Abstract
Objective
To describe baseline technology use within the head and neck cancer (HNC) population prior to the COVID-19 pandemic.
Study Design
Cross-sectional analysis of National Health Interview Survey (NHIS) data.
Setting
The NHIS is a survey of population health administered in person annually to a nationally representative sample of noninstitutionalized US residents via a complex clustered sampling design.
Methods
Data regarding technology use, cancer history, and demographics were extracted from the NHIS. The study population comprised individuals who completed the NHIS Sample Adult survey from 2012 to 2018 and self-reported a cancer diagnosis. Poisson regression was used to evaluate associations between demographics and general or health-related technology use and prevalence ratios reported.
Results
Patients with HNC were less likely to use general technology (computers, internet, or email) when compared with other patients with cancer (60% vs 73%, P < .001), although this difference was not statistically significant after controlling for sociodemographic factors. Among patients with HNC, older age, lower education, and lower income were negatively associated with general technology use (adjusted prevalence ratio [aPR], 0.71 [95% CI, 0.59-0.87] for age 65-79 years vs <50 years; aPR, 0.66 [95% CI, 0.51-0.85] for high school vs master; aPR, 0.66 [95% CI, 0.48-0.91] for income 100%-200% vs >400% federal poverty level). Older age and lower education were negatively associated with health-related technology use (aPR, 0.46 [95% CI, 0.32-0.67] for age 65-79 years vs <50 years; aPR, 0.47 [95% CI, 0.30-0.74] for high school vs master).
Conclusion
Socioeconomic disparities exist in technology use rates among patients with HNC. Access to technology may pose a barrier to telehealth visits for many patients with HNC due to the unique socioeconomic demographics of this patient population.
Keywords: head and neck cancer, technology, telemedicine, telehealth, COVID-19, coronavirus, disparities, health disparities, socioeconomic
Clinicians have come to increasingly rely on technology to connect with patients during the COVID-19 pandemic. Telehealth visits are becoming a common substitute for in-person visits due to concerns about transmission of COVID-19 in the hospital or clinic setting. 1 In the head and neck cancer (HNC) population, many providers have opted to conduct appointments with patients via videoconferencing. Postoperative visits, oncologic surveillance, and monitoring of radiotherapy are some situations in which telehealth may be considered an appropriate alternative to an in-person visit.2,3 Additionally, some clinicians are using telehealth to guide patients through simple procedures, such as drain removal. 4 As the COVID-19 pandemic evolves and ends, it seems likely that telehealth will continue to be a standard part of practice in head and neck oncology. 5
Patients with HNC represent a socioeconomically vulnerable patient population as they are, on average, older and less educated and have lower incomes than the general population.6-8 For this reason, concerns have been raised over potential disparities in telehealth access among these patients. 9 Individual reports have already described instances in which socioeconomic barriers have limited patient engagement in telehealth encounters during the COVID-19 pandemic. 10 However, no study has yet quantitatively examined technology access and use within the HNC population.
By using nationally representative data from the National Health Interview Survey (NHIS), the aims of this study were to describe baseline patterns of technology use within the HNC population prior to the COVID-19 pandemic and to identify vulnerable subpopulations who may be less likely to benefit from telehealth visits. We hypothesized that patients with HNC have a lower prevalence of technology utilization when compared with other patients with cancer and that certain demographics factors may be associated with less technology use. Understanding technology use within this population will enable clinicians to better serve the needs of these patients as telehealth is increasingly incorporated into oncology practices during the COVID-19 pandemic and beyond.
Methods
NHIS Data Set
Beginning in 1957, the NHIS is a cross-sectional survey of population health administered annually by the Centers for Disease Control and Prevention to a nationally representative sample of noninstitutionalized US residents. 11 The NHIS is administered in person by trained interviewers to households selected through a complex clustered sampling design. The Centers for Disease Control and Prevention keeps comprehensive records of survey procedures, definitions, and data, which are stored as a harmonized data set by IPUMS, a service created by the Institute for Social Research and Data Innovation at University of Minnesota to facilitate use of freely available survey and census data. 12
The Sample Adult survey is administered to a randomly selected adult within each surveyed household, and it collects details of health behaviors and medical history, including cancer diagnoses. Respondents are asked whether they use computers, internet, or email and whether they use internet-based technology for health-related purposes.
