsstag J, Dürr S, Penny MA, Mindekem R, Roth F, Menendez Gonzalez S, et al. [Transmission dynamics and cost-effectiveness of rabies control in dogs and humans in an African city]. Med Trop Rev Corps Sante Colon. 2011;71:596–604. [PubMed] [Google Scholar]
- 6.Broban A, Tejiokem MC, Tiembré I, Druelles S, L’Azou M. Bolstering human rabies surveillance in Africa is crucial to eliminating canine-mediated rabies. PLoS Negl Trop Dis. 2018;12:e0006367. doi: 10.1371/journal.pntd.0006367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Townsend SE, Lembo T, Cleaveland S, Meslin FX, Miranda ME, Putra AAG, et al. Surveillance guidelines for disease elimination: A case study of canine rabies. Comp Immunol Microbiol Infect Dis. 2013;36:249–261. doi: 10.1016/j.cimid.2012.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. WHO Expert Consultation on Rabies: second report. World Health Organization; 2013. Available from: https://apps.who.int/iris/handle/10665/85346. [PubMed] [Google Scholar]
- 9.Departamento de epidemiologia. Protocolos de Vigilancia Epidemiológica Enfermedades Zoonóticas. Gobierno de la república de Guatemala; 2018. Available from: http://epidemiologia.mspas.gob.gt/files/Publicaciones%202018/Protocolos/Protocolos%20de%20Vigilancia%20Epidemiol%C3%B3gica%20Enfermedades%20Zoon%C3%B3ticas.pdf. [Google Scholar]
- 10.PAHO. Manual de rabia—Página inicial. [cited 11 Jul 2020]. Available from: https://www.paho.org/arg/publicaciones/publicaciones%20virtuales/cdmanualRabia/index.html.
- 11.Perú Ministerio de Salud. Norma técnica de salud para la prevención y control de rabia humana en el Perú. Perú Ministerio de Salud; 2017. Available from: http://bvs.minsa.gob.pe/local/MINSA/4193.pdf. [Google Scholar]
- 12.Servicio departamental de salud. Programa de control y vigilancia de zoonosis. Gobierno autonómo del departametno de La Paz; Available from: https://www.sedeslapaz.gob.bo/sites/default/files/PROGRAMA%20DE%20CONTROL%20Y%20VIGILANCIA%20DE%20ZOONOSIS.pdf. [Google Scholar]
- 13.PAHO. Coronavirus Disease (COVID-19) pandemic—PAHO/WHO | Pan American Health Organization. [cited 22 Jun 2020]. Available from: http://www.paho.org/en/topics/coronavirus-infections/coronavirus-disease-covid-19-pandemic. [Google Scholar]
- 14.Latin America: COVID-19 cases by country. In: Statista [Internet]. [cited 13 Jul 2020]. Available from: https://www-statista-com.proxy.library.upenn.edu/statistics/1101643/latin-america-caribbean-coronavirus-cases/.
- 15.WHO. WHO Director-General’s opening remarks at the media briefing on COVID-19–11 March 2020. [cited 22 Jun 2020]. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020.
- 16.DPCEMZ-Zoonosis. Nota informativa no. 0029-2020-DPCEM-DGIESP/MINSA. MINSA; Available from: www.minsa.gob.pe. [Google Scholar]
- 17.Quinchía AZ. Así será la segunda jornada de vacunación contra la rabia para perros y gatos en Antioquia. In: www.elcolombiano.com [Internet]. 6 Nov 2020 [cited 6 Feb 2021]. Available from: https://www.elcolombiano.com/antioquia/medellin/jornada-de-vacunacion-para-perros-y-gatos-en-antioquia-JE14013802.
- 18.Ribeiro T. Campanha de Vacinação contra a raiva é adiada em SP por conta da Covid-19. In: Agora São Paulo; [Internet]. 5 Aug 2020. [cited 6 Feb 2021]. Available from: https://agora.folha.uol.com.br/sao-paulo/2020/08/campanha-de-vacinacao-contra-a-raiva-e-adiada-em-sp-por-conta-da-covid-19.shtml. [Google Scholar]
- 19.Pospuesta la jornada de vacunación antirrábica. Milenio. 29 Mar 2020. Available from: https://www.milenio.com/ciencia-y-salud/pospuesta-la-jornada-de-vacunacion-antirrabica. Accessed 6 Feb 2021.
- 20.Municipalidad del Partido de Olavarría. Se suspende la Campaña de Vacunación Antirrábica. [cited 12 Apr 2021]. Available from: https://www.olavarria.gov.ar/se-suspende-la-campana-de-vacunacion-antirrabica/.
- 21.Gobierno de La Habana cancela campaña gratuita de vacunación antirrábica promovida por animalistas. In: CiberCuba [Internet]. 18 Jun 2020 [cited 12 Apr 2021]. Available from: https://www.cibercuba.com/noticias/2020-06-18-u1-e199291-s27061-gobierno-habana-cancela-campana-gratuita-vacunacion.
