Abstract
OBJECTIVE:
Stress is a risk factor for numerous negative health outcomes, including cognitive impairment in late-life. The negative association between stress and cognition may be mediated by depressive symptoms, which separate studies have identified as both a consequence of perceived stress and a risk factor for cognitive decline. Pathways linking perceived stress, depressive symptoms, and cognition may be moderated by sociodemographics and psychosocial resources. The goal of this cross-sectional study was to identify modifying factors and enhance understanding of the mechanisms underlying the stress–cognition association in a racially and ethnically diverse sample of older adults.
METHOD:
A linear regression estimated the association between perceived stress and episodic memory in 578 older adults (Mage= 74.58) in the Washington Heights-Inwood Columbia Aging Project. Subsequent models tested whether depressive symptoms mediated the stress–memory relationship and whether sociodemographics (gender, race, and ethnicity) or perceived control moderated these pathways.
RESULTS:
Independent of sociodemographics and chronic diseases, greater perceived stress was associated with worse episodic memory. This relationship was mediated by more depressive symptoms. Higher perceived control buffered the association between stress and depressive symptoms. There was no significant moderation by gender, race, or ethnicity.
CONCLUSION:
Depressive symptoms may play a role in the negative association between perceived stress and cognition among older adults, however, longitudinal analyses and studies using experimental designs are needed. Perceived control is a modifiable psychological resource that may offset the negative impact of stress.
Keywords: Depressive symptoms, psychological stress, cognitive aging, sense of control
Introduction
In light of the aging global population, the identification of modifiable factors that can prevent or delay cognitive decline in older adults is increasingly important due to the lack of disease-modifying treatments for late-life cognitive disorders, such as dementia. Stress is a modifiable environmental factor that may have important implications for cognitive aging. The psychological experience of stress includes both the occurrence of stressors (e.g., exposure to traumatic life events, ongoing caregiving burden or job-related strain) and the interpretations of and reactions to these stressors (Cohen, Kessler, & Gordon, 1997). Indeed, it is the subjective perception of distress that likely triggers the cascade of neuroendocrine changes that can negatively affect health outcomes in the presence of stressful life events (Dedovic, Duchesne, Andrews, Engert, & Pruessner, 2009). In addition to being a risk factor for numerous negative late-life physical health outcomes (Epel et al., 2006; Gouin, Hantsoo, & Kiecolt-Glaser, 2008), stress is also a risk factor for late-life cognitive impairment, cognitive decline (Aggarwal, et al., 2014; Peavy et al., 2009), and dementia (Machado et al., 2014).
Perceived Stress and Cognition
Prior research on the effects of stress on cognitive aging has largely focused on the influence of specific negative life events (Dickinson, Potter, Hybels, McQuoid, & Steffens, 2011) or daily stressors (Rickenbach, Almeida, Seeman, & Lachman, 2014) and whether the occurrence of these “objective” stressors is associated with late-life cognitive impairment or decline. However, measuring exposure to stressors alone may not capture the subjective experience of stress due to individual differences in coping style or appraisals of environmental factors and life experiences. Perceived (i.e., subjective) stress reflects an individual’s cognitively mediated emotional response to a stressor, which includes assessment of available coping resources in response to a stressor, regardless of the type of stressor (Cohen, Kamarck, & Mermelstein, 1983). Previous research suggests that higher levels of perceived stress is associated with poorer cognitive functioning among older adults (Munoz, Sliwinski, Scott, & Hofer, 2015). Indeed, high perceived stress was associated with both lower baseline cognition and faster decline over 6 years in adults over age 65 in the Chicago Health and Aging Project (Aggarwal et al., 2014). Further, the cognitive domain of episodic memory appears to be particularly sensitive to the effects of greater perceived stress (VonDras, Powless, Olson, Wheeler, & Snudden, 2005). A deeper understanding of this association is important, as episodic memory difficulties are a prominent aspect of age-related decline, in addition to being one of the earliest predictors of dementia (Bäckman, Small, & Fratiglioni, 2001; Boraxbekk et al., 2015). Although the physiological pathways (e.g., hippocampal atrophy) involving stress biomarkers have been previously explored (Juster, McEwen, & Lupien, 2010; Justice, 2018; McEwen & Sapolsky, 1995), less is known regarding the socioemotional pathways (e.g., depressive symptoms) linking perceived stress and cognition.
The Mediating Role of Depressive Symptoms
In addition to its impact on late-life cognition and dementia pathology, greater perceived stress is also associated with the development of depressive symptoms and clinical depression throughout the lifespan (Cohen, Janicki-Deverts, & Miller, 2007; Tafet & Bernardini, 2003). Further, there is growing evidence that late-life depressive symptoms are prospectively associated with cognitive impairment, and decline, particularly in the domain of episodic memory (Dotson, Resnick, & Zonderman, 2008; O’Shea et al., 2015). Depressive symptoms in late-life have also been associated with clinical dementia (Richard et al., 2013). Results from a meta-analysis revealed that both diagnosed Major Depressive Disorder and depressive symptoms in late-life are associated with increased risk of dementia (Cherbuin, Kim, & Anstey, 2015). There is also evidence to suggest that depressive symptoms precede memory decline, rather than the inverse (Zahodne, Stern, & Manly, 2014).
Despite the link between perceived stress and depression, not all individuals who experience stress develop depressive symptoms or cognitive impairment. Therefore, the presence of depressive symptoms in the face of perceived stress may be an indicator of an individual’s psychological and physiological vulnerability to the toxic effects of stress. Depressive symptoms may therefore function as a mediator of the relationship between perceived stress and cognitive impairment or decline. Most prior studies on perceived stress and late-life cognition have either not considered the role of depressive symptoms or statistically controlled for their presence. However, if depressive symptoms are indeed a part of the underlying process linking perceived stress to late-life cognitive impairment or dementia, interventions designed to reduce or manage depressive symptoms in the face of stress may help promote healthy cognitive aging.
Sociodemographic Moderators
Differential vulnerability to the impacts of perceived stress and depressive symptoms may contribute to late-life disparities in cognitive aging. Women and certain racial and ethnic groups appear to be at greater risk for late-life cognitive disorders such as Alzheimer’s disease (“Alzheimer’s Disease Facts and Figures,” 2019; Carter, Resnick, Mallampalli, & Kalbarczyk, 2012; Mayeda, Glymour, Quesenberry, & Whitmer, 2016; Podcasy & Epperson, 2016). Interactions between sociodemographic characteristics and perceived stress may contribute to these observed inequalities. For example, there is evidence suggesting that older women may experience greater vulnerability to life stress, as evidenced by more symptoms of depression in the presence of chronic financial and health strain, compared to men (Krause, 1986). Analyses of gender differences in stress and coping methods suggest that while men and women may not differ on the number of stressful life experiences, women are more likely to rate stressful events as more negative and less controllable than men (Matud, 2004). There is also evidence for differential biological reactivity to stress between men and women (Verma, Balhara, & Gupta, 2011), which may contribute to the higher incidence, chronicity, and severity of depression among women (Hammen, Kim, Eberhart, & Brennan, 2009; Kessler, 2003; Kornstein, 2002). Thus, it is possible that differences in biological and behavioral responses to stress among men and women contribute to the current gender disparities observed in late-life cognitive outcomes.
Compared with non-Hispanic Whites, racial and ethnic minorities may be especially vulnerable to the negative impact of stress due to negative life events and chronic stressors (Ulbrich, Warheit, & Zimmerman, 1989), in addition to experiencing more stress overall (Golding & Burnam, 1990; Salgado de Snyder, Cervantes, & Padilla, 1990; Shuey & Willson, 2008; Turner & Avison, 2003; Williams, Yan Yu, Jackson, & Anderson, 1997). Indeed, one epidemiological study of older adults documented an increase in experiences of stress due to loss-related events for non-Hispanic Blacks, but not Whites, over a period of nine years (George & Lynch, 2003). Additionally, although stress was associated with depressive symptoms regardless of race, increasing stress explained more variance in depressive symptoms for Blacks than for Whites. Finally, depressive symptoms appear to be more strongly associated with episodic memory and executive functioning in Black older adults compared to White older adults (Zahodne, Nowinski, Gershon, & Manly, 2014).
Prior research on racial/ethnic differences in stress exposure and the impact of stress, however, have largely focused on objective measures of stress rather than perceived stress. Comparisons of perceived stress in response to specific negative life events between Black and White women has revealed group differences in which events were appraised as more subjectively stressful (Vines, Ta, Esserman, & Baird, 2009). Specific types of stress exposure may be unique to racial and ethnic minorities, such as racial discrimination. Differences in perceived stress due to such racial/ethnic differences in stressors, as well as racial/ethnic differences in the likelihood of receiving depression treatments (Williams et al., 2007), may contribute to the current racial and ethnic disparities observed in late-life cognitive outcomes.
Perceived Control
Identifying modifiable factors that can buffer the negative impacts of perceived stress and depressive symptoms can help inform the development of prevention and intervention strategies to reduce cognitive morbidity and eliminate sociodemographic disparities. Perceived control is one modifiable psychological resource that has been shown to buffer against the effects of traumatic (Elliot, Mooney, Infurna, & Chapman, 2017), acute, and chronic (Cummins, 1988; Diehl & Hay, 2010) stress exposure. Perceived control refers to the degree to which people believe that they have the capacity to influence life outcomes (Wallston, Wallston, Smith, & Dobbins, 1987). Epidemiological studies have shown that sense of control is among the most important psychosocial predictors of morbidity, mortality, and psychological well-being in later adulthood, independent of key predictors such as age, gender, disability, and socioeconomic status (Gerstorf et al., 2014; Lachman, 2006). Greater perceived control has also been shown to mitigate risk for the development of depression in the presence of numerous acute and chronic stressors (Grote, Bledsoe, Larkin, Lemay, & Brown, 2007). It may be that individuals with greater perceived control engage in more adaptive or solution-focused coping strategies (Gourounti et al., 2012), which may buffer against the negative effects of perceived stress.
