Abstract
This article outlines a multidisciplinary approach to implementing a telehealth program in the acute care hospital setting during the coronavirus disease 2019 (COVID-19) pandemic. Telehealth has been used in many practice areas, although it can be a particular challenge to establish in an acute care hospital given the fast-paced environment. However, the COVID-19 pandemic presented a unique situation. In-person treatment interactions became increasingly high risk for both patient and provider, and there was an emerging need to conserve personal protective equipment and limit exposure. In response to these developments, physical therapists, occupational therapists, and speech language pathologists treating an adult population turned to telehealth to supplement in-person treatment. This article outlines the clinical reasoning and practical application to implementing a telehealth program in an acute care hospital and includes regulations, identified successful strategies, barriers, considerations, decision-making algorithms, and discipline-specific interventions.
Keywords: COVID-19, Rehabilitation, Telemedicine
List of abbreviations: AM-PAC, Activity Measure for Post-Acute Care; AOTA, American Occupational Therapy Association; APTA, American Physical Therapy Association; ASHA, American Speech-Language-Hearing Association; COVID-19, coronavirus disease 2019; EMR, electronic medical record; JH-HLM, Johns Hopkins Highest Level of Mobility; OT, occupational therapist; PT, physical therapist; SLP, speech language pathologist
Graphical Abstract

As the coronavirus disease 2019 (COVID-19) pandemic progressed, Johns Hopkins Physical Medicine and Rehabilitation therapy services including speech language pathology, occupational therapy, and physical therapy rapidly altered an established delivery of care model to meet patient needs while maintaining safe and evolving infection control practices. As typical delivery of care became higher risk for both provider and patient, therapists needed alternative means of treatment and turned to telehealth services to meet this need. A core team of therapists onsite completed telehealth sessions using the following outlined strategies and interventions.
Regulations
National organizations
The American Physical Therapy Association (APTA), American Occupational Therapy Association (AOTA), and American-Speech-Language-Hearing Association (ASHA) define telehealth as the use of communication technology to deliver therapy services including assessment, intervention, prevention, and/or consultation. AOTA, APTA, and ASHA acknowledge the need for clinical judgment when determining the appropriateness of telehealth utilization while also requiring that the quality of service is congruent with that which is provided in person. The national organizations deem telehealth as an appropriate model of service delivery when provided in a manner consistent with the association positions, standards, guidelines, policies, and procedures with strict adherence to the code of ethics.1, 2, 3, 4
Centers for Medicare and Medicaid Services federal policy and regulation
Before the pandemic, physical therapists (PTs), occupational therapists (OTs), and speech language pathologists (SLPs) were not eligible telehealth providers through Medicare. This posed the ultimate barrier to widespread telehealth implementation in the rehabilitation profession. Eligible providers of telehealth also had site-specific stipulations that sometimes required the patient be in a rural or underserved area, the patient be in a clinical setting while services are provided, and the services be provided in real time.5 On April 30, 2020, the Centers for Medicare and Medicaid Services announced the addition of PTs, OTs, and SLPs to their list of eligible telehealth providers who could bill for telehealth services through the duration of the COVID-19 emergency declaration. This temporary regulatory change was retroactive to March 1, 2020.6
Protocol development
Based on regulations, a need for alternative treatment delivery for the population with COVID-19, and to streamline decision making, a multidisciplinary telehealth team of PTs, OTs, and SLPs developed algorithms using discipline-specific considerations.The algorithms were used to guide clinical reasoning when identifying patients appropriate for telehealth therapy sessions. Algorithms were created during initial telehealth meetings and modified as the telehealth outreach progressed. Therapists completed chart reviews, retrieving the following information from the electronic medical record (EMR) to determine telehealth eligibility.
Multidisciplinary considerations
Patient independence
The ideal candidate would have the ability to sit upright within the field of the camera, adjust the camera angle, and follow commands. The therapists screening for telehealth appropriateness used a standardized outcome measure, the Activity Measure for Post-Acute Care (AM-PAC), to assess for independence and capability. The AM-PAC measures 2 functional domains: basic mobility and daily activities.7 Each domain has 6 questions in which patients are scored on the level of assistance they require for each task, based on observation and clinical judgment.7 The AM-PAC is completed daily by nursing staff so that the score represents the patient's current level of function. For example, a documented AM-PAC score of 24 would indicate total independence, whereas an AM-PAC score of 6 would indicate total dependence in the basic mobility and daily activities observed.