For this analysis, the study population was limited to individuals who completed the NHIS Sample Adult survey between 2012 and 2018 (when technology-related data were available) and self-reported a cancer diagnosis. Those who self-reported a diagnosis of laryngeal, pharyngeal, or oral cavity cancer were categorized as patients with HNC. Those who self-reported any other cancer diagnosis were categorized as other patients with cancer. Demographic data were extracted regarding age, race, ethnicity, sex, education, region of residence, health insurance, and ratio of income to federal poverty level (FPL). Race was categorized as a binary variable describing respondents as non-Hispanic White or other race. Age was binned to enable comparison across age groups.
Data related to respondents’ technology use in general and in relation to health were additionally extracted. General technology use data included the following: (1) frequency of computer use, dichotomized as “not computer users” for survey respondents who answered never or almost never and “computer users” for those who answered some days, most days, or every day, and (2) binary questions (yes/no) about internet and email use. A composite variable was created to represent use of any general technology. Health technology use data included binary answers (yes/no) to the following questions: “During the past year, have you used computers to look up health information on the internet?”“During the past year, have you used the internet to schedule healthcare appointments?” and “During the past year, have you used email to communicate with providers?” A second composite variable was created to represent use of any health-related technology.
Because this study used publicly available deidentified data, approval was not required by the Mass General Brigham Institutional Review Board.
Statistical Methods
Individual responses to questions from the NHIS data from 2012 to 2018 were obtained and merged via IPUMS. For statistical analysis, data were imported from IPUMS into R (version 3.6.1) on RStudio (version 1.2.1335) via the ipumsr package (version 0.4.3). Sampling weights provided by the NHIS, which account for stratification, clustering, and oversampling procedures, were used to produce estimates representative of the US population. 11 Analysis was carried out with the survey package (version 4.0) in R, which allows for incorporation of sampling weights and analysis of complex survey designs. Chi-square statistical tests were used to generate P values for demographic and technology use differences between the HNC and other cancer populations. Univariate Poisson regressions with robust standard errors were run to generate prevalence ratios (PRs) and evaluate the relationship between the outcome variables of general and health-related technology use and the independent variables age, sex, race, education, income, region, and health insurance status. Multivariable Poisson regressions were used to determine which variables were independently associated with technology use. Multivariable models include variables that were statistically significant in the univariate analysis. Imputation of missing data was performed through the MICE statistical package in R. For robustness, all statistical tests were run with imputed and ignored missing values. The outcomes of the analysis were not affected by imputation. Nonimputed values are reported in this article. Statistical significance was considered at P < .05.
Results
Study Population
The unweighted sample of persons surveyed by the NHIS from 2012 to 2018 who had a self-reported cancer diagnosis was 22,644, representing a total weighted sample of 21,582,841 ( Table 1 ). Patients with HNC accounted for 381 in the unweighted sample, representing 368,248 in the weighted sample.
Table 1.
Demographics of Surveyed Patients With Cancer.
| Head and neck cancer | Other cancer | ||||
|---|---|---|---|---|---|
| No. a | % b | No. a | % b | P value | |
| Total | 381 | 100 | 22,263 | 100 | |
| Sex | <.001 c | ||||
| Male | 251 | 69 | 9025 | 43 | |
| Female | 130 | 31 | 13,238 | 57 | |
| Age, y | .78 | ||||
| <50 | 46 | 14 | 2805 | 15 | |
| 50-64 | 115 | 31 | 6316 | 32 | |
| 65-79 | 163 | 40 | 9063 | 38 | |
| ≥80 | 57 | 15 | 4079 | 15 | |
| Race | .03 d | ||||
| White | 303 | 79 | 18,637 | 85 | |
| Other race | 78 | 21 | 3546 | 15 | |
| Education | .008 e | ||||
| <High school | 77 | 19 | 2807 | 11 | |
| High school | 113 | 29 | 5688 | 25 | |
| Some college | 100 | 28 | 6727 | 30 | |
| Bachelor | 58 | 16 | 3998 | 19 | |
| Master | 31 | 8 | 2967 | 14 | |
| Income as % FPL | <.001 c | ||||
| ≥400 | 139 | 40 | 10,667 | 55 | |
| 300 to <400 | 37 | 11 | 2277 | 10 | |
| 200 to <300 | 55 | 15 | 3098 | 13 | |
| 100 to <200 | 91 | 22 | 3882 | 15 | |
| <100 | 55 | 12 | 2118 | 7 | |
| Region | .91 | ||||
| Northeast | 66 | 21 | 3847 | 18 | |
| Midwest | 83 | 22 | 5149 | 23 | |
| South | 150 | 36 | 7825 | 37 | |
| West | 82 | 22 | 5442 | 21 | |
| Health insurance | .03 d | ||||
| Public | 91 | 46 | 6149 | 35 | |
| Private | 96 | 54 | 9631 | 65 | |
Abbreviation: FPL, federal poverty level.