In addition to its association with a variety of mental and physical health outcomes (Chipperfield, Campbell, & Perry, 2004), perceived control is also associated with cognitive performance in domains such as memory, verbal intelligence, and processing speed among young, middle-aged, and older adults (Windsor & Anstey, 2008). Individuals with greater perceived control may be more likely to use compensatory strategies to maintain cognitive functioning (Lachman & Andreoletti, 2006) or engage in health behaviors that can buffer the negative effects of stress on cognition (Infurna & Gerstorf, 2013). Thus, it is possible that differences in perceived control influence the degree to which perceived stress and/or depressive symptoms negatively impact cognition among older adults.
The Current Study
The objective of the current cross-sectional study was to integrate and extend previous research related to perceived stress, depressive symptoms, and cognition in older adults. Our first aim was to replicate prior findings, which suggest that perceived stress may have a negative impact on episodic memory. Thus, we hypothesized that greater perceived stress would be associated with poorer episodic memory (see Figure 1, Path C) in a diverse sample of urban-dwelling older adults.
Figure 1.
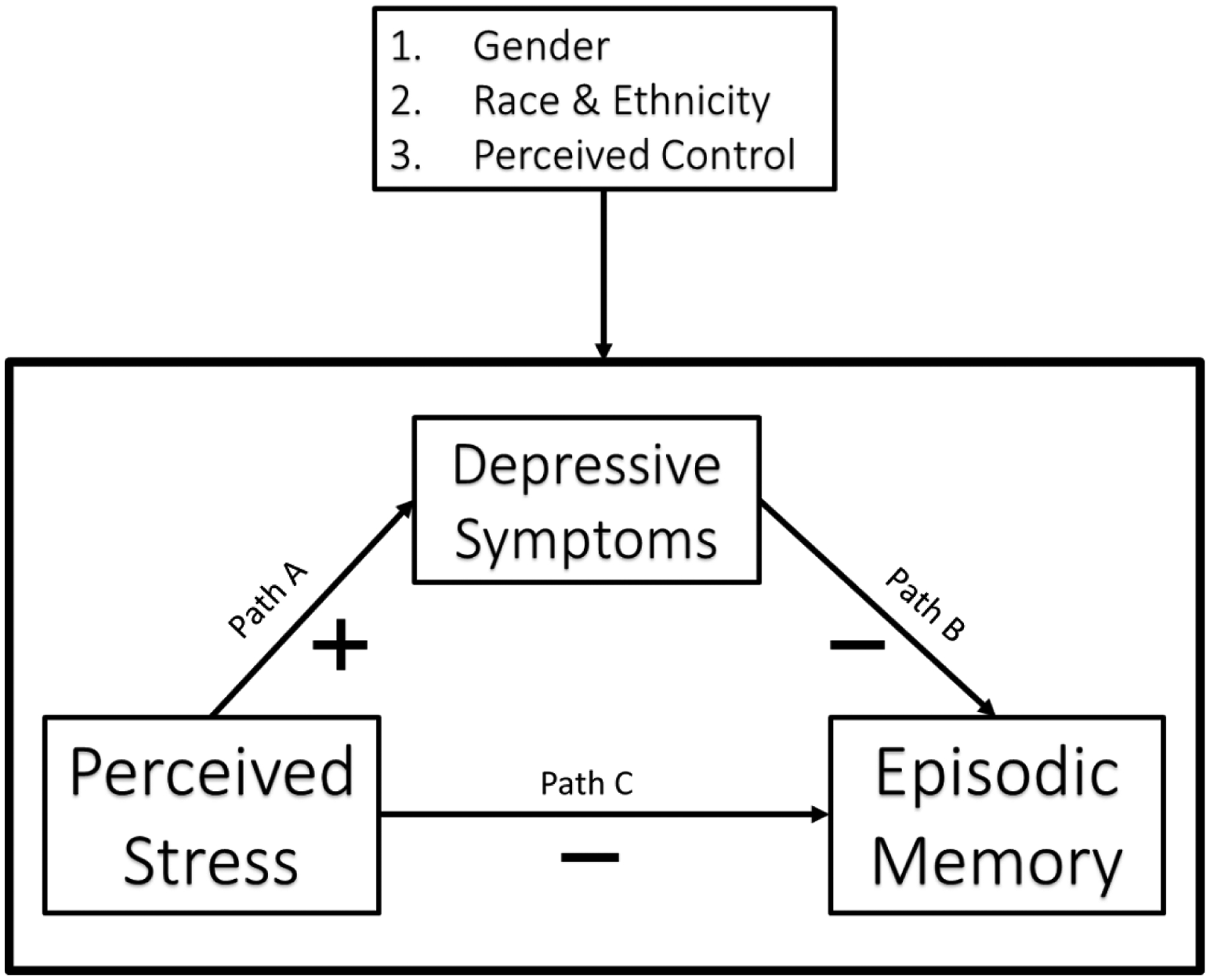
Conceptual model. Hypothesized positive and negative associations between perceived stress, depressive symptoms, and episodic memory are depicted in the conceptual model. Moderating effects of gender, race and ethnicity, and perceived control were tested for the direct (c) and indirect (a and b) paths of the mediation model.
Our second aim was to investigate whether the relationship between perceived stress and memory is mediated by depressive symptoms. Specifically, we hypothesized that higher perceived stress would be associated with more depressive symptoms (Figure 1, Path A), and more depressive symptoms would be associated with worse memory performance (Figure 1, Path B).
Our third aim was to identify sociodemographic and psychological factors that could moderate associations involving perceived stress and depressive symptoms. We hypothesized that (1) the positive association between perceived stress and depressive symptoms, (2) the negative association between perceived stress and episodic memory, and (3) the negative association between depressive symptoms and episodic memory would each be stronger in women, non-Hispanic Blacks, and Hispanics, as compared with men and non-Hispanic Whites, respectively. Additionally, we hypothesized that having more perceived control would be associated with weaker associations among perceived stress, depressive symptoms, and episodic memory (see Figure 1 for the full conceptual model).
Method
Participants and Procedures
The 578 participants included in this study were participants in the Washington Heights-Inwood Columbia Aging Project (WHICAP), a longitudinal study of aging and dementia in a multi-ethnic community cohort in New York, NY (Manly et al., 2005; Tang et al., 2001). Participants residing in the northern Manhattan communities of Washington Heights and Inwood were identified through Medicare records and recruited for the prospective study beginning in 1992. Additional participants were recruited in waves beginning in 1999 and 2009. Participants are followed up every 18 to 24 months and undergo detailed assessments of physical health, functional abilities, and cognition in their preferred language of English or Spanish. Cognitive functioning is assessed in-person through a comprehensive neuropsychological battery. Importantly, the same cognitive constructs of memory, language, visual-spatial abilities, and processing speed are measured by the English and Spanish batteries as demonstrated through prior factor analysis in WHICAP (Siedlecki et al., 2010). Beginning in 2013, 600 non-demented participants recruited in the most recent wave (beginning in 2009) also completed validated measures of psychosocial functioning as part of an ancillary study (Zahodne, Watson, Seehra, & Martinez, 2017). Thus, the present cross-sectional study uses data obtained from these participants during study visits that occurred between 2013 and 2017.
Participants were included in the present study if they (1) had available data on the variables of interest (see below) and (2) self-identified as non-Hispanic Black, non-Hispanic White, or Hispanic of any race (9 participants who identified as “other” race were excluded). Over 95% of participants were retained, leading to a final sample size of 578 individuals. Informed consent was obtained from all participants, and the study was approved by the Columbia University Institutional Review Board. Descriptive characteristics on all study participants are summarized in Table 1.
Table 1.
Participant characteristics
| Mean (SD) or % | ||
|---|---|---|
| Age (60–95) | 74.58 (6.16) | |
| Gender (% women) | 63.70 | |
| Race & ethnicity (%) | ||
| Non-Hispanic Black | 41.50 | |
| Hispanic (any race) | 27.50 | |
| Non-Hispanic White | 31.00 | |
| Education (0–20 years) | 13.19 (4.43) | |
| Physical health (0–3 diseases) | 1.03 (0.87) | |
| Perceived stress (−4–4) | −0.20 (1.03) | |
| Depressive symptoms (0–10) | 1.28 (1.74) | |
| Perceived control (1–7) | 5.43 (1.09) | |
| Episodic memory (−2.33–2.04) | 0.58 (0.73) | |
Measures
Outcome
Episodic memory was assessed via the Selective Reminding Test (SRT; Buschke & Fuld, 1974). Previous studies demonstrated the clinical utility of the SRT in differentiating normal cognitive aging from dementia at preclinical stages (Masur et al., 1989). A list of twelve words were presented and participants were given six trials to learn this list. At the end of each trial, participants were reminded of any words they failed to recall immediately following list presentation. A total learning score was computed as the sum of words correctly recalled over the six trials. Delayed free recall and recognition were assessed after a fifteen-minute delay. A memory composite score was computed by averaging the z-scores from initial learning, delayed recall, and recognition trials of the SRT based on the performance of the larger WHICAP sample. Higher scores correspond to better memory performance.