Physical and sensory characteristics
Patients were screened via chart review or during initial evaluation to determine limitations in hearing ability, visual ability, manual dexterity (ie, ability to hold and manipulate the tablet), and physical endurance (ie, self-positioning, sitting tolerance).
Cognitive and behavioral considerations
To successfully participate in a telehealth session, the patient was required to demonstrate the ability to sustain adequate attention, be alert and oriented to self and place, have adequate impulse control, and follow 1-step commands for remote setup. This was determined from chart review, clinical decision of the treating therapist based on previous performance, and/or interdisciplinary communication with unit or department staff.
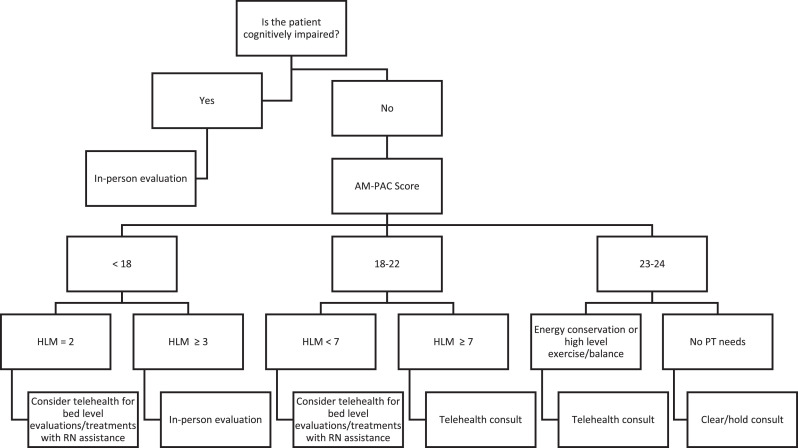
Physical therapy algorithm
In addition to the multidisciplinary considerations, the physical therapy algorithm used 2 in-house mobility assessments, the AM-PAC and the Johns Hopkins Highest Level of Mobility (JH-HLM), to assess patient independence and filter appropriate candidates. Like the AM-PAC, the JH-HLM is completed daily by nursing staff and documents a patient's highest level of observed mobility, using an ordinal scale ranging from lying in bed (score=1) to ambulating ≥250 ft (score=8).8 , 9 For example, a 3 onthe JH-HLM would equal sitting on the side of the bed. Therefore, if a patient's documented HLM is a 3, then the highest level of mobility completed within that documentation time period was to sit on the side of the bed, whereas a patient with an HLM of 6 would indicate that the patient was walking 10 or more steps (fig 1 ).
Fig 1.
PT decision-making algorithm. A comprehensive flow chart guiding clinical reasoning for physical therapists to appropriately identify patients for telehealth intervention. Abbreviation: RN, Registered Nurse.
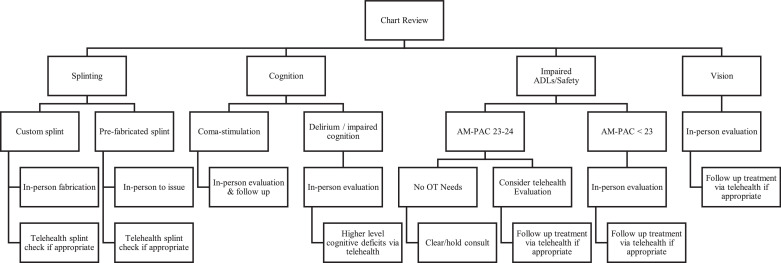
Occupational therapy algorithm
In addition to the multidisciplinary considerations, OTs completed more in-depth chart review based on the specific reason for the OT order. The most common orders were identified as splinting, cognition, impaired activities of daily living/safety, and vision. The OT decision-making algorithm guided the therapists to make clinical decisions based on the OT order as well as the needs of the patient (fig 2 ).
Fig 2.
OT decision-making algorithm. A comprehensive flow chart guiding clinical reasoning for occupational therapists to appropriately identify patients for telehealth intervention.