- 22.Castillo-Neyra R, Toledo AM, Arevalo-Nieto C, MacDonald H, Puente-León MD la, Naquira-Velarde C, et al. Socio-spatial heterogeneity in participation in mass dog rabies vaccination campaigns, Arequipa, Peru. PLoS Negl Trop Dis. 2019;13:e0007600. doi: 10.1371/journal.pntd.0007600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.R core team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; 2018. Available from: https://www.R-project.org/. [Google Scholar]
- 24.Red Arequipa Caylloma. Plan de accion de la campaña de vacunacion antirabica canina 2019. 2019. Available from: https://redperifericaaqp.gob.pe/wp-content/uploads/2019/04/accion-de-la-campana-atirabica-2019-comprimido.pdf.
- 25.Hampson K, Dushoff J, Cleaveland S, Haydon DT, Kaare M, Packer C, et al. Transmission Dynamics and Prospects for the Elimination of Canine Rabies. PLOS Biol. 2009;7:e1000053. doi: 10.1371/journal.pbio.1000053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MSD. Nobivac Rabies. In: MSD Salud Animal Argentina [Internet]. [cited 4 Feb 2021]. Available from: https://www.msd-salud-animal.com.ar/productos/nobivac-rabies/.
- 27.Instituto Nacional de Salud. Productos. In: Productos [Internet]. [cited 4 Feb 2021]. Available from: http://web.ins.gob.pe/es/productos-biologicos/productos.
- 28.Diekmann O, Heesterbeek JAP, Roberts MG. The construction of next-generation matrices for compartmental epidemic models. J R Soc Interface. 2010;7:873–885. doi: 10.1098/rsif.2009.0386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.WHO. At least 80 million children under one at risk of diseases such as diphtheria, measles and polio as COVID-19 disrupts routine vaccination efforts, warn Gavi, WHO and UNICEF. [cited 11 Jul 2020]. Available from: https://www.who.int/news-room/detail/22-05-2020-at-least-80-million-children-under-one-at-risk-of-diseases-such-as-diphtheria-measles-and-polio-as-covid-19-disrupts-routine-vaccination-efforts-warn-gavi-who-and-unicef.
- 30.Schneider MC, Belotto A, Adé MP, Hendrickx S, Leanes LF, Rodrigues MJ de F, et al. Current status of human rabies transmitted by dogs in Latin America. Cad Saúde Pública. 2007;23:2049–2063. doi: 10.1590/s0102-311x2007000900013 [DOI] [PubMed] [Google Scholar]
- 31.Castillo-Neyra R, Zegarra E, Monroy Y, Bernedo RF, Cornejo-Rosello I, Paz-Soldan VA, et al. Spatial Association of Canine Rabies Outbreak and Ecological Urban Corridors, Arequipa, Peru. Trop Med Infect Dis. 2017;2. doi: 10.3390/tropicalmed2030038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.GEO PERÚ. Plataforma Digital Georreferenciada del Estado peruano. In: Mapa Interactivo; [Internet]. [cited 7 May 2021]. Available from: https://www.geoperu.gob.pe. [Google Scholar]
- 33.WHO, FAO, OIE. Zero by 30: the global strategic plan to end human deaths from dog-mediated rabies by 2030. Geneva: WHO, FAO, OIE; 2018. Available from: http://www.who.int/rabies/resources/9789241513838/en/. [Google Scholar]
- 34.Castillo-Neyra R, Brown J, Borrini K, Arevalo C, Levy MZ, Buttenheim A, et al. Barriers to dog rabies vaccination during an urban rabies outbreak: Qualitative findings from Arequipa, Peru. PLoS Negl Trop Dis. 2017;11:e0005460. doi: 10.1371/journal.pntd.0005460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cleaveland S, Kaare M, Tiringa P, Mlengeya T, Barrat J. A dog rabies vaccination campaign in rural Africa: impact on the incidence of dog rabies and human dog-bite injuries. Vaccine. 2003;21:1965–1973. doi: 10.1016/s0264-410x(02)00778-8 [DOI] [PubMed] [Google Scholar]
- 36.Townsend SE, Sumantra IP, Pudjiatmoko, Bagus GN, Brum E, Cleaveland S, et al. Designing Programs for Eliminating Canine Rabies from Islands: Bali, Indonesia as a Case Study. PLoS Negl Trop Dis. 2013;7:e2372. doi: 10.1371/journal.pntd.0002372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferguson EA, Hampson K, Cleaveland S, Consunji R, Deray R, Friar J, et al. Heterogeneity in the spread and control of infectious disease: consequences for the elimination of canine rabies. Sci Rep. 2015;5:18232. doi: 10.1038/srep18232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Laager M, Léchenne M, Naissengar K, Mindekem R, Oussiguere A, Zinsstag J, et al. A metapopulation model of dog rabies transmission in N’Djamena, Chad. J Theor Biol. 2019;462:408–417. doi: 10.1016/j.jtbi.2018.11.027 [DOI] [PubMed] [Google Scholar]
- 39.Weyer J, Dermaux-Msimang V, Grobbelaar A, Roux C le, Moolla N, Paweska J, et al. Epidemiology of human rabies in South Africa, 2008–2018. S Afr Med J. 2020;110:877–881. doi: 10.7196/SAMJ.2020.v110i9.14324 [DOI] [PubMed] [Google Scholar]
