Fig. 4. Arterial pulsatility propels fluid flow in the brain.
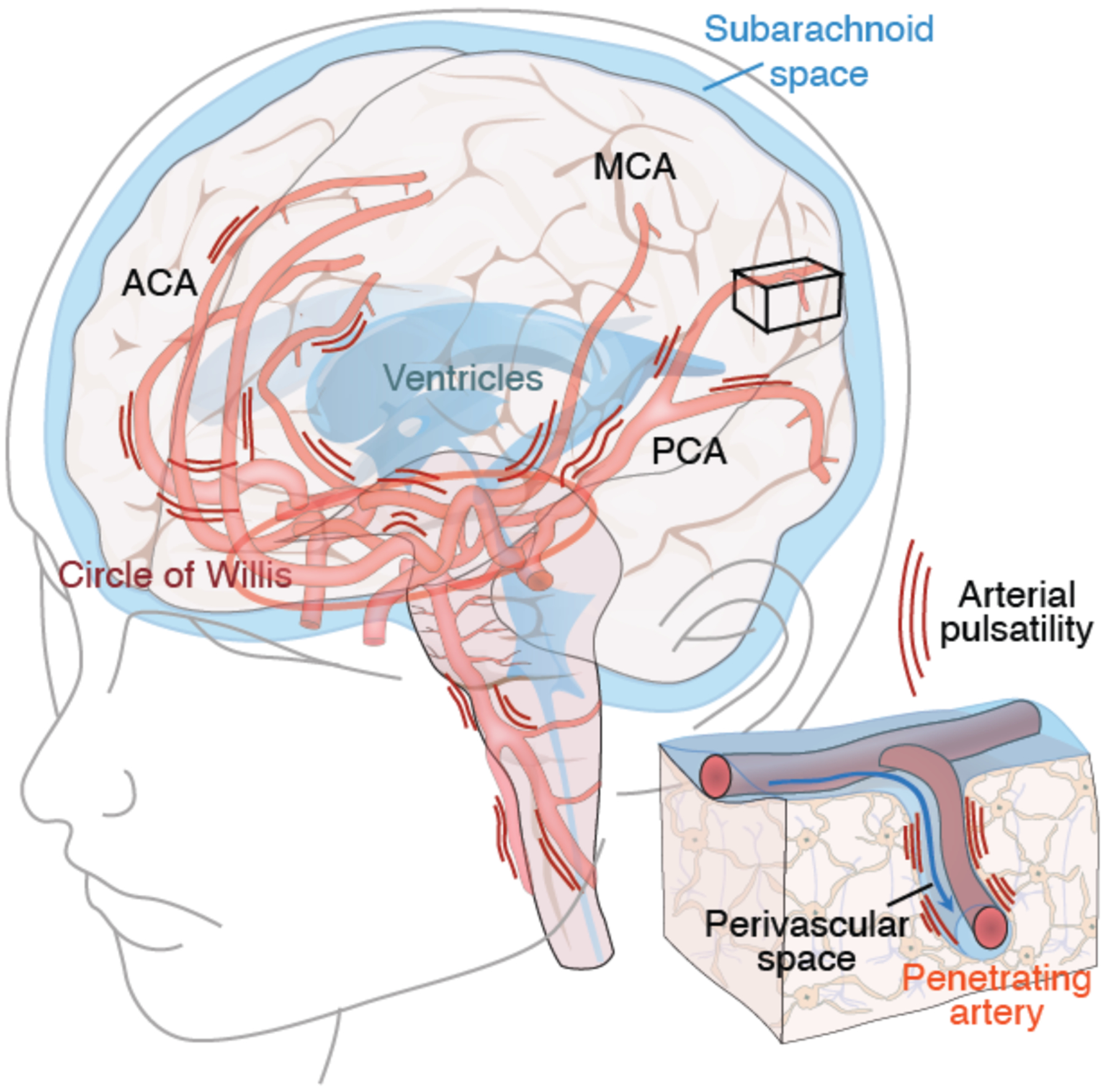
The brain receives 20–25% of cardiac output, yet comprises ~2% of total body weight. The large caliber arteries of the circle of Willis are positioned in the CSF-containing basal cisterns below the ventral surface of the brain. Arterial pulsatility provides the motive force for CSF transit into the perivascular spaces surrounding the major arteries, while respiration and slow vasomotion contribute to sustaining its flow (112). The anterior (ACA), middle (MCA), and posterior (PCA) arteries transport CSF to the penetrating arteries (insert), from which CSF is then driven into the neuropil via the still-contiguous perivascular spaces. Cardiovascular diseases associated with reduced cardiac output, such as left heart failure and atrial arrhythmias, reduce arterial wall pulsatility, resulting in less CSF flow. In addition, thickening of the arterial wall in small vessel disease, hypertension and diabetes all reduce arterial wall compliance and hence pulsatility. Each of these fundamentally cardiovascular disorders serves to attenuate glymphatic flow, providing a potential causal link between these vascular etiologies and Alzheimer disease (113).