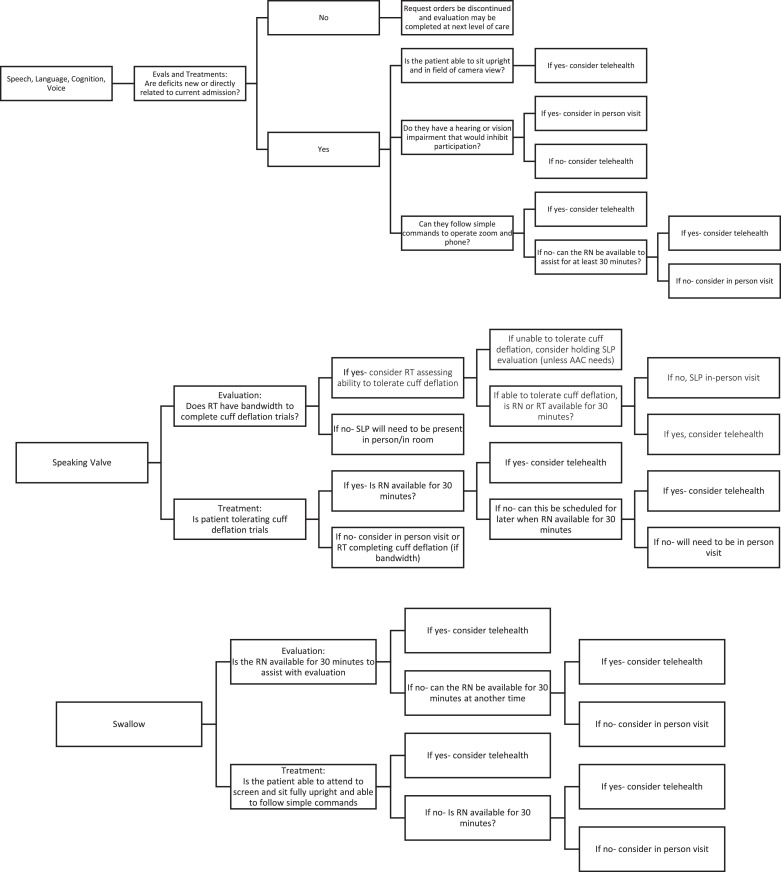
Speech language pathology algorithm
Patients who met the multidisciplinary criteria could participate in treatment for dysphagia, voice disorders, language and cognitive disorders, dysarthria, and motor-speech disorders. Instrumental swallowing evaluations were not considered for telehealth evaluations because of equipment needs. The algorithms were specifically designed with safety in mind and therefore were stringent in the selection of patients for noninstrumental swallow evaluations and speaking valve sessions. Although these were not a direct exclusion, no patients were identified as appropriate during the telehealth outreach (fig 3 ).
Fig 3.
SLP decision-making algorithm. A comprehensive flow chart guiding clinical reasoning for speech language pathologists to appropriately identify patients for telehealth intervention. Abbreviations: RN, Registered Nurse; RT, Respiratory Therapist.
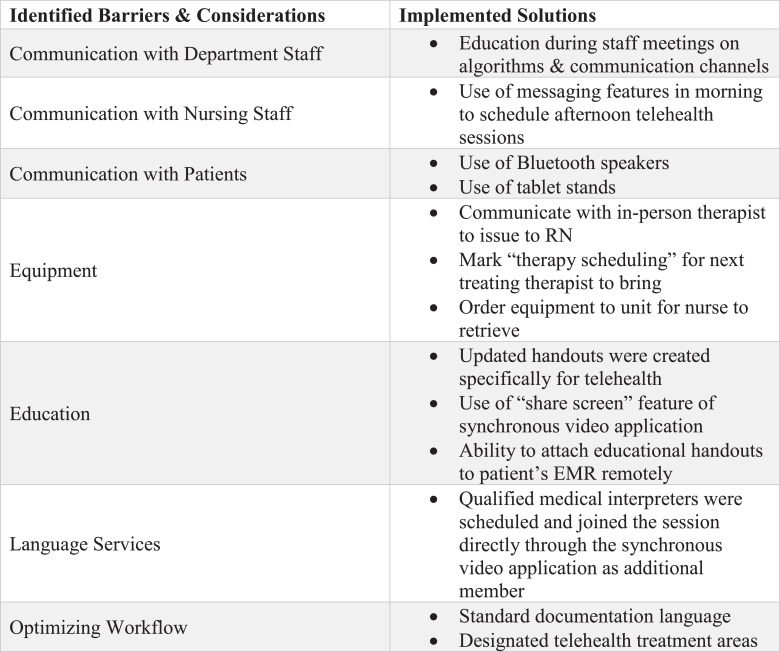
Barriers to implementation
Several barriers arose during the initial sessions of telehealth requiring solutions to maximize the outcome of the treatment delivery method. The barriers included the following:
-
•
Communication with the therapy department staff, the nursing staff, and the patient: Calling the nursing staff to schedule sessions had the potential to be difficult, either because of the inability to answer or personal protective equipment causing difficulty hearing between providers. Communicating with the patient also was a barrier. For example, the protective cases on the bedside tablets diminished audio output, preventing patients from hearing the therapist. Conversely, therapists also had difficulty hearing patients if exhibiting dysphonia.