Unweighted number of survey respondents.
Weighted percentages.
P < .001.
P < .05.
P < .01.
Patients with HNC differed significantly from the remainder of the oncology population with respect to demographic characteristics ( Table 1 ). Patients with HNC were more likely to be male (69% vs 43%, P < .001) and non-White (21% vs 15%, P = .03) and less likely to have private health insurance (54% vs 65%, P = .03) than patients with other types of cancer. They also had lower incomes (P < .001) and lower educational attainment (P = .008). These results are consistent with other epidemiologic studies of the HNC population.6-8
Cancer and Technology Use
Patients with HNC were less likely to report use of general technology, such as computers, internet, and email, than patients with other cancers ( Figure 1 ). Merely 60% indicated any general technology use, as opposed to 73% of other patients with cancer (P < .001). In addition, they had significantly lower rates of health-related technology use versus other patients with cancer (43% vs 53%, P = .006). However, in a multivariable model controlling for sociodemographic factors, the association between HNC and technology use was no longer statistically significant.
Figure 1.
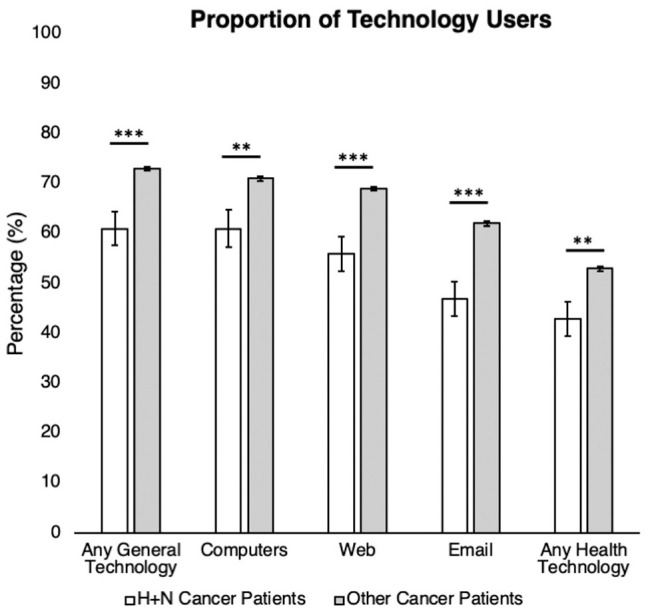
Technology use among patients with head and neck cancer vs other cancer. Error bars indicate 95% CI. **P < .01. ***P < .001.
Technology Use Among Patients With HNC
Among the HNC population, several demographic and socioeconomic factors were strongly associated with general and health-related technology use in univariate regression analysis ( Table 2 ). Increasing age was associated with lower rates of general and health-related technology use ( Figure 2a ). Patients with HNC <50 years old had the highest rates of technology use, with 88% and 74% reporting general and health-related technology use, respectively. In contrast, among patients aged ≥80 years, only 30% and 20% indicated general and health-related technology use (PR, 0.34 [95% CI, 0.22-0.55]; PR, 0.28 [95% CI 0.15-0.50]).
Table 2.