Exposure
Perceived stress was measured using the NIH Toolbox Perceived Stress Survey (Kupst et al., 2015; Salsman et al., 2013), a 10-item version of the Perceived Stress Scale (Cohen et al., 1983), which has been demonstrated to have good internal consistency (Cronbach’s alpha= 0.91) and concordance with objective measures of stress exposure, such as life-events or daily stressors scales (Stawski, Sliwinski, Almeida, & Smyth, 2008). The 10-item scale has demonstrated measurement invariance across English and Spanish languages (Perera et al., 2017), gender, and time (Barbosa-Leiker et al., 2013), and has also been validated for use with older adults (Ezzati et al., 2014). Participants rated the frequency of stressful experiences and the extent to which they felt strained or overloaded during the past month (e.g., How often have you felt nervous and “stressed”? How often have you felt difficulties were piling up so high that you could not overcome them?) on a five-point scale, ranging from Never (1) to Very Often (5). A theta score (range −4 to 4) was computed for each participant, representing the overall perceived stress for that participant; higher scores correspond to greater perceived stress.
Mediator
The presence of depressive symptoms during the week leading up to the interview was assessed with 10 items from the Center for Epidemiologic Studies Depression (CES-D) Scale (Irwin, Artin, & Oxman, 1999). Prior research on older adults has demonstrated the shortened and dichotomous version of the CES-D scale to have adequate internal consistency (Cronbach’s alpha= 0.78), measurement invariance across English and Spanish languages (González et al., 2017), and factor structure in line with the original 20-item measure which assesses frequency of depressive symptoms on a 4-point Likert scale (Turvey, Wallace, & Herzog, 1999). Items such as “Everything was an effort” and “I felt depressed” were presented in yes (1)/ no (0) format. Responses were summed, and higher scores correspond to the presence of more depressive symptoms.
Moderators
Sociodemographic data.
The WHICAP population comprises three primary racial and ethnic groups: non-Hispanic Black/African American, Hispanic (mostly Caribbean Hispanic), and non-Hispanic White. Race and ethnicity were self-reported, and participants were dummy-coded into three, mutually-exclusive categories: non-Hispanic Black, non-Hispanic White, and Hispanic of any race. Non-Hispanic White was selected as the reference category. Gender was assessed via self-report and coded as a dichotomous variable (men/ women) with men as the reference category.
Perceived Control.
Perceived control was assessed using the Perceived Control Questionnaire (Lachman & Weaver, 1998). Of the 578 participants included in this study, 441 had available data on this measure. The questionnaire is composed of twelve statements that assess sense of personal mastery (i.e., “I can do just about anything I really set my mind to”) and perceived constraints on life situations (i.e., “There are many things that interfere with what I want to do”). Participants rated responses on a 7-point Likert scale ranging from Strongly Agree (1) to Strongly Disagree (7). Four of the twelve items were reverse-coded, and a total perceived control score (average) was computed such that higher scores indicate greater perceived control.
Covariates
Age, education, gender, race and ethnicity, and physical health were included as sociodemographic covariates in the primary model (Aim 1). Age was participants’ age (in years) at the time of assessment. Education was participants’ self-reported years of education (0–20). Physical health was assessed via self-report and quantified as the sum of the presence of hypertension, diabetes, and heart disease.
Analytic Strategy
Statistical analyses were conducted using IBM SPSS v. 25. Differences in perceived stress, depressive symptoms, and memory between genders and across racial/ethnic groups were assessed with t-tests and ANOVAs. Multiple linear regression models examined direct and indirect effects of perceived stress on episodic memory through depressive symptoms. These models controlled for age, education, gender, race and ethnicity, and physical health. Subsequent models systematically tested for moderation of the perceived stress–depressive symptoms–episodic memory mediation pathways (see Figure 1). Mediation and moderated-mediation effects were probed for further analysis using the PROCESS modeling tool for SPSS (Hayes, 2017). Confidence intervals (CI) of indirect effects (i.e., mediation) of perceived stress through depressive symptoms were generated through 5,000 bootstrapped samples (Hayes, 2017). Four separate moderated-mediation models included interaction terms involving each of the proposed moderators: gender, Black race, Hispanic ethnicity, and perceived control. Conditional direct and indirect effects of perceived stress were assessed comparing both genders, the three racial/ethnic groups, and three levels of perceived control (high= +1 SD, medium= mean, low= −1SD). Diagnostics were included to test for multicollinearity with tolerance value <.2 and variance inflation factor (VIF) value >4.0 as cutoffs (Garson, 2012). Statistical significance at all levels of analysis was evaluated at the p < .05 level.
Results
Results from the initial regression model are summarized in Table 2, and all significant paths are depicted in Figure 2. Results did not indicate any concerns of multicollinearity among variables. Participants included in the study (N=578) did not differ from those who were excluded (N=22) due to missing data on variables of interest (all ps > .05), except for race and ethnicity. Specifically, the proportion of non-Hispanic Blacks to non-Hispanic Whites was larger among excluded participants (2.25:1) than included participants (1.34:1).
Table 2.
Linear regression of perceived stress and episodic memory (Aim 1)
| B | SE | β | |
|---|---|---|---|
| Age | −0.03*** | 0.00 | −0.22 |
| Education | 0.04*** | 0.01 | 0.26 |
| Female | 0.23*** | 0.06 | 0.15 |
| Black | −0.31*** | 0.07 | −0.21 |
| Hispanic | −0.29** | 0.09 | −0.18 |
| Physical Health | −0.05 | 0.03 | −0.06 |
| Perceived Stress | −0.06* | 0.03 | −0.08 |
Note. B= unstandardized coefficient. SE= standard error. β= standardized coefficient.
p<.05,
p<.01,
p<.001
Figure 2.
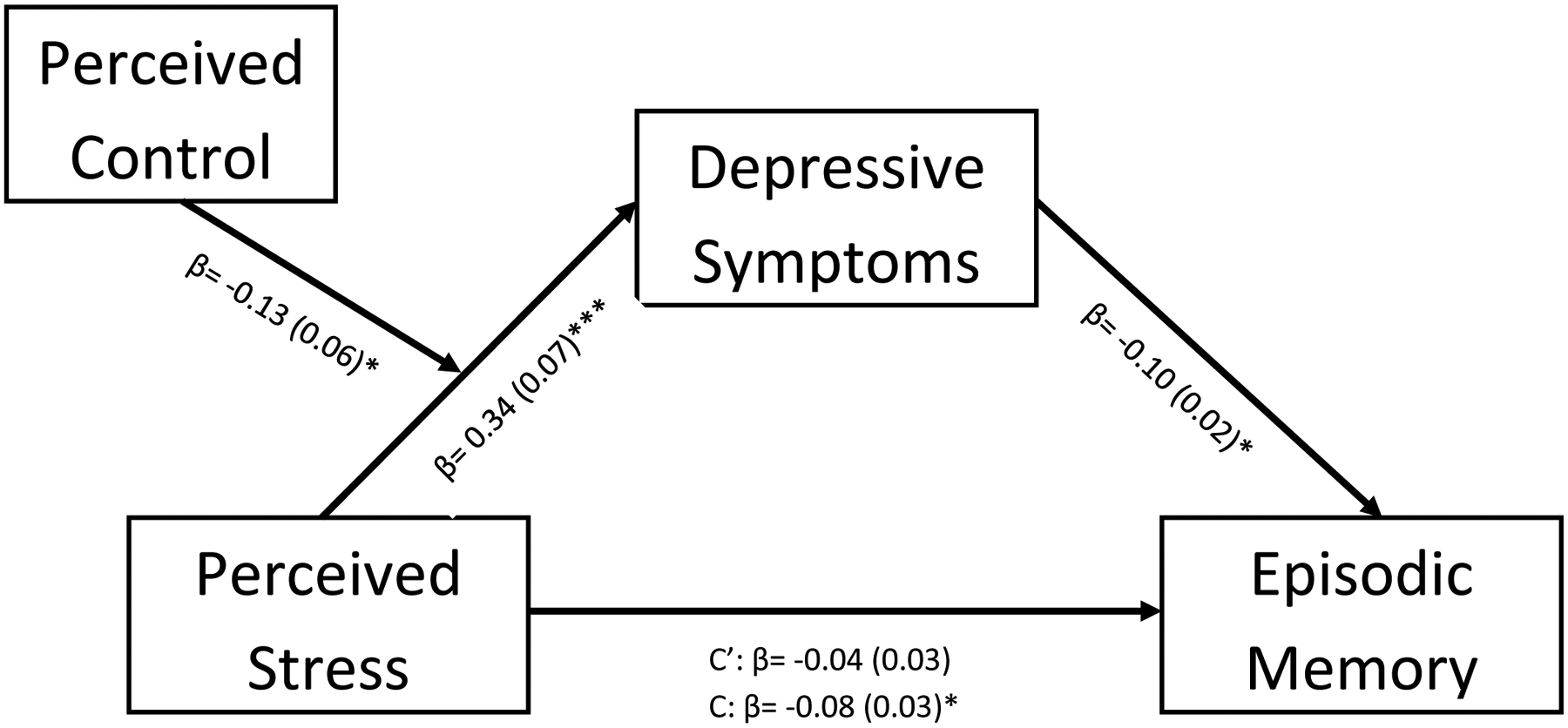
Standardized estimates from all significant paths. C= total effect. C’= direct effect.