-
•
Equipment: Although the purpose of telehealth was to prevent contact, contact is required for the issuing of a physical item discussed or educated during therapy sessions.
-
•
Education: Typical education methods of providing handouts or using educational tools during treatments sessions were limited secondary to remote work.
-
•
Language services: Patients requiring language interpretation were screened as appropriate for telehealth via the algorithms, but this posed as a barrier if they did not speak the primary language of the telehealth therapist.
-
•
Workflow, documentation, and efficiency: The unique content and structure of telehealth sessions required ample amounts of free-text information, which increased documentation time.
Considerations and solutions
Communication with department staff, nursing staff, and patients
The treating therapists on the biocontainment units and departmental staff outside of the core telehealth team were vital to implementing telehealth in the acute hospital setting. All departmental therapists were provided with education on the decision-making algorithms, communication channels, and telehealth operation details during staff meetings. Details shared were inclusive of (1) patient identification, departmental therapists were taught to use discipline-specific algorithms to identify patients appropriate for telehealth, and (2) communication of patient identification, departmental therapists were taught to use the EMR and the feature “Therapy Scheduling” to communicate telehealth appropriateness with the associated discipline-specific telehealthteam. Department staff were updated on telehealth changes, provided an opportunity to ask questions, and reminded of telehealth parameters at monthly staff meetings and weekly discipline-specific meetings. This aided in continued appropriate use of clinical reasoning to identify and reassess patient telehealth appropriateness daily.
To communicate with the nursing staff, the adopted workflow included reaching out to nursing in the morning to schedule telehealth intervention in the afternoon. The EMR “Chat” messaging feature proved successful for communication, allowing the nurses to answer at their convenience and refer to the details of the session if needed. Messages to nursing included the intended time of intervention and asked them to leave the room phone and bedside tablet within reach of the patient when they were next in the patient room. In addition to therapists, physicians and other providers were using telehealth to connect with the patients. As the use of telehealth streamlined throughout the hospital, including using a synchronous video application to communicate with family, nursing staff became competent with use of the technology and devices. This communication strategy was determined the most efficient for workflow and to reduce burden on staff.
To communicate with the patients, Bluetooth speakers were provided to connect with and solve the barrier of the patient's inability to hear effectively.
Access to telehealth improved communication with physical medicine and rehabilitation physicians as they coordinated with in-person therapists to join therapy sessions to better assess the patient, collaborate with the therapy team, and contribute to discharge planning.
Equipment
Each patient required basic equipment to participate in a telehealth session. The hospital provided bedside tablets in all rooms available for patient use. These tablets came preinstalled with approved applications to serve several purposes, including synchronous video with family, communication, and access to leisure applications. These tablets were also used for telehealth intervention. The hospital provided Bluetooth speakers for patients with hearing deficits or for those who required translation services. In addition, unit-based tablet stands could be acquired for patients if needed for independent use.
Patients also required access to rehabilitation equipment for treatment advancement that telehealth therapists were unable to provide remotely. To solve this, therapists communicated equipment needs with coworkers who were treating on the unit and could deliver to the patient's nurse. Alternatively, the telehealth therapist could communicate the equipment need via “Therapy Scheduling” for the next in-person therapist to deliver or order equipment directly to the unit for the nurse to issue on its arrival.
Education
Given the ability to “share screen” with the synchronous video application, educational handouts were updated and created for the purpose of telehealth intervention. These handouts included energy conservation strategies, breathing techniques, fall precautions, home safety recommendations, and exercise programs including fine motor coordination, range of motion, strengthening, and swallowing exercises. Handouts used during telehealth were attached to the patient's medical record, enabling them to receive a printed copy at time of discharge.