Demographic Differences in Computer-Based Technology Use Among Patients With Head and Neck Cancer.
| General use | Health-related use | |||
|---|---|---|---|---|
| % a | PR (95% CI) b | % a | PR (95% CI) b | |
| Overall | 60 | 43 | ||
| Sex | ||||
| Male | 62 | Reference | 46 | Reference |
| Female | 57 | 0.91 (0.71-1.15) | 38 | 0.83 (0.6-1.14) |
| Age, y | ||||
| <50 | 88 | Reference | 74 | Reference |
| 50-64 | 69 | 0.79 (0.64-0.96) c | 57 | 0.77 (0.57-1.05) |
| 65-79 | 56 | 0.63 (0.5-0.8) d | 31 | 0.42 (0.28-0.62) d |
| ≥80 | 30 | 0.34 (0.22-0.55) d | 20 | 0.28 (0.15-0.5) d |
| Race | ||||
| White | 70 | Reference | 46 | Reference |
| Other race | 67 | 0.83 (0.61-1.13) | 33 | 0.71 (0.44-1.14) |
| Cancer site | ||||
| Oral cavity | 74 | Reference | 54 | Reference |
| Pharynx | 61 | 0.82 (0.67-1.02) | 43 | 0.79 (0.58-1.08) |
| Larynx | 44 | 0.6 (0.4-0.9) c | 31 | 0.57 (0.34-0.98) c |
| Education | ||||
| Master | 96 | Reference | 84 | Reference |
| Bachelor | 79 | 0.82 (0.62-1.08) c | 61 | 0.84 (0.49-1.04) |
| Some college | 75 | 0.78 (0.66-0.92) e | 53 | 0.63 (0.48-0.85) e |
| High school | 51 | 0.54 (0.42-0.69) d | 31 | 0.36 (0.24-0.55) d |
| <High school | 17 | 0.18 (0.09-0.35) d | 11 | 0.13 (0.06-0.30) d |
| Income as % FPL | ||||
| ≥400 | 78 | Reference | 61 | Reference |
| 300 to <400 | 67 | 0.86 (0.64-1.15) | 36 | 0.59 (0.33-1.07) |
| 200 to <300 | 56 | 0.71 (0.48-1.04) | 26 | 0.42 (0.23-0.77) e |
| 100 to <200 | 40 | 0.51 (0.36-0.74) d | 32 | 0.52 (0.34-0.81) e |
| <100 | 36 | 0.46 (0.27-0.8) e | 29 | 0.47 (0.24-0.92) c |
| Region | ||||
| Northeast | 57 | Reference | 44 | Reference |
| Midwest | 61 | 1.06 (0.72-1.57) | 38 | 0.87 (0.52-1.48) |
| South | 57 | 0.99 (0.7-1.41) | 42 | 0.96 (0.61-1.51) |
| West | 72 | 1.25 (0.88-1.7) | 50 | 1.15 (0.72-1.83) |
| Health insurance | ||||
| Public | 50 | Reference | 33 | Reference |
| Private | 70 | 1.37 (1.1-1.7) e | 51 | 1.53 (1.01-2.02) c |
Abbreviations: FPL, federal poverty level; PR, prevalence ratio.
Weighted percentages.
Univariate robust Poisson regression.
P < .05.
P < .001.
P < .01.
Figure 2.