*p<0.05, **p<0.01, ***p<0.001
Mediation (Aims 1 & 2)
The initial regression model excluding depressive symptoms indicated a negative relationship between perceived stress and episodic memory. Specifically, greater perceived stress was associated with worse episodic memory, independent of the covariates (β = −0.08, SE= 0.03, p< .05). A subsequent model revealed a negative indirect effect of perceived stress on memory through depressive symptoms (completely standardized indirect effect = −0.03, SE= 0.01, 95% CI [−0.06, −0.01]). As shown in Figure 2, greater perceived stress was associated with more depressive symptoms (β = 0.34, SE= 0.07, p< 0.001), and more depressive symptoms was associated with worse memory (β = −0.10, SE= 0.02, p= .01).
Robustness of findings was confirmed with the following sensitivity analyses: (1) running an alternate model with perceived stress as the mediator between depressive symptoms and episodic memory, (2) replacing the memory composite with the SRT components (initial learning, delayed recall, and recognition) as separate memory outcomes, (3) excluding participants with mild cognitive impairment, (4) adding monthly household income as an additional covariate, (5) expanding the physical health covariate, and (6) adding time between assessment dates as a covariate. Detailed results are provided in the Supplementary Materials. Notably, effects of perceived stress, both directly and indirectly through depressive symptoms, were the same as the original analyses for initial learning and delayed recall, but not recognition. Upon adjusting for income, depressive symptoms was no longer a significant mediator of the association between perceived stress and episodic memory (completely standardized indirect effect = −0.02, SE= 0.01, 95% CI [−0.05, 0.00]) because there was no longer an association between depressive symptoms and memory (β = −0.07, SE= 0.02, p= .07). However, the total effect of perceived stress on episodic memory (β = −0.08, SE= 0.03, p< .05) and the association between perceived stress and depressive symptoms (β = 0.34, SE= 0.07, p< .001) did not change from the original model.
Moderated Mediation (Aim 3)
Mean comparisons of key study variables (perceived stress, depressive symptoms, episodic memory) across race, ethnicity, and gender are reported in Table 3. Analyses revealed racial and ethnic differences in perceived stress (F(2, 575)= 3.26, p< .05) and episodic memory (F(2, 575)= 36.75, p< .001). Non-Hispanic Blacks reported the highest perceived stress, followed by non-Hispanic Whites and Hispanics, and post-hoc comparisons using the Tukey HSD test revealed a significant difference (p= .02, Cohen’s d= .24) between non-Hispanic Blacks and Hispanics only. All three racial and ethnic groups differed on episodic memory (all ps ≤ .01, ds= .29–.95), such that non-Hispanic Whites demonstrated the highest episodic memory, followed by non-Hispanic Blacks, then Hispanics. There were also gender differences in perceived stress (t(576)= −2.09, p< .05) and episodic memory (t(576)= −2.44, p< .05). Specifically, women reported higher perceived stress (d= .18) and episodic memory (d= .21) compared to men. There were no group differences in depressive symptoms.
Table 3.
Mean differences in key study variables across race/ethnicity and gender
| Perceived Stress | Depressive Symptoms | Episodic Memory | ||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |
| non-Hispanic White (W) | −0.24 | 1.01 | 1.19 | 1.52 | 0.93 | 0.61 |
| non-Hispanic Black (B) | −0.08 | 0.92 | 1.30 | 1.82 | 0.51 | 0.74 |
| Hispanic (H) | −0.33 | 1.17 | 1.36 | 1.85 | 0.30 | 0.71 |
| Group Differences | B>H | none | W>B>H | |||
| Men (M) | −0.32 | 1.03 | 1.13 | 1.56 | 0.48 | 0.72 |
| Women (F) | −0.13 | 1.01 | 1.37 | 1.83 | 0.63 | 0.74 |
| Group Differences | F>M | none | F>M | |||
Note. All group differences were evaluated at p< .05
In a moderated mediation model, neither gender nor race/ethnicity moderated any associations among perceived stress, depressive symptoms, and episodic memory (Table 4).
Table 4.
Standardized regression results of interactions with moderators (Aim 3)
| Perceived Stress → Depressive Symptoms | Depressive Symptoms → Episodic Memory | Perceived Stress → Episodic Memory | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Moderator | β | SE | p | β | SE | p | β | SE | p |
| Female gender | 0.02 | 0.04 | 0.55 | −0.01 | 0.04 | 0.81 | 0.06 | 0.04 | 0.15 |
| Black race | 0.06 | 0.04 | 0.14 | −0.00 | 0.04 | 0.90 | −0.01 | 0.04 | 0.83 |
| Hispanic ethnicity | −0.04 | 0.04 | 0.24 | −0.02 | 0.04 | 0.50 | 0.04 | 0.04 | 0.22 |
| Perceived control | −0.14 | 0.05 | <0.01 | −0.01 | 0.04 | 0.74 | −0.07 | 0.04 | 0.14 |
Note. SE= standard error
Perceived control moderated the relationship between perceived stress and depressive symptoms (β = −.13, SE = .06, p < .05) only. Simple slopes analysis revealed that in individuals with lower (≤1 SD) perceived control, higher (≥1 SD) perceived stress was associated with more depressive symptoms [t(83) = −2.70, p < .01, d = .59; see Figure 3]. In contrast, depressive symptoms did not differ based on perceived stress level in individuals with higher (≥1 SD) perceived control. Perceived control did not moderate the association between depressive symptoms and episodic memory, or the direct effect of perceived stress on episodic memory independent of depressive symptoms.
Figure 3.
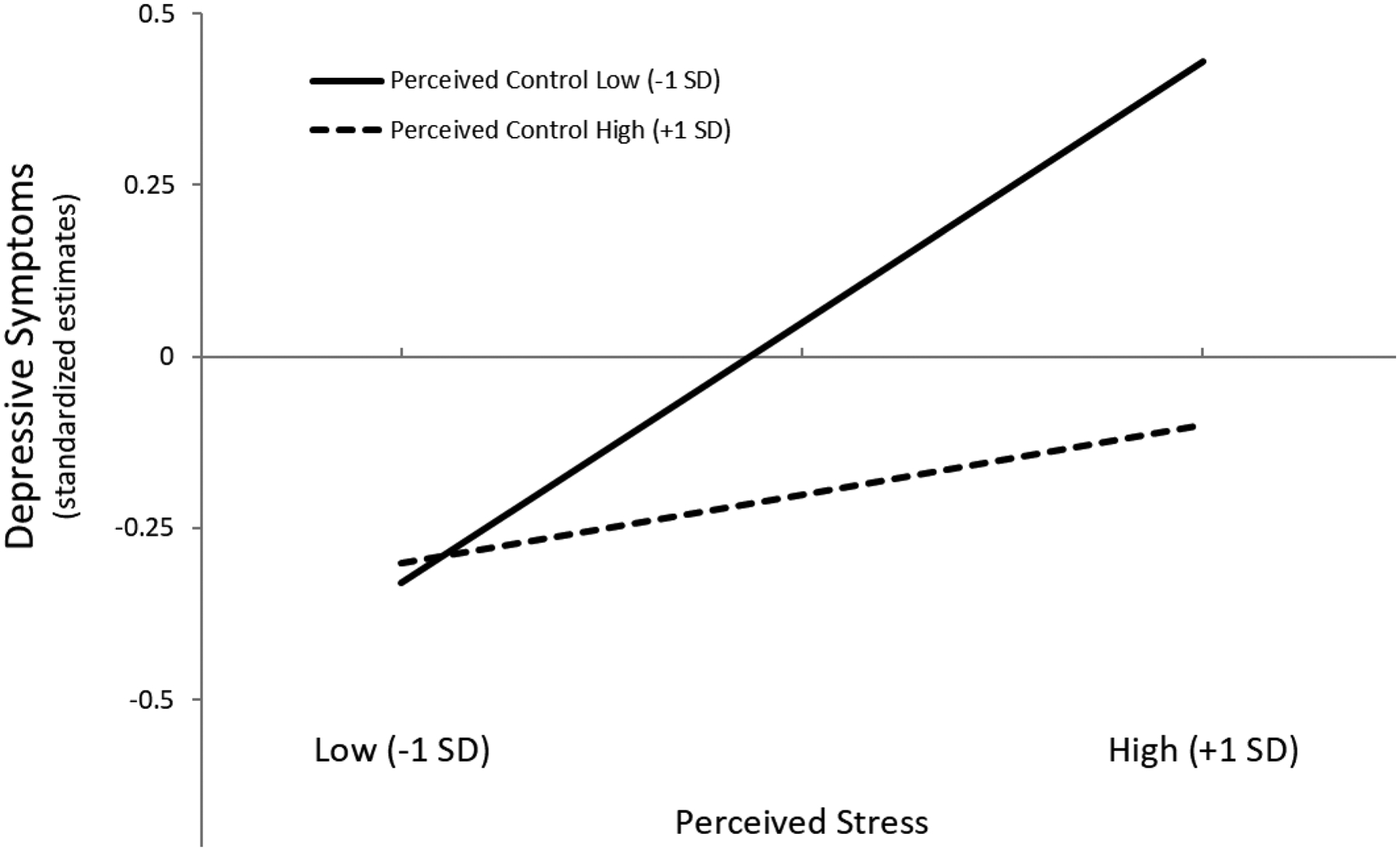
Simple slopes of perceived stress predicting depressive symptoms in individuals with low (−1 SD) versus high (+1 SD) perceived control. Estimates for depressive symptoms were adjusted for covariates. SD = standard deviation.
Discussion
In line with previous research, greater perceived stress was associated with poorer episodic memory in this cross-sectional study of diverse urban-dwelling older adults. Furthermore, this association was mediated by depressive symptoms, such that individuals with higher perceived stress also had more depressive symptoms, and those with more depressive symptoms had poorer episodic memory. Although the associations between stress, depressive symptoms, and memory were not modified by sociodemographic characteristics of gender or race/ethnicity, greater perceived control buffered the association between greater perceived stress and more depressive symptoms.