Language services
For patients who required interpretation services, a qualified medical interpreter joined the therapy session directly through the synchronous video application as an additional member. The treating therapist emailed the hospital's Language Access Services department in the morning, requesting an interpreter to join the telehealth session. Within the initial email, the therapist provided information including the language needed, the patient's medical identification number, the practitioner's contact information, the access information for the synchronous video application, and a time frame. Once an interpreter acknowledged the session, the therapist confirmed the session time with the patient and their nurse. Incorporating an interpreter into a telehealth session required increased planning and coordination, however not significantly more than scheduling an in-person interpreter. This was also easily incorporated into the telehealth workflow because treating therapists were already communicating with the nursing staff in the morning remotely, and a standardized email format was developed to easily include all needed information.
Optimizing workflow
Given the uniqueness of telehealth treatment sessions and the need for service delivery from an alternate location, workflow required renovation. Two key components in optimizing workflow included documentation efficiency and space availability. The telehealth team established standardized documentation language for treatment, education, and goals that allowed for customization of patient-specific details, thus adding to quickness of free-text documentation. The department also designated several spaces for telehealth use and door signs implemented to ensure privacy when telehealth was in session (fig 4 ).
Fig 4.
Barriers, considerations, and solutions. A concise summary of the barriers therapists faced, factors considered, and solutions generated through the process of telehealth implementation. Abbreviation: RN, Registered Nurse.
Therapy interventions
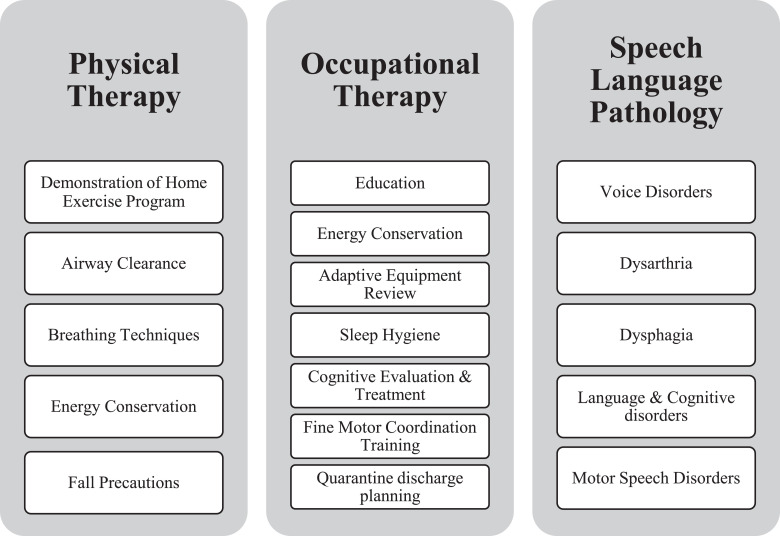
As stated in the national association guidelines, therapy provided via telehealth must be of equal quality as in-person services. To uphold this standard, telehealth therapists were limited to a specific selection of interventions that could be performed remotely. Interventions were developed from clinical experience and grew over time as therapists gained knowledge and confidence with telehealth. Patients who met the multidisciplinary considerations and discipline-specific algorithm criteria were identified as appropriate for telehealth intervention (fig 5 ). The PT, OT or SLP on the telehealth team then scheduled a telehealth session and used the following interventions to meet therapy goals.
Fig 5.
Discipline-specific interventions. A list of interventions, per discipline, that can successfully be performed via telehealth.
Physical therapy interventions
Demonstration of home exercise program
Patients appropriate for therapeutic exercise to address functional strength and endurance deficits were prescribed patient-specific exercise programs. Via screen sharing, patients were able to see images of prescribed exercises, received skilled demonstrations and/or verbal cueing, and then performed exercises with immediate feedback from the therapist.
Airway clearance
To aide with sputum production and evacuation, intervention for airway clearance included patient performance of positive airway pressure devices and education on optimal techniques for producing sputum, including the huff cough.
Breathing techniques
Patients admitted for COVID-19 were often noted to have increased levels of anxiety. Breathing techniques that used deep, calming breathing had the combined effect of optimizing lung expansion, decreasing breathlessness and reducing anxiety.10 The “square breathing” technique was used as simple introduction and progressed as tolerated. Incentive spirometry was used to promote lung expansion and effective ventilation.
