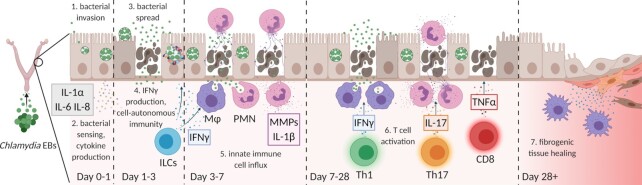
Figure 2.
Course of immune responses during murine genital Chlamydia infection. (A) Infectious elementary bodies (EBs) ascend through the cervix into the uterine horns and potentially to the oviducts and ovaries. EBs enter epithelial cells, establish membrane-bound inclusion bodies, and differentiate into replicative reticular bodies. (B) Bacteria are sensed by epithelial cell pattern recognition receptors, and epithelial cells produce cytokines and chemokines, including IL-1α, IL-6 and IL-8, to activate nearby immune cells. (C) Chlamydia extrude inclusions from infected cells or lyse infected cells, as bacteria spread to neighboring cells. (D) Tissue-resident immune cells (such as ILCs or γδT cells) produce IFNγ, which activates epithelial cell-autonomous immunity. C. trachomatis is effectively cleared by cell-autonomous immunity, but C. muridarum infection persists. (E) Innate immune cells such as macrophages and neutrophils accumulate in the genital tract, engulfing and destroying extracellular bacteria. Neutrophils comprise the most prominent source of matrix metalloproteases (MMPs) and reactive oxygen species, which contribute to tissue damage. (F) Chlamydia-specific lymphocytes traffic to the genital mucosa. Th1 cells sustain production of IFNγ, driving clearance of Chlamydia infection. Th17 cells produce IL-17, strengthening pathogenic neutrophil responses. CD8+ T cells produce TNFα, further driving tissue damage. (G) Wound-healing responses repair damaged tissue, resulting in pathogenic fibrosis and genital scarring. Figure created with Biorender.com.