Perceived Stress, Depressive Symptoms, and Episodic Memory
The present study contributes to the growing literature suggesting that perceived stress may be a risk factor for late-life cognitive impairment and decline (Aggarwal et al., 2014; Korten, Comijs, Penninx, & Deeg, 2017; Turner, James, Capuano, Aggarwal, & Barnes, 2017) and dementia (Jiang et al., 2014). These findings may reflect detrimental effects of stress on the hippocampus, a key brain structure involved in episodic memory processes that has a high density of glucocorticoid receptors (Ohman, Nordin, Bergdahl, Slunga Birgander, & Stigsdotter Neely, 2007). Indeed, higher perceived stress has been associated with smaller hippocampal volume in a diverse sample of older adults cross-sectionally (Zimmerman et al., 2016). One proposed mechanism for the association between perceived stress and episodic memory is through neuroendocrine dysfunction and dysregulation of glucocorticoid (e.g., cortisol) secretion in response to prolonged stress. Indeed, previous research has found long-term elevation of cortisol levels to be associated with structural and functional changes in brain regions associated with various cognitive domains (Cerqueira, Mailliet, Almeida, Jay, & Sousa, 2007; Lupien, McEwen, Gunnar, & Heim, 2009; McEwen & Robinson, 2012).
Sensitivity analyses in the present study showed perceived stress was associated directly and indirectly through depressive symptoms with learning and recall, but not recognition memory. This pattern of results is consistent with prior research suggesting that depression is more strongly associated with impairments in recall than recognition memory (Brand, Jolles, & Gispen-de Wied, 1992). It may also provide further evidence for a hippocampally-mediated relationship between perceived stress and episodic memory impairment. Converging evidence from animal and human studies using neurophysiological, neuroimaging, and neuropsychological methods suggests that, compared with recall, recognition memory may rely more heavily on parahippocampal regions of the medial temporal lobe (particularly the perirhinal cortex) rather than the hippocampus, per sé (see Eichenbaum, Yonelinas, & Ranganath, 2007 for a review).
Although efforts aimed at reducing life-course exposure to stressors may protect individuals against later cognitive decline by preserving neurological and immune functioning (Graham, Christian, & Kiecolt-Glaser, 2006), this may not be an immediate practical approach. Rather, interventions aimed at improving older adults’ ability to manage stress may alleviate some of its burden on mental and cognitive health. For example, reflecting on personal values and engaging in value affirmation leads to lower cortisol response to acute stress in the laboratory among older adults (Creswell et al., 2005). Thus, while the presence of certain stressors may not be eliminated (i.e., caring for a chronically ill or disabled adult, high job-related stress), utilizing adaptive stress management techniques may lead to healthier cognitive aging.
Results from the present study also support previous work on the association between perceived stress and depressive symptoms (Kwag, Martin, Russell, Franke, & Kohut, 2011; Tsai, Chi, & Wang, 2015), as well as the association between late-life depressive symptoms and cognitive impairment and dementia (Dotson et al., 2008; Fiske, Wetherell, & Gatz, 2009; Richard et al., 2013). Stress and depressive symptoms are thought to influence late-life cognition through similar biological mechanisms, including greater HPA axis dysregulation and hippocampal atrophy (Caraci, Copani, & Nicoletti, 2010). However, results from the present study suggest that rather than operating as two separate pathways, depressive symptoms may be part of the underlying process that links experiences of stress to late-life cognitive impairment. If the presence of depressive symptoms increases risk for cognitive impairment or dementia (Cherbuin et al., 2015), then interventions aimed at reducing risk for depression or managing depressive symptoms may protect individuals living with high perceived stress against cognitive decline.
Although a sensitivity analysis revealed that the association between depressive symptoms and memory did not remain when household income was included in the model, prior research has demonstrated robust associations between late-life depressive symptoms and cognitive impairment even after accounting for confounding effects of income (Zahodne, Sol, & Kraal, 2017). Thus, we are hesitant to conclude that there is no link between depressive symptoms and memory independent of income. In the current study, the absence of a unique association between depressive symptoms and memory above and beyond income may reflect the relatively small sample size, low overall endorsement of depressive symptoms, and/or high proportion of individuals with low income. Nonetheless, income likely contributes to both depressive symptoms (Koster et al., 2006) and memory functioning (Marden, Tchetgen Tchetgen, Kawachi, & Glymour, 2017) in late life. Though it is beyond the scope of the present study, systemic interventions targeting late-life poverty as well as individual interventions aimed at increasing personal coping resources may help reduce the risk of depression among older adults. Of note, adjusting for income did not eliminate the associations between perceived stress and depressive symptoms nor the association between perceived stress and memory in the initial model that did not include depressive symptoms. Thus, early detection of the presence of depressive symptoms and interventions aimed at reducing risk for depressive symptoms among older adults may lead to healthy aging more generally (Reynolds et al., 2012).
Perceived Control
Previous research has identified perceived control as a psychosocial predictor of cognitive health among older adults (Soederberg Miller & Lachman, 1999). Although perceived control did not modify the direct effect of perceived stress on episodic memory in the present study, it did buffer the association between greater perceived stress and more depressive symptoms. This pattern of results suggests that whether an individual develops depressive symptoms when faced with stress may depend on their control beliefs.
A growing body of research suggests that individuals who perceive less control are more likely to develop depressive symptoms (Diehl & Hay, 2010; Grote et al., 2007; Johnson & Sarason, 1978). Control beliefs may influence mental health through behavioral, psychological, and biological mechanisms. It may be that individuals with low perceived control have more negative appraisals of stressful situations and/or engage in fewer adaptive or more maladaptive coping strategies when faced with stress. For example, prior research suggests individuals with lower perceived control are more likely to engage in unhealthy behaviors (i.e., smoking, over-eating) and use fewer compensatory memory strategies (Lachman, Neupert, & Agrigoroaei, 2011). In contrast, engagement in healthy behaviors, such as more physical activity, mediated the association between high perceived control and lower cognitive decline among older adults in the Health and Retirement Study (Infurna & Gerstorf, 2013). Perceiving greater control over one’s environment and life circumstances may also buffer the negative impact of stress by increasing intrinsic motivation to handle stressors in the environment. Physiologically, greater perceived control has been shown to buffer cortisol response to an acute laboratory stressor (Bollini, Walker, Hamann, & Kestler, 2004), as well as systemic inflammation in response to lifetime trauma exposure (Elliot et al., 2017).
While the current study did not find evidence that perceived control modifies the negative impact of depressive symptoms on episodic memory, previous research indicates that perceived control may act as a resource for managing cognitive difficulties associated with age-related changes in the brain. For example, greater perceived control was associated with preserved episodic memory function in the presence of lower hippocampal volume among a subset of older adults in WHICAP (Zahodne, Schupf, & Brickman, 2018). Thus, modifying control beliefs may lead to healthier cognitive aging through both effects on cognition and a more indirect pathway involving reduced risk for late-life depressive symptoms.
Sociodemographic Considerations
Although the strength of associations among perceived stress, depressive symptoms, and memory did not differ across sociodemographic characteristics in the present study, we did observe group differences in perceived stress (Matud, 2004; Meyer, Schwartz, & Frost, 2008) and episodic memory (Díaz-Venegas, Downer, Langa, & Wong, 2016) in line with prior research. While our results suggest that perceived stress and depressive symptoms have negative impacts on cognition regardless of sociodemographic identity, certain groups (i.e., women and non-Hispanic Blacks) appeared to be at greater risk for experiencing stress. This pattern of results indicates that these groups have more frequent exposure to universal stressors, exposure to stressors that are sociodemographically patterned (e.g., sexual assault, racial discrimination), and/or more negative appraisals of stressful experiences. As a result of experiencing higher levels of perceived stress, these groups may have a greater likelihood of experiencing the negative cognitive consequences associated with stress.
Additionally, depressive symptoms did not differ across sociodemographic groups in the present study despite differences in perceived stress, and women in the present study demonstrated higher memory functioning despite reporting greater perceived stress than men. These findings may reflect gender differences in coping resources (West & Simons, 1983) and suggest that the negative cognitive influence of stress also operates through mechanisms other than depression. Future research on the stress–cognition link should consider the influence of intersectionality when determining which individuals may be at heightened risk for the adverse cognitive impacts of stress. A deeper understanding of these processes may inform interventions aimed at reducing stressors at a structural level in addition to those aimed at increasing person-specific coping resources.
Limitations and Future Directions
The present study was limited to a cross-sectional design due to the relatively recent implementation of an expanded psychosocial battery in WHICAP. A future longitudinal mediation model incorporating follow-up data currently being collected would allow further understanding of associations between perceived stress, depressive symptoms, and episodic memory functioning in older adults. Furthermore, the current study relied on a single self-reported measure of stress. Although perceived stress has been shown to be a proximal indicator of the impact of chronic stressors, future research should incorporate additional measures of stress (e.g., stress biomarkers, lifetime stress exposure checklist) in addition to perceived stress in order to disentangle the effects of stress exposure from reactions to stressors. Incorporation of multiple levels of the stress experience (e.g., exposure, cognitive appraisal, physiological response) may help elucidate the mechanisms driving stress–cognition relationships.