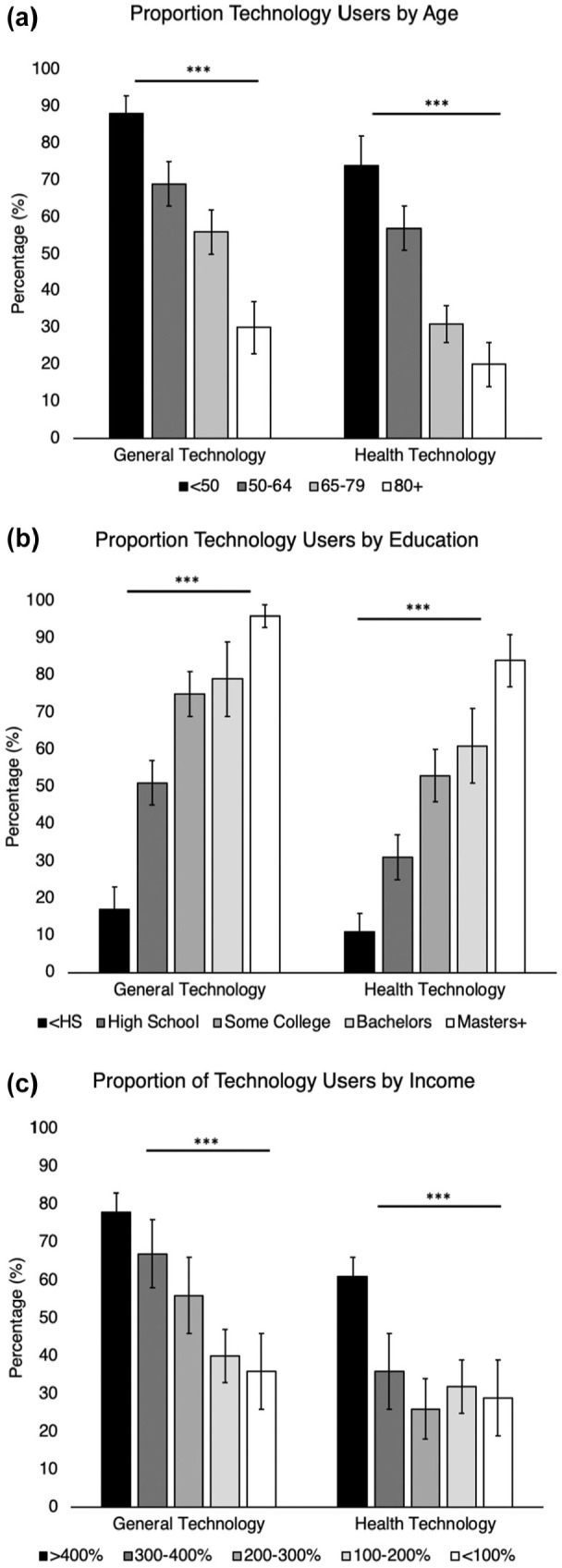
Technology use among patients with head and neck cancer by age and education. Percentage of health and general technology users by (a) education, (b) age, and (c) income. P value trend obtained through nonparametric correlation. Error bars indicate 95% CI. ***P < .001.
Lower educational attainment and income were associated with disparities in general and health-related technology use among patients with HNC ( Table 2 , Figure 2b and 2c ). Among patients with a master degree or higher, 96% and 84% reported use of general and health-related technology, respectively. In comparison, of those without a high school degree, just 17% and 11% indicated using general and health-related technology (PR, 0.18 [95% CI, 0.09-0.35]; PR, 0.13 [95% CI, 0.06-0.30]). Those who cited incomes <100% of the FPL were significantly less likely to use general or health-related technology as compared with those with incomes ≥400% of the FPL (PR, 0.46 [95% CI, 0.27-0.80]; PR, 0.47 [95% CI, 0.24-0.92]).
Finally, cancer site and health insurance status were weakly associated with technology use. Patients with laryngeal cancer were less likely to report general and health-related technology use when compared with those with oral cavity cancer (PR, 0.6 [95% CI, 0.4-0.9]; PR, 0.57 [95% CI, 0.34-0.98]). Patients with HNC with private health insurance were more likely than those with public insurance to report general and health-related technology use (PR, 1.37 [95% CI, 1.1-1.7]; PR, 1.53 [95% CI, 1.01-2.02]). Region, sex, and self-reported race were not significantly associated with general or health-related technology use.
Multivariable Models of Technology Use
Multivariable regression was performed to characterize factors that were independently associated with technology use in the HNC population ( Table 3 ). Older age and lower educational attainment were independently associated with lower likelihood of general and health-related technology use. Income <200% of the FPL was associated with lower rates of general but not health-related technology use. Health insurance status and cancer site were not associated with general or health-related technology use.
Table 3.
Multivariable Models of Technology Use Among Patients With Head and Neck Cancer.