- 40.Benavides JA, Megid J, Campos A, Rocha S, Vigilato MAN, Hampson K. An evaluation of Brazil’s surveillance and prophylaxis of canine rabies between 2008 and 2017. PLoS Negl Trop Dis. 2019;13:e0007564. doi: 10.1371/journal.pntd.0007564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carvalho MF de, Vigilato MAN, Pompei JA, Rocha F, Vokaty A, Molina-Flores, et al. Rabies in the Americas:1998–2014. PLoS Negl Trop Dis. 2018;12:e0006271. doi: 10.1371/journal.pntd.0006271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Widdowson M-A, Morales GJ, Chaves S, McGrane J. Epidemiology of Urban Canine Rabies, Santa Cruz, Bolivia, 1972–1997. Emerg Infect Dis. 2002;8:458–461. doi: 10.3201/eid0805.010302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pley CM, McNaughton AL, Matthews PC, Lourenço J. The global impact of the COVID-19 pandemic on the prevention, diagnosis and treatment of hepatitis B virus (HBV) infection. BMJ Glob Health. 2021;6:e004275. doi: 10.1136/bmjgh-2020-004275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sherrard-Smith E, Hogan AB, Hamlet A, Watson OJ, Whittaker C, Winskill P, et al. The potential public health consequences of COVID-19 on malaria in Africa. Nat Med. 2020;26:1411–1416. doi: 10.1038/s41591-020-1025-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zomahoun DJ. Impact of COVID-19 Pandemic on Global Poliovirus Surveillance. MMWR Morb Mortal Wkly Rep. 2021;69. doi: 10.15585/mmwr.mm695152a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Olive M-M, Baldet T, Devillers J, Fite J, Paty M-C, Paupy C, et al. The COVID-19 pandemic should not jeopardize dengue control. PLoS Negl Trop Dis. 2020;14:e0008716. doi: 10.1371/journal.pntd.0008716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Santoli JM. Effects of the COVID-19 Pandemic on Routine Pediatric Vaccine Ordering and Administration—United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69. doi: 10.15585/mmwr.mm6919e2 [DOI] [PubMed] [Google Scholar]
- 48.Gortázar C, de la Fuente J. COVID-19 is likely to impact animal health. Prev Vet Med. 2020;180:105030. doi: 10.1016/j.prevetmed.2020.105030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leuenberger D, Hebelamou J, Strahm S, De Rekeneire N, Balestre E, Wandeler G, et al. Impact of the Ebola Epidemic on General and HIV Care in Macenta, Forest Guinea, 2014. AIDS Lond Engl. 2015;29:1883–1887. doi: 10.1097/QAD.0000000000000784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parpia AS, Ndeffo-Mbah ML, Wenzel NS, Galvani AP. Effects of Response to 2014–2015 Ebola Outbreak on Deaths from Malaria, HIV/AIDS, and Tuberculosis, West Africa—Volume 22, Number 3—March 2016. —Emerging Infectious Diseases journal—CDC. [cited 14 Jul 2020]. doi: 10.3201/eid2203.150977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Research Council (US) Committee on Achieving Sustainable Global Capacity for Surveillance and Response to Emerging Diseases of Zoonotic Origin, Keusch GT, Pappaioanou M, Gonzalez MC, Scott KA, Tsai P. Sustainable Financing for Global Disease Surveillance and Response. Sustaining Global Surveillance and Response to Emerging Zoonotic Diseases. National Academies Press; (US: ); 2009. Available from: http://www.ncbi.nlm.nih.gov/books/NBK215328/. [PubMed] [Google Scholar]
- 52.International Working Group on Financing Preparedness. From Panic and Neglect to Investing in Health Security: Financing Pandemic Preparedness at a National Level. International Working Group on Financing Preparedness; 2017. Dec. Available from: http://pubdocs.worldbank.org/en/890291523304595565/FINAL-IWG-Report-3-5-18.pdf. [Google Scholar]
- 53.Nicolay N, Mirinaviciute G, Mollet T, Celentano LP, Bacci S. Epidemiology of measles during the COVID-19 pandemic, a description of the surveillance data, 29 EU/EEA countries and the United Kingdom, January to May 2020. Eurosurveillance. 2020;25:2001390. doi: 10.2807/1560-7917.ES.2020.25.31.2001390 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
Code used to create the model is publicly available at https://github.com/bhraynor/Rabies_CovidDisruption_Model. All the parameters and parameter methods necessary to replicate our results are shared in both manuscript and code. Surveillance data are available at the Peruvian Ministry of Health upon request and should be requested directly from the local Health Office in Arequipa (amesadepartes@saludarequipa.gob.pe).