Additionally, the present study focused on participants’ current depressive symptoms which may not be indicative of life-time presence of depression. Prior research has suggested that late-onset depression may reflect prodromal stages of dementia rather than a risk factor, per sé (Steffens, 2017). Thus, additional research is needed to investigate the longitudinal effects of clinical depression or the presence of chronic depressive symptoms throughout the life course on late-life memory trajectories. It should also be noted that the use of a single memory measure may not have captured the extent to which stress, depressive symptoms, and psychosocial or sociodemographic factors affect late-life cognition. Although the SRT taps multiple episodic memory processes and is sensitive to pre-clinical changes in cognition, future research should investigate whether perceived stress similarly influences other measures of episodic memory and other cognitive domains. Lastly, the geographic specificity of this study limits the generalizability of current findings.
Strengths of this study include its diverse sample and inclusion of relevant covariates. Furthermore, including stress and depressive symptoms together in a mediation framework allows for a deeper understanding of potential mechanisms underlying their previously documented influence on cognitive health and the identification of multiple potential points of intervention. Future intervention studies designed to reduce stress exposure, improve management of stress and depressive symptoms, and/or increase perceived control may facilitate healthy cognitive aging and aid in dementia prevention. Knowledge of these modifiable contributing factors may influence healthcare policy and encourage healthcare providers to screen for and identify stress and depression as potential risk factors for late-life cognitive impairment.
Supplementary Material
Acknowledgments
Data collection and sharing for this project was supported by the Washington Heights-Inwood Columbia Aging Project (WHICAP, PO1AG07232, R01AG037212, RF1AG054023, R01AG054520, R00AG047963) funded by the National Institute on Aging (NIA). This manuscript has been reviewed by WHICAP investigators for scientific content and consistency of data interpretation with previous WHICAP Study publications. We acknowledge the WHICAP study participants and the WHICAP research and support staff for their contributions to this study. This publication was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR001873. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The authors of this study have no conflicts of interest to declare.
References
- Aggarwal NT, Wilson RS, Beck TL, Rajan KB, Mendes de Leon CF, Evans DA, & Everson-Rose SA (2014). Perceived stress and change in cognitive function among adults 65 years and older. Psychosomatic Medicine, 76(1), 80–85. 10.1097/PSY.0000000000000016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer’s Disease Facts and Figures. (2019). Alzheimer’s & Dementia, 321–387. Retrieved from https://www.alz.org/media/Documents/alzheimers-facts-and-figures-2019-r.pdf [Google Scholar]
- Bäckman L, Small BJ, & Fratiglioni L (2001). Stability of the preclinical episodic memory deficit in Alzheimer’s disease. Brain : A Journal of Neurology, 124(Pt 1), 96–102. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11133790 [DOI] [PubMed] [Google Scholar]
- Barbosa-Leiker C, Kostick M, Lei M, McPherson S, Roper V, Hoekstra T, & Wright B (2013). Measurement Invariance of the Perceived Stress Scale and Latent Mean Differences across Gender and Time. Stress and Health, 29(3), 253–260. 10.1002/smi.2463 [DOI] [PubMed] [Google Scholar]
- Bollini AM, Walker EF, Hamann S, & Kestler L (2004). The influence of perceived control and locus of control on the cortisol and subjective responses to stress. Biological Psychology. 10.1016/j.biopsycho.2003.11.002 [DOI] [PubMed] [Google Scholar]
- Boraxbekk C-J, Lundquist A, Nordin A, Nyberg L, Nilsson L-G, & Adolfsson R (2015). Free Recall Episodic Memory Performance Predicts Dementia Ten Years prior to Clinical Diagnosis: Findings from the Betula Longitudinal Study. Dementia and Geriatric Cognitive Disorders Extra. 10.1159/000381535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand AN, Jolles J, & Gispen-de Wied C (1992). Recall and recognition memory deficits in depression. Journal of Affective Disorders, 25(1), 77–86. 10.1016/0165-0327(92)90095-N [DOI] [PubMed] [Google Scholar]
- Buschke H, & Fuld PA (1974). Evaluating storage, retention, and retrieval in disordered memory and learning. Neurology, 24(11), 1019–1025. 10.1212/WNL.24.11.1019 [DOI] [PubMed] [Google Scholar]
- Caraci F, Copani A, & Nicoletti F (2010). Depression and Alzheimer’s disease: Neurobiological links and common pharmacological targets. European Journal of Pharmacology, 626(1), 64–71. 10.1016/J.EJPHAR.2009.10.022 [DOI] [PubMed] [Google Scholar]
- Carter CL, Resnick EM, Mallampalli M, & Kalbarczyk A (2012). Sex and Gender Differences in Alzheimer’s Disease: Recommendations for Future Research. Journal of Women’s Health, 21(10), 1018–1023. 10.1089/jwh.2012.3789 [DOI] [PubMed] [Google Scholar]
- Cerqueira JJ, Mailliet F, Almeida OFX, Jay TM, & Sousa N (2007). The prefrontal cortex as a key target of the maladaptive response to stress. The Journal of Neuroscience : The Official Journal of the Society for Neuroscience, 27(11), 2781–2787. 10.1523/JNEUROSCI.4372-06.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherbuin N, Kim S, & Anstey KJ (2015). Dementia risk estimates associated with measures of depression: a systematic review and meta-analysis. 10.1136/bmjopen-2015 [DOI] [PMC free article] [PubMed]
- Chipperfield JG, Campbell DW, & Perry RP (2004). Stability in Perceived Control. Journal of Aging and Health, 16(1), 116–147. 10.1177/0898264303260447 [DOI] [PubMed] [Google Scholar]
- Cohen S, Kessler RC, & Gordon LU (Eds.). (1997). Measuring Stress: A Guide for Health and Social Scientists. Oxford University Press on Demand. Retrieved from https://books.google.com/books?hl=en&lr=&id=o8znCwAAQBAJ&oi=fnd&pg=PR9&ots=aJCh682ubo&sig=k1T2c2MOpE_2EpHhAyxjrpmfbdM#v=onepage&q&f=false [Google Scholar]
- Cohen Sheldon, Janicki-Deverts D, & Miller GE (2007). Psychological Stress and Disease. JAMA, 298(14), 1685. 10.1001/jama.298.14.1685 [DOI] [PubMed] [Google Scholar]
- Cohen Sheldon, Kamarck T, & Mermelstein R (1983). A Global Measure of Perceived Stress. Source Journal of Health and Social Behavior, 24(4), 385–396. Retrieved from http://www.jstor.org/stable/2136404 [PubMed] [Google Scholar]
- Creswell JD, Welch WT, Taylor SE, Sherman DK, Gruenewald TL, & Mann T (2005). Affirmation of Personal Values Buffers Neuroendocrine and Psychological Stress Responses. Psychological Science, 16(11), 846–851. 10.1111/j.1467-9280.2005.01624.x [DOI] [PubMed] [Google Scholar]
- Cummins RC (1988). Perceptions of social support, receipt of supportive behaviors, and locus of control as moderators of the effects of chronic stress. American Journal of Community Psychology, 16(5), 685–700. 10.1007/BF00930021 [DOI] [PubMed] [Google Scholar]
- Dedovic K, Duchesne A, Andrews J, Engert V, & Pruessner JC (2009). The brain and the stress axis: The neural correlates of cortisol regulation in response to stress. NeuroImage, 47(3), 864–871. 10.1016/J.NEUROIMAGE.2009.05.074 [DOI] [PubMed] [Google Scholar]
- Díaz-Venegas C, Downer B, Langa KM, & Wong R (2016). Racial and ethnic differences in cognitive function among older adults in the USA. International Journal of Geriatric Psychiatry, 31(9), 1004–1012. 10.1002/gps.4410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson WJ, Potter GG, Hybels CF, McQuoid DR, & Steffens DC (2011). Change in stress and social support as predictors of cognitive decline in older adults with and without depression. International Journal of Geriatric Psychiatry, 26(12), 1267–1274. 10.1002/gps.2676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diehl M, & Hay EL (2010). Risk and resilience factors in coping with daily stress in adulthood: the role of age, self-concept incoherence, and personal control. Developmental Psychology, 46(5), 1132–1146. 10.1037/a0019937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dotson VM, Resnick SM, & Zonderman AB (2008). Differential Association of Concurrent, Baseline, and Average Depressive Symptoms With Cognitive Decline in Older Adults. The American Journal of Geriatric Psychiatry, 16(4), 318–330. 10.1097/JGP.0B013E3181662A9C [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichenbaum H, Yonelinas AP, & Ranganath C (2007). The Medial Temporal Lobe and Recognition Memory. Annual Review of Neuroscience, 30(1), 123–152. 10.1146/annurev.neuro.30.051606.094328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot AJ, Mooney CJ, Infurna FJ, & Chapman BP (2017). Associations of Lifetime Trauma and Chronic Stress With C-reactive Protein in Adults Ages 50 Years and Older. Psychosomatic Medicine, 79(6), 622–630. 10.1097/PSY.0000000000000476 [DOI] [PubMed] [Google Scholar]
- Epel ES, Lin J, Wilhelm FH, Wolkowitz OM, Cawthon R, Adler NE, … Blackburn EH (2006). Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinology, 31(3), 277–287. 10.1016/J.PSYNEUEN.2005.08.011 [DOI] [PubMed] [Google Scholar]