| aPR (95% CI) a | ||
|---|---|---|
| General use | Health-related use | |
| Age, y | ||
| <50 | Reference | Reference |
| 50-64 | 0.86 (0.72-1.04) | 0.82 (0.61-1.11) |
| 65-79 | 0.71 (0.59-0.87) b | 0.46 (0.32-0.67) b |
| ≥80 | 0.47 (0.31-0.7) b | 0.39 (0.22-0.69) c |
| Cancer site | ||
| Oral cavity | Reference | Reference |
| Pharynx | 0.95 (0.82-1.11) | 1.09 (0.83-1.43) |
| Larynx | 0.73 (0.46-1.16) | 0.87 (0.5-1.51) |
| Education | ||
| Master or higher | Reference | Reference |
| Bachelor | 0.86 (0.71-1.04) | 0.76 (0.56-1.03) |
| Some college | 0.89 (0.72-1.08) | 0.66 (0.49-0.88) c |
| High school | 0.66 (0.51-0.85) c | 0.47 (0.3-0.74) c |
| <High school | 0.25 (0.13-0.48) b | 0.19 (0.08-0.43) b |
| Income as % FPL | ||
| ≥400 | Reference | Reference |
| 300 to <400 | 1.11 (0.80-1.54) | 0.75 (0.37-1.52) |
| 200 to <300 | 0.95 (0.67-1.35) | 0.62 (0.35-1.11) |
| 100 to <200 | 0.66 (0.48-0.91) d | 0.7 (0.48-1.04) |
| <100 | 0.61 (0.4-0.93) d | 0.59 (0.34-1.05) |
| Health insurance | ||
| Public | Reference | Reference |
| Private | 0.9 (0.73-1.1) | 0.86 (0.61-1.21) |
Abbreviations: aPR, adjusted prevalence ratio; FPL, federal poverty level.
Multivariable robust Poisson regression.
P < .001.
P < .01.
P < .05.
Discussion
The COVID-19 pandemic has accelerated the incorporation of telehealth into cancer care. However, little is known about the access to technology upon which telehealth relies for patients with HNC, a population commonly subject to socioeconomic disadvantages.6-8 We describe a substantially lower prevalence of technology use among individuals with a diagnosis of HNC when compared with individuals with other cancers in a nationally representative survey of health behaviors. This difference in prevalence can likely be attributed to the unique sociodemographic makeup of the HNC population, within which nearly half (40%) of patients reported no use of computers, internet, or email prior to the COVID-19 pandemic. Among patients with laryngeal cancer, a majority (56%) indicated no use of these technologies. We also identified older age and lower educational attainment as the strongest predictors of lower technology use among patients with HNC. As telehealth is increasingly implemented in head and neck oncology clinics, understanding barriers in access to basic technology among our most vulnerable patients is critical to avoiding exacerbation of the preexisting health care disparities exposed by the COVID-19 pandemic. 13
Our findings are consistent with prior data identifying socioeconomic barriers to technology access in the general population. While technology use has increased steeply over the past decade, 14 previous studies found that race, income, and sex continue to influence access to computers, smartphones, and internet.9,10,15 In addition, studies of patient portals have found that within vulnerable patient populations, lack of familiarity and limited experience with technology present barriers to portal use. 16
The findings of this study have concerning implications about the ability of many patients with HNC to participate in telehealth. Information gathering during virtual visits relies on thorough history taking and visual information obtained during videoconferencing. Guidelines for effective communication and performance of rudimentary physical examination maneuvers have been developed to help providers and patients engage in virtual care. 17 Patient participation in videoconferencing requires access to the internet and a camera-enabled device, as well as familiarity with the use of this technology, which our results indicate may not be realistic because of the social and financial challenges faced by many individuals with HNC.
When a patient is scheduled for a telehealth encounter, it is incumbent on providers to consider not only whether the type of encounter is appropriate for telehealth, which has been addressed elsewhere,2-4,17 but also whether the particular patient is able to effectively engage in telehealth. Patients with the characteristics described here, such as older age, less educational attainment, and lower income, may require additional educational and financial resources to support technology access to participate in telehealth visits. Patients with laryngeal cancer, who already face communication barriers, 18 may also experience unique challenges with telehealth. These characteristics should alert providers to patients who may need additional accommodations to participate in telehealth or perhaps may benefit significantly from an in-person visit instead, where there is a choice. Importantly, it is well known that delayed treatment causes increased mortality for patients with HNC,19,20 so the capacity of telehealth to facilitate timely care is a distinct advantage. Our findings do not negate the benefits of telehealth but rather underscore the importance of understanding and addressing inequities in technology access to support the use of telehealth in the HNC population.