Energy conservation
The pulmonary effect of COVID-19 and reliance on supplemental oxygen often caused endurance issues. Patient-specific education was provided to optimize functional independence within current pulmonary impairments and prevent adverse effect. These interventions were used to improve activity tolerance, often via screen sharing to review handouts and reciprocate techniques while on video.
Fall precautions
As patients prepared for discharge home, PTs were able to review techniques to decrease risk of falls, as well as perform higher level balance interventions and attached associated patient education handouts to their discharge paperwork. The teach-back method was used to facilitate patients directing their own family to assist appropriately or provide supervision for necessary tasks.
Occupational therapy interventions
Education
The main patient education points for OT intervention included energy conservation, breathing techniques, fall prevention, and home safety. These topics were included in many of the OT telehealth sessions, either as the primary or supplemental intervention. A variety of educational methods were used, such as the teach-back technique and “share screening” of educational packets to ensure carryover of learning.
Adaptive equipment review
During traditional in-person sessions, various types of adaptive equipment, such as a sock aid or reacher, were issued as appropriate. During telehealth follow-ups, the OTs continued education on appropriate use of the equipment and had patients demonstrate competency of equipment use.
Sleep hygiene
Sleep intervention was adapted to remote intervention by facilitating education and discussion regarding quality of sleep and barriers to sleep, as well as using questionnaire-based assessments to objectively document sleep dysfunction and guide personalized goal setting. The OT could also order “sleep kits” to the patient's room, which composed of eye masks, ear plugs, and an informative sheet regarding television channels for relaxation music to aid in environmental modification for increased sleep hygiene.
Cognitive evaluation and treatment
For high level cognitive deficits, some assessments were modified to be completed remotely. An example of this is the Hopkins Medication Schedule.11 To implement this assessment, the “share screen” function allowed the patient to view the intended document needed to complete the test. Treatments to address cognition, such as puzzles, picture comprehension tasks, sequencing cards, and simulated meal preparation, were also adapted to telehealth. Cognitive stimulation activities, such as orientation boards and daily routine schedules, were also used to address and prevent patient delirium.
Fine motor coordination training
Fine motor coordination was addressed using visual demonstration via synchronous video in addition to “screen sharing” a handout of picture-based hand exercises for fine motor coordination intervention. Exercise equipment needed for intervention, such as foam blocks or Theraputty, were delivered to the patient in a prior therapy session by an in-person therapist.
Quarantine discharge planning
The population with COVID-19 requires special attention to discharge planning given the sensitivity of the pandemic to the population. This means that some patients must self-quarantine after discharge. Using telehealth, OTs were able to assist in quarantine planning with education on home setup and durable medical equipment, use of technology to ensure appropriate telehealth follow-up with providers, and available modes of communication with family and friends to facilitate patient safety and independence in an isolated environment.
Speech language pathology interventions
Dysphagia intervention
The focus of this intervention was to target dysphagia goals including effortful swallowing, increased frequency of swallowing, hard/fast swallowing, use of expiratory muscle strength trainer, and observation of previously recommended compensatory strategies. Results of instrumental swallowing evaluations, including video swallowing studies and fiber-optic endoscopic evaluations, and education on diet recommendations and goals could be shared during this intervention session.
Voice intervention
As a result of prolonged intubation, many patients experienced aphonia or dysphonia. Patients with primary goals for voice intervention were a target population given their lack of comorbidities, intact cognitive abilities, and low frequency need to be provided with tactile cueing during a session. In addition, SLPs noted increased ability to perceive vocal characteristics and increased intelligibility during telehealth because of the patient speaking directly into the tablet microphone and the ability to control the volume and amplify the patient's voice.
Cognitive-linguistic screening
During treatment sessions targeting dysphagia or voice goals, the SLP also performed cognitive screening to determine need for further examination. For example, if using the Saint Louis University Mental Status Exam,12 the patient would be provided with a pencil and paper with the figures for the 2 questions requiring written stimuli prior to the session. Verbal stimuli were easily recorded remotely, and the written portions were assessed by the patient turning their work to the camera for clinician interpretation. Results of the screenings, collateral information from the medical record, and discussion with patient's family member helped in identifying a change from baseline performance and need for formal testing.