- Ezzati A, Jiang J, Katz MJ, Sliwinski MJ, Zimmerman ME, & Lipton RB (2014). Validation of the Perceived Stress Scale in a community sample of older adults. International Journal of Geriatric Psychiatry, 29(6), 645–652. 10.1002/gps.4049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske A, Wetherell JL, & Gatz M (2009). Depression in Older Adults. Annual Review of Clinical Psychology, 5(1), 363–389. 10.1146/annurev.clinpsy.032408.153621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garson GD (2012). Testing Statistical Assumptions. Asheboro, NC. Retrieved from; www.statisticalassociates.com [Google Scholar]
- George LK, & Lynch SM (2003). Race Differences in Depressive Symptoms: A Dynamic Perspective on Stress Exposure and Vulnerability. Journal of Health and Social Behavior, 44(3), 353. 10.2307/1519784 [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Heckhausen J, Ram N, Infurna FJ, Schupp J, & Wagner GG (2014). Perceived personal control buffers terminal decline in well-being. Psychology and Aging, 29(3), 612–625. 10.1037/a0037227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golding JM, & Burnam MA (1990). Stress and social support as predictors of depressive symptoms in Mexican Americans and non-Hispanic Whites. Journal of Social and Clinical Psychology, 9(2), 268–287. 10.1521/jscp.1990.9.2.268 [DOI] [Google Scholar]
- González P, Nuñez A, Merz E, Brintz C, Weitzman O, Navas EL, … Gallo LC (2017). Measurement properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): Findings from HCHS/SOL. Psychological Assessment, 29(4), 372–381. 10.1037/pas0000330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gouin J-P, Hantsoo L, & Kiecolt-Glaser JK (2008). Immune dysregulation and chronic stress among older adults: a review. Neuroimmunomodulation, 15(4–6), 251–259. 10.1159/000156468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gourounti K, Anagnostopoulos F, Potamianos G, Lykeridou K, Schmidt L, & Vaslamatzis G (2012). Perception of control, coping and psychological stress of infertile women undergoing IVF. Reproductive BioMedicine Online, 24(6), 670–679. 10.1016/J.RBMO.2012.03.002 [DOI] [PubMed] [Google Scholar]
- Graham JE, Christian LM, & Kiecolt-Glaser JK (2006). Stress, Age, and Immune Function: Toward a Lifespan Approach. Journal of Behavioral Medicine, 29(4), 389–400. 10.1007/s10865-006-9057-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Bledsoe SE, Larkin J, Lemay EP, & Brown C (2007). Stress Exposure and Depression in Disadvantaged Women: The Protective Effects of Optimism and Perceived Control. Social Work Research, 31(1), 19–33. 10.1093/swr/31.1.19 [DOI] [Google Scholar]
- Hammen C, Kim EY, Eberhart NK, & Brennan PA (2009). Chronic and acute stress and the prediction of major depression in women. Depression and Anxiety, 26(8), 718–723. 10.1002/da.20571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis: A regression-based approach (2nd ed.). Gilford Publications. [Google Scholar]
- Infurna FJ, & Gerstorf D (2013). Linking perceived control, physical activity, and biological health to memory change. Psychology and Aging. 10.1037/a0033327 [DOI] [PubMed] [Google Scholar]
- Irwin M, Artin KH, & Oxman MN (1999). Screening for Depression in the Older Adult: Criterion Validity of the 10-Item Center for Epidemiological Studies Depression Scale (CES-D). Archives of Internal Medicine, 159(15), 1701. 10.1001/archinte.159.15.1701 [DOI] [PubMed] [Google Scholar]
- Jiang J, Katz MJ, White R, Zimmerman ME, Sliwinski M, Kim M, & Lipton RB (2014). PERCEIVED STRESS AND RISK OF DEMENTIA IN OLDER ADULTS WITH AMNESTIC MILD COGNITIVE IMPAIRMENT. Alzheimer’s & Dementia, 10(4), P594. 10.1016/j.jalz.2014.05.993 [DOI] [Google Scholar]
- Johnson JH, & Sarason IG (1978). Life stress, depression and anxiety: Internal- external control as a moderator variable. Journal of Psychosomatic Research, 22(3), 205–208. 10.1016/0022-3999(78)90025-9 [DOI] [PubMed] [Google Scholar]
- Juster R-P, McEwen BS, & Lupien SJ (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews, 35(1), 2–16. 10.1016/J.NEUBIOREV.2009.10.002 [DOI] [PubMed] [Google Scholar]
- Justice NJ (2018). The relationship between stress and Alzheimer’s disease. Neurobiology of Stress, 8, 127–133. 10.1016/J.YNSTR.2018.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC (2003). Epidemiology of women and depression. Journal of Affective Disorders, 74(1), 5–13. 10.1016/S0165-0327(02)00426-3 [DOI] [PubMed] [Google Scholar]
- Kornstein SG (2002). Chronic Depression in Women. The Journal of Clinical Psychiatry, 63(7), 602–609. 10.4088/JCP.v63n0713 [DOI] [PubMed] [Google Scholar]
- Korten NCM, Comijs HC, Penninx BWJH, & Deeg DJH (2017). Perceived stress and cognitive function in older adults: which aspect of perceived stress is important? International Journal of Geriatric Psychiatry, 32(4), 439–445. 10.1002/gps.4486 [DOI] [PubMed] [Google Scholar]
- Koster A, Bosma H, Kempen GIJM, Penninx BWJH, Beekman ATF, Deeg DJH, & van Eijk JTM (2006). Socioeconomic differences in incident depression in older adults: The role of psychosocial factors, physical health status, and behavioral factors. Journal of Psychosomatic Research, 61(5), 619–627. 10.1016/j.jpsychores.2006.05.009 [DOI] [PubMed] [Google Scholar]
- Krause N (1986). Stress and Sex Differences in Depressive Symptoms Among Older Adults. Journal of Gerontology, 41(6), 727–731. 10.1093/geronj/41.6.727 [DOI] [PubMed] [Google Scholar]
- Kupst MJ, Butt Z, Stoney CM, Griffith JW, Salsman JM, Folkman S, & Cella D (2015). Assessment of stress and self-efficacy for the NIH Toolbox for Neurological and Behavioral Function. Anxiety, Stress, & Coping, 28(5), 531–544. 10.1080/10615806.2014.994204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwag KH, Martin P, Russell D, Franke W, & Kohut M (2011). The impact of perceived stress, social support, and home-based physical activity on mental health among older adults. International Journal of Aging & Human Development, 72(2), 137–154. 10.2190/AG.72.2.c [DOI] [PubMed] [Google Scholar]
- Lachman ME, & Andreoletti C (2006). Strategy Use Mediates the Relationship Between Control Beliefs and Memory Performance for Middle-Aged and Older Adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 61(2), P88–P94. 10.1093/geronb/61.2.P88 [DOI] [PubMed] [Google Scholar]
- Lachman Margie E. (2006). Perceived control over aging-related declines: Adaptive beliefs and behaviors. Current Directions in Psychological Science. 10.1111/j.1467-8721.2006.00453.x [DOI] [Google Scholar]
- Lachman Margie E., & Weaver SL (1998). The Sense of Control as a Moderator of Social Class Differences in Health and Well-Being. Journal of Personality and Social Psychology. 10.1037/0022-3514.74.3.763 [DOI] [PubMed] [Google Scholar]
- Lachman Margie E, Neupert SD, & Agrigoroaei S (2011). Chapter 11 - The Relevance of Control Beliefs for Health and Aging. In Handbook of the Psychology of Aging (Seventh Edition). 10.1016/B978-0-12-380882-0.00011-5 [DOI] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, & Heim C (2009). Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience, 10(6), 434–445. 10.1038/nrn2639 [DOI] [PubMed] [Google Scholar]
- Machado A, Herrera AJ, De Pablos RM, Espinosa-Oliva AM, Sarmiento M, Ayala A, … Cano J (2014). Chronic stress as a risk factor for Alzheimer’s disease. Reviews in the Neurosciences. 10.1515/revneuro-2014-0035 [DOI] [PubMed] [Google Scholar]
- Manly JJ, Bell-McGinty S, Tang M-X, Schupf N, Stern Y, & Mayeux R (2005). Implementing Diagnostic Criteria and Estimating Frequency of Mild Cognitive Impairment in an Urban Community. Archives of Neurology, 62(11), 1739. 10.1001/archneur.62.11.1739 [DOI] [PubMed] [Google Scholar]
- Marden JR, Tchetgen Tchetgen EJ, Kawachi I, & Glymour MM (2017). Contribution of Socioeconomic Status at 3 Life-Course Periods to Late-Life Memory Function and Decline: Early and Late Predictors of Dementia Risk. In American Journal of Epidemiology (Vol. 186, pp. 805–814). Oxford University Press. 10.1093/aje/kwx155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masur DM, Fuld PA, Blau AD, Thal LJ, Levin HS, & Aronson MK (1989). Distinguishing normal and demented elderly with the selective reminding test. Journal of Clinical and Experimental Neuropsychology, 11(5), 615–630. 10.1080/01688638908400920 [DOI] [PubMed] [Google Scholar]
- Matud MP (2004). Gender differences in stress and coping styles. Personality and Individual Differences, 37(7), 1401–1415. 10.1016/J.PAID.2004.01.010 [DOI] [Google Scholar]
- Mayeda ER, Glymour MM, Quesenberry CP, & Whitmer RA (2016). Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimer’s and Dementia. 10.1016/j.jalz.2015.12.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcewen BS, & Robinson GE (2012). Brain on stress: How the social environment gets under the skin. Proc Natl Acad Sci PNAS, 109(4), 17180–17185. Retrieved from 10.1073/pnas.1221399110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, & Sapolsky RM (1995). Stress and cognitive function. Current Opinion in Neurobiology, 5(2), 205–216. 10.1016/0959-4388(95)80028-X [DOI] [PubMed] [Google Scholar]