Providers should be cautious about using phone visits as an alternative for patients with HNC who face barriers to videoconferencing visits, as lack of visual communication may result in a lower quality of care for socioeconomically disadvantaged individuals. Data from a randomized controlled trial demonstrated superiority of videoconferencing when compared with telephone alone for the diagnosis of stroke. 21 Other studies have shown that videoconferencing visits were associated with improved diagnostic accuracy, superior treatment decision making, and fewer medication errors when compared with telephone-only visits. 22 While studies have not yet compared videoconferencing and telephone care for oncology visits, published guidelines for the use of telehealth in the HNC population support the use of videoconferencing to maximize the information that can be obtained during a telehealth visit. 17
Importantly, measures can be undertaken at a policy level to bridge the technology gap and decrease socioeconomic barriers to telehealth access. The expansion of existing programs that provide federal funds for broadband access for telehealth would improve access of low-income patients to virtual care. 23 There may be a role for providing a laptop, tablet, smartphone, or other internet- and camera-enabled device to facilitate telehealth as a health insurance benefit for certain patients. Additional measures aimed at the promotion of technological literacy would complement these programs by improving familiarity with technology. 24
Limitations
There were several limitations to our study. First, our unweighted sample population of patients with HNC surveyed by the NHIS was just 381, limiting the power of our analysis. However, the complex sampling design used by the NHIS to create a representative national sample should improve the generalizability of our results. Furthermore, not all survey respondents in the adult sample answered all questions regarding technology use. Missing data were accounted for by performing statistical analyses on imputed and nonimputed data sets. The results of these 2 sets of analyses did not differ, indicating that the missing data likely had a minimal effect on our analysis. Finally, the NHIS did not include questions regarding smartphone use or access. Participants who did not report using computers may still use other internet-enabled devices, such as smartphones and tablets, which would facilitate telehealth visits. To mitigate the potential for overestimating the number of patients with barriers to telehealth access, patients were characterized as “not general technology users” if they indicated not using computers and not using internet.
Conclusion
COVID-19 has already disproportionately affected the health of minority and socioeconomically disadvantaged communities. 13 As clinicians continue to navigate the challenges of caring for patients with HNC during this pandemic, it is important not to widen existing disparities in care for socioeconomically disadvantaged groups. Telehealth is a valuable tool that allows providers to continue to care for patients while reducing risk of infection for patients and health care workers. However, our analysis demonstrates that there may be barriers to telehealth access for many patients. The socioeconomic risk factors that are strongly associated with HNC are also associated with less access to the technologies on which telehealth depends. Clinicians who care for patients with HNC and incorporate telehealth into practice should remain cognizant of barriers to telehealth use among their patients and perhaps explore ways to increase technology access for their most socioeconomically vulnerable patients.
Author Contributions
Chloe B. Warinner, study conception and design, data collection, statistical analysis, manuscript preparation and revisions; Tuna C. Hayirli, data collection, statistical analysis, manuscript revisions; Regan W. Bergmark, study conception and design, data collection, statistical analysis, manuscript preparation and revisions; Rosh Sethi, data collection, statistical analysis, manuscript revisions; Eleni M. Rettig, study conception and design, data collection, statistical analysis, manuscript preparation and revisions.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
References
- 1. Hollander JE, Carr BG. Virtually perfect? Telehealth for COVID-19. N Engl J Med. 2020;382(18):1679-1681. [DOI] [PubMed] [Google Scholar]