Conclusions
PTs, OTs, and SLPs in the acute care setting turned to telehealth in a time of need to adapt and respond during the COVID-19 pandemic. A multidisciplinary team of rehabilitation professionals rapidly developed decision-making algorithms, practices, educational materials, and intervention strategies to efficiently provide quality services to patients. The acute care setting is historically fast paced and constantly changing, which can be a challenge, thus making the implementation of telehealth a particularly unique undertaking. However, recent global events have prompted a change in policy of the APTA, AOTA, ASHA, and Centers for Medicare and Medicaid Services to include PTs, OTs, and SLPs as eligible telehealth providers. This makes telehealth a valuable resource as we continue to progress effective treatment and patient outcomes in the acute hospital setting.
Throughout the pandemic, telehealth sessions were successfully completed using the aforementioned protocols, algorithms, interventions, and solutions by a multidisciplinary team of rehabilitation professionals. Although this is considered a success to overcome an unprecedented challenge, the telehealth outreach was suspended as full biocontainment units closed. However, with these resources, the program is ready to be reimplemented as needed to continue to provide skilled patient care and maximize positive patient outcomes in future situations.
Footnotes
The authors are acute care occupational therapists, physical therapists, and speech language pathologists practicing at The Johns Hopkins Hospital treating patients in the intensive care units and nursing step-down units across all services and specialties. Holly Russell is an occupational therapist and an acute care team leader at The Johns Hopkins Hospital.
Disclosures: none
References
- 1.American Physical Therapy Association. Telehealth. Available at: https://www.apta.org/siteassets/pdfs/policies/telehealth.pdf. Accessed August 18, 2020.
- 2.Shaw DK. Overview of telehealth and its application to cardiopulmonary physical therapy. Cardiopulm Phys Ther J. 2009;20:13–18. [PMC free article] [PubMed] [Google Scholar]
- 3.American Occupational Therapy Association Telehealth in occupational therapy. Am J Occup Ther. 2018;72(Suppl 2) [Google Scholar]
- 4.American Speech-Language-Hearing Association. Telepractice. Available at: www.asha.org/Practice-Portal/Professional-Issues/Telepractice/. Accessed August 18, 2020.
- 5.Lee AC, Harada N. Telehealth as a means of health care delivery for physical therapist practice. Phys Ther. 2012;92:463–468. doi: 10.2522/ptj.20110100. [DOI] [PubMed] [Google Scholar]
- 6.Lee AC. COVID-19 and the advancement of digital therapist practice and telehealth. Phys Ther. 2020;100:1054–1057. doi: 10.1093/ptj/pzaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. AM-PAC “6-clicks” functional assessment scores predict acute care hospital discharge destination. Phys Ther. 2014;94:1252–1261. doi: 10.2522/ptj.20130359. [DOI] [PubMed] [Google Scholar]
- 8.Hiser S, Chung CR, Toonstra A. Inter-rater reliability of the Johns Hopkins Highest Level of Mobility Scale (JH-HLM) in the intensive care unit. Braz J Phys Ther. 2020;25:352–355. doi: 10.1016/j.bjpt.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoyer EH, Young DL, Klein LM. Toward a common language for measuring patient mobility in the hospital: reliability and construct validity of interprofessional mobility measures. Phys Ther. 2018;98:133–142. doi: 10.1093/ptj/pzx110. [DOI] [PubMed] [Google Scholar]
- 10.Borge CR, Mengshoel AM, Omenaas E. Effects of guided deep breathing on breathlessness and the breathing pattern in chronic obstructive pulmonary disease: a double-blind randomized control study. Patient Educ Couns. 2015;98:182–190. doi: 10.1016/j.pec.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 11.Carlson M, Fried L, Tekwe C, Brandt J. Validation of the Hopkins Medication Schedule to identify difficulties in taking medications. J Gerontol A Biol Sci Med Sci. 2005;60:217–223. doi: 10.1093/gerona/60.2.217. [DOI] [PubMed] [Google Scholar]
- 12.Tariq SH, Tumosa N, Chibnall JT, Perry MH, 3rd, Morley JE. The Saint Louis University Mental Status (SLUMS) Examination for detecting mild cognitive impairment and dementia is more sensitive than the Mini-Mental Status Examination (MMSE): a pilot study. Am J Geriatr Psychol. 2006;14:900–910. doi: 10.1097/01.JGP.0000221510.33817.86. [DOI] [PubMed] [Google Scholar]