- Meyer IH, Schwartz S, & Frost DM (2008). Social patterning of stress and coping: Does disadvantaged social statuses confer more stress and fewer coping resources? Social Science and Medicine, 67(3), 368–379. 10.1016/j.socscimed.2008.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munoz E, Sliwinski MJ, Scott SB, & Hofer S (2015). Global perceived stress predicts cognitive change among older adults. Psychology and Aging, 30(3), 487–499. 10.1037/pag0000036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Shea DM, Fieo RA, Hamilton JL, Zahodne LB, Manly JJ, & Stern Y (2015). Examining the association between late-life depressive symptoms, cognitive function, and brain volumes in the context of cognitive reserve. International Journal of Geriatric Psychiatry, 30(6), 614–622. 10.1002/gps.4192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohman L, Nordin S, Bergdahl J, Slunga Birgander L, & Stigsdotter Neely A (2007). Cognitive function in outpatients with perceived chronic stress. Scandinavian Journal of Work, Environment & Health, 33(3), 223–232. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17572832 [DOI] [PubMed] [Google Scholar]
- Peavy GM, Salmon DP, Jacobson MW, Hervey A, Gamst AC, Wolfson T, … Galasko D (2009). Effects of Chronic Stress on Memory Decline in Cognitively Normal and Mildly Impaired Older Adults. American Journal of Psychiatry, 166(12), 1384–1391. 10.1176/appi.ajp.2009.09040461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera MJ, Brintz CE, Birnbaum-Weitzman O, Penedo FJ, Gallo LC, Gonzalez P, … Llabre MM (2017). Factor structure of the perceived stress scale-10 (PSS) across english and Spanish language responders in the HCHS/SOL sociocultural ancillary study. Psychological Assessment, 29(3), 320–328. 10.1037/pas0000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podcasy JL, & Epperson CN (2016). Considering sex and gender in Alzheimer disease and other dementias. Dialogues in Clinical Neuroscience, 18(4), 437–446. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/28179815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds CF, Cuijpers P, Patel V, Cohen A, Dias A, Chowdhary N, … Albert SM (2012). Early Intervention to Reduce the Global Health and Economic Burden of Major Depression in Older Adults. Annual Review of Public Health, 33(1), 123–135. 10.1146/annurev-publhealth-031811-124544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard E, Reitz C, Honig LH, Schupf N, Tang MX, Manly JJ, … Luchsinger JA (2013). Late-Life Depression, Mild Cognitive Impairment, and Dementia. JAMA Neurology, 70(3), 383. 10.1001/jamaneurol.2013.603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickenbach EH, Almeida DM, Seeman TE, & Lachman ME (2014). Daily stress magnifies the association between cognitive decline and everyday memory problems: An integration of longitudinal and diary methods. Psychology and Aging, 29(4), 852–862. 10.1037/a0038072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salgado de Snyder VN, Cervantes RC, & Padilla AM (1990). Gender and ethnic differences in psychosocial stress and generalized distress among Hispanics. Sex Roles, 22(7–8), 441–453. 10.1007/BF00288163 [DOI] [Google Scholar]
- Salsman JM, Butt Z, Pilkonis PA, Cyranowski JM, Zill N, Hendrie HC, … Cella D (2013). Emotion assessment using the NIH Toolbox. Neurology, 80(11 Suppl 3), S76–86. 10.1212/WNL.0b013e3182872e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuey KM, & Willson AE (2008). Cumulative Disadvantage and Black-White Disparities in Life-Course Health Trajectories. Research on Aging, 30(2), 200–225. 10.1177/0164027507311151 [DOI] [Google Scholar]
- Siedlecki KL, Manly JJ, Brickman AM, Schupf N, Tang M-X, & Stern Y (2010). Do neuropsychological tests have the same meaning in Spanish speakers as they do in English speakers? Neuropsychology, 24(3), 402–411. 10.1037/a0017515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soederberg Miller LM, & Lachman ME (1999). The Sense of Control and Cognitive Aging: Toward a Model of Mediational Processes. Social Cognition and Aging, 17–41. 10.1016/B978-012345260-3/50003-3 [DOI] [Google Scholar]
- Stawski RS, Sliwinski MJ, Almeida DM, & Smyth JM (2008). Reported exposure and emotional reactivity to daily stressors: The roles of adult age and global perceived stress. Psychology and Aging, 23(1), 52–61. 10.1037/0882-7974.23.1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffens DC (2017, July 1). Late-life depression and the prodromes of dementia. JAMA Psychiatry. American Medical Association. 10.1001/jamapsychiatry.2017.0658 [DOI] [PubMed] [Google Scholar]
- Tafet GE, & Bernardini R (2003). Psychoneuroendocrinological links between chronic stress and depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 27(6), 893–903. 10.1016/S0278-5846(03)00162-3 [DOI] [PubMed] [Google Scholar]
- Tang MX, Cross P, Andrews H, Jacobs DM, Small S, Bell K, … Mayeux R (2001). Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology, 56(1), 49–56. 10.1212/WNL.56.1.49 [DOI] [PubMed] [Google Scholar]
- Tsai AC, Chi S-H, & Wang J-Y (2015). Association of perceived stress with depressive symptoms in older Taiwanese: Results of a population-based study. Geriatrics & Gerontology International, 15(5), 535–543. 10.1111/ggi.12307 [DOI] [PubMed] [Google Scholar]
- Turner AD, James BD, Capuano AW, Aggarwal NT, & Barnes LL (2017). Perceived Stress and Cognitive Decline in Different Cognitive Domains in a Cohort of Older African Americans. The American Journal of Geriatric Psychiatry, 25(1), 25–34. 10.1016/j.jagp.2016.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, & Avison WR (2003). Status Variations in Stress Exposure: Implications for the Interpretation of Research on Race, Socioeconomic Status, and Gender. Journal of Health and Social Behavior, 44(4), 488. 10.2307/1519795 [DOI] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, & Herzog R (1999). A Revised CES-D Measure of Depressive Symptoms and a DSM-Based Measure of Major Depressive Episodes in the Elderly. International Psychogeriatrics, 11(2), 139–148. 10.1017/S1041610299005694 [DOI] [PubMed] [Google Scholar]
- Ulbrich PM, Warheit GJ, & Zimmerman RS (1989). Race, Socioeconomic Status, and Psychological Distress: An Examination of Differential Vulnerability. Journal of Health and Social Behavior, 30(1), 131. 10.2307/2136918 [DOI] [PubMed] [Google Scholar]
- Verma R, Balhara YPS, & Gupta CS (2011). Gender differences in stress response: Role of developmental and biological determinants. Industrial Psychiatry Journal, 20(1), 4–10. 10.4103/0972-6748.98407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vines AI, Ta M, Esserman D, & Baird DD (2009). A Comparison of the Occurrence and Perceived Stress of Major Life Events in Black and White Women. Women & Health, 49(5), 368–380. 10.1080/03630240903238743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- VonDras DD, Powless MR, Olson AK, Wheeler D, & Snudden AL (2005). Differential effects of everyday stress on the episodic memory test performances of young, mid-life, and older adults. Aging & Mental Health, 9(1), 60–70. 10.1080/13607860412331323782 [DOI] [PubMed] [Google Scholar]
- Wallston KA, Wallston BS, Smith S, & Dobbins CJ (1987). Perceived control and health. Current Psychology, 6(1), 5–25. 10.1007/BF02686633 [DOI] [Google Scholar]
- West GE, & Simons RL (1983). Sex Differences in Stress, Coping Resources, and Illness among the Elderly. Research on Aging, 5(2), 235–268. 10.1177/0164027583005002006 [DOI] [Google Scholar]
- Williams DR, González HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, & Jackson JS (2007). Prevalence and Distribution of Major Depressive Disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites. Archives of General Psychiatry, 64(3), 305. 10.1001/archpsyc.64.3.305 [DOI] [PubMed] [Google Scholar]
- Williams DR, Yan Yu Y, Jackson JS, & Anderson NB (1997). Racial Differences in Physical and Mental Health. Journal of Health Psychology, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- Windsor TD, & Anstey KJ (2008). A Longitudinal Investigation of Perceived Control and Cognitive Performance in Young, Midlife and Older Adults. Aging, Neuropsychology, and Cognition, 15(6), 744–763. 10.1080/13825580802348570 [DOI] [PubMed] [Google Scholar]
- Zahodne LB, Nowinski CJ, Gershon RC, & Manly JJ (2014). Depressive Symptoms Are More Strongly Related to Executive Functioning and Episodic Memory Among African American compared with Non-Hispanic White Older Adults. Archives of Clinical Neuropsychology, 29(7), 663–669. 10.1093/arclin/acu045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne Laura B., Schupf N, & Brickman AM (2018). Control beliefs are associated with preserved memory function in the face of low hippocampal volume among diverse older adults. Brain Imaging and Behavior, 12(4), 1112–1120. 10.1007/s11682-017-9776-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne Laura B., Stern Y, & Manly JJ (2014). Depressive symptoms precede memory decline, but not vice versa, in non-demented older adults. Journal of the American Geriatrics Society. 10.1111/jgs.12600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne Laura B., Watson CWM, Seehra S, & Martinez MN (2017). Positive Psychosocial Factors and Cognition in Ethnically Diverse Older Adults. Journal of the International Neuropsychological Society, 24, 294–304. 10.1017/S1355617717000935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahodne Laura B, Sol K, & Kraal Z (2017). Psychosocial Pathways to Racial/Ethnic Inequalities in Late-Life Memory Trajectories. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 10.1093/geronb/gbx113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman ME, Ezzati A, Katz MJ, Lipton ML, Brickman AM, Sliwinski MJ, & Lipton RB (2016). Perceived Stress Is Differentially Related to Hippocampal Subfield Volumes among Older Adults. PLOS ONE, 11(5), e0154530. 10.1371/journal.pone.0154530 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