- 2. Prasad A, Carey RM, Rajasekaran K. Head and neck virtual medicine in a pandemic era: lessons from COVID-19. Head Neck. 2020;42(6):1308-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chua ML, Ma DJ, Anderson CM, Karam SD, Margalit DN, Kimple RJ. Follow-up and management of head and neck cancer patients during the 2019 novel coronavirus (SARS-CoV-2) disease pandemic. Adv Radiat Oncol. 2020;5(4):631-636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Qualliotine JR, Orosco RK. Self-removing passive drain to facilitate postoperative care via telehealth during the COVID-19 pandemic. Head Neck. 2020;42(6):1305-1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Faggiano F, Partanen T, Kogevinas M, Boffetta P. Socioeconomic differences in cancer incidence and mortality. IARC Sci Publ. 1997;138:65-176. [PubMed] [Google Scholar]
- 6. Rettig EM, D’Souza G. Epidemiology of head and neck cancer. Surg Oncol Clin N Am. 2015;24(3):379-396. [DOI] [PubMed] [Google Scholar]
- 7. Faggiano F, Partanen T, Kogevinas M, Boffetta P. Socioeconomic differences in cancer incidence and mortality. IARC Sci Publ. 1997;138:65-176. [PubMed] [Google Scholar]
- 8. Johnson S, McDonald JT, Corsten MJ. Socioeconomic factors in head and neck cancer. J Otolaryngol Head Neck Surg. 2008;37(4):597-601. [PubMed] [Google Scholar]
- 9. Graboyes E, Cramer J, Balakrishnan Ket al. COVID-19 pandemic and health care disparities in head and neck cancer: scanning the horizon. Head Neck. 2020;42(7):1555-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rajasekaran K. Access to telehealth—are we doing all that we can during the COVID-19 pandemic? Otolaryngol Head Neck Surg. 2020;163(1):104-106. [DOI] [PubMed] [Google Scholar]
- 11. National Center for Health Statistics. National Health Interview Survey. Updated May 28, 2020. Accessed May 29, 2020. https://www.cdc.gov/nchs/nhis/index.htm
- 12. Blewett LA, Rivera Drew JA, King ML, Williams K. IPUMS Health Surveys: National Health Interview Survey. Version 6.4. IPUMS; 2019. [Google Scholar]
- 13. Burks CA, Ortega G, Bergmark RW. COVID-19, disparities, and opportunities for equity in otolaryngology—unequal America. JAMA Otolaryngol Head Neck Surg. [DOI] [PubMed] [Google Scholar]
- 14. Hung LY, Lyons JG, Wu CH. Health information technology use among older adults in the United States, 2009-2018. Curr Med Res Opin. 2020;36(5):789-797. [DOI] [PubMed] [Google Scholar]
- 15. Farlie RW. Are We Really a Nation Online? Ethnic and Racial Disparities in Access to Technology and Their Consequences. Leadership Conference on Civil Rights Education Fund; 2005. [Google Scholar]
- 16. Grossman LV, Creber RMM, Ancker JSet al. Technology access, technical assistance, and disparities in inpatient portal use. Appl Clin Inform. 2019;10(1):40-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Prasad A, Brewster R, Newman JG, Rajasekaran K. Optimizing your telehealth visit during the COVID-19 pandemic: practice guidelines for patients with head and neck cancer. Head Neck. 2020;42(6):1317-1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Blood GW, Dineen M, Kauffman SM, Raimondi SC, Simpson KC. Perceived control, adjustment, and communication problems in laryngeal cancer survivors. Perceptual and Motor Skills. 1993;77(3):764-766. [DOI] [PubMed] [Google Scholar]
- 19. Coca-Pelaz A, Takes RP, Hutcheson Ket al. head and neck cancer: a review of the impact of treatment delay on outcome. Adv Ther. 2018;35(2):153-160. [DOI] [PubMed] [Google Scholar]
- 20. Schutte HW, Heutink F, Wellenstein DJet al. Impact of time to diagnosis and treatment in head and neck cancer: a systematic review. Otolaryngol Head Neck Surg. 2020;162(4):446-457. [DOI] [PubMed] [Google Scholar]
- 21. Capampangan DJ, Wellik KE, Bobrow BJet al. Telehealth versus telephone for remote emergency stroke consultations: a critically appraised topic. Neurologist. 2009;15(3):163-166. [DOI] [PubMed] [Google Scholar]
- 22. Rush KL, Howlett L, Munro A, Burton L. Videoconference compared to telephone in healthcare delivery: a systematic review. Int J Med Inform. 2018;118:44-53. [DOI] [PubMed] [Google Scholar]
- 23. Bauerly BC, McCord RF, Hulkower R, Pepin D. Broadband access as a public health issue: the role of law in expanding broadband access and connecting underserved communities for better health outcomes. J Law Med Ethics. 2019;47(2, suppl):39-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gould CE, Hantke NC. Promoting technology and virtual visits to improve older adult mental health in the face of COVID-19. Am J Geriatr Psychiatry. 2020;28(8):889-890. [DOI] [PMC free article] [PubMed] [Google Scholar]


