This cohort study evaluates the incidence, cost, and length of hospitalizations associated with seasonal respiratory viruses from 2011 to 2017 among older adults who live in long-term care facilities.
Key Points
Question
What is the burden of cardiorespiratory events attributable to influenza and respiratory syncytial virus (RSV) among older adults residing in long-term care facilities (LTCFs) in the US?
Findings
In this cohort study of 2 909 106 LTCF residents, a total of 10 939 influenza- and RSV-attributable cardiorespiratory events occurred from 2011 to 2017 for an incidence rate of 215 events per 100 000 person-years, with a cost of $91 055 393 and 56 858 hospitalization days.
Meaning
Results of this study suggest that older adults in LTCFs remain vulnerable to seasonal influenza and RSV infections; thus, resources should be invested to prevent transmission and reduce the burden on LTCF residents and the US health care system.
Abstract
Importance
Older adults residing in long-term care facilities (LTCFs) are at a high risk of being infected with respiratory viruses, such as influenza and respiratory syncytial virus (RSV). Although these infections commonly have many cardiorespiratory sequelae, the national burden of influenza- and RSV-attributable cardiorespiratory events remains unknown for the multimorbid and vulnerable LTCF population.
Objective
To estimate the incidence of cardiorespiratory hospitalizations that were attributable to influenza and RSV among LTCF residents and to quantify the economic burden of these hospitalizations on the US health care system by estimating their associated cost and length of stay.
Design, Setting, and Participants
This retrospective cohort study used national Medicare Provider Analysis and Review inpatient claims and Minimum Data Set clinical assessments for 6 respiratory seasons (2011-2017). Long-stay residents of LTCFs were identified as those living in the facility for at least 100 days (index date), aged 65 years or older, and with 6 months of continuous enrollment in Medicare Part A were included. Follow-up occurred from the resident’s index date until the first hospitalization, discharge from the LTCF, disenrollment from Medicare, death, or the end of the study. Residents could re-enter the sample; thus, long-stay episodes of care were identified. Data analysis was performed between January 1 and September 30, 2020.
Exposures
Seasonal circulating pandemic 2009 influenza A(H1N1), human influenza A(H3N2), influenza B, and RSV.
Main Outcomes and Measures
Cardiorespiratory hospitalizations (eg, asthma exacerbation, heart failure) were identified using primary diagnosis codes. Influenza- and RSV-attributable cardiorespiratory events were estimated using a negative binomial regression model adjusted for weekly circulating influenza and RSV testing data. Length of stay and costs of influenza- and RSV-attributable events were then estimated.
Results
The study population comprised 2 909 106 LTCF residents with 3 138 962 long-stay episodes and 5 079 872 person-years of follow-up. Overall, 10 939 (95% CI, 9413-12 464) influenza- and RSV-attributable cardiorespiratory events occurred, with an incidence of 215 (95% CI, 185-245) events per 100 000 person-years. The cost of influenza- and RSV-attributable cardiorespiratory events was $91 055 393 (95% CI, $77 885 316-$104 225 470), and the length of stay was 56 858 (95% CI, 48 757-64 968) days.
Conclusions and Relevance
This study found that many cardiorespiratory hospitalizations among LTCF residents in the US were attributable to seasonal influenza and RSV. To minimize the burden these events place on the health care system and residents of LTCFs and to prevent virus transmission, additional preventive measures should be implemented.
Introduction
Each year, influenza and respiratory syncytial virus (RSV) are responsible for substantial morbidity and mortality among older adults in the US.1 Adults aged 65 years or older accounted for more than 50% of influenza-associated hospitalizations and 64% of influenza-associated deaths during the 2014 to 2015 respiratory season as well as approximately $2.6 billion in medical costs in 2015.2,3 In the US, annual estimates of deaths associated with RSV were approximately 14 000, with more than 177 000 inpatient admissions, at a cost of more than $1 billion in high-risk and older adults.4 Given the high incidence of multimorbidity and susceptibility to adverse infection–related sequelae in older adults, these respiratory infections are particularly burdensome. In particular, influenza and RSV infections commonly have cardiorespiratory sequelae that include acute myocardial infarction, stroke, and exacerbation of asthma and chronic obstructive pulmonary disease.4,5,6 Although evidence of the incidence and risk factors for influenza and RSV infections among older adults is starting to emerge,4,7,8,9,10,11,12,13,14 little is known about the implications of these respiratory viruses for the most vulnerable group: residents of long-term care facilities (LTCFs).
The 1.3 million older adults living in LTCFs each year are at a heightened risk for influenza and RSV infections compared with their community-dwelling counterparts, and outbreaks with serious consequences are common in this population.15,16 Residents of LTCFs are more susceptible to respiratory infections for several reasons. First, older adults are at a high risk for influenza and RSV infections because of age-related physiological changes, such as reduced chest wall compliance, decreased cough strength, and impaired immune function attributed to cellular senescence.17,18,19 Previous work has also shown that impaired functional status and advanced age (ie, ≥85 years) are major risk factors for pneumonia and influenza hospitalizations among LTCF residents.20 Second, the risk of infection is increased because of the institutional nature of LTCFs and by frequent exposure to co-residents, visitors, volunteers, and staff, all of whom may transmit viruses.15,21,22 Third, frail residents with decreased functional capacity may experience the most severe forms of illness, requiring transfer to the hospital for supportive care and services that are not often provided in the LTCF setting.
To date, studies have evaluated the association of influenza and RSV infections with functional decline, hospitalization for infection, and death among LTCF residents.20,23,24,25 However, the national burden of cardiorespiratory events that are attributable to influenza and RSV in LTCFs is largely unknown.7,20,23,24,25,26 Without such knowledge, the types of policies implemented and the amount of resources allocated to reduce respiratory virus transmission and burden in LTCFs could be inadequate and, at worst, systematically harmful. Given the vulnerability of the LTCF population, a better understanding of the role of influenza and RSV in cardiorespiratory outcomes is warranted.
Using a national population of LTCF residents from 2011 to 2017, we conducted a retrospective cohort study. The objectives of this study were to estimate the incidence of cardiorespiratory hospitalizations that were attributable to seasonal influenza and RSV and to quantify the economic burden of these hospitalizations on the US health care system by estimating their associated cost and length of stay (LOS).
Methods
The institutional review board at Brown University approved the study protocol and waived the need for informed consent because of the use of deidentified data. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.27
Data Sources
In this retrospective cohort study, we used Medicare Provider Analysis and Review (MedPAR) inpatient claims that were linked to the Medicare Master Beneficiary Summary File, Minimum Data Set version 3.0 clinical assessment records, and national Centers for Disease Control and Prevention weekly circulating influenza and RSV testing data for all LTCF residents enrolled in Medicare. MedPAR claims supplied information on inpatient admission diagnosis, cost, and LOS; these data have been previously described.23 In addition, we obtained national data on weekly circulating influenza strains reported from public health and clinical laboratories from the publicly available FluView Interactive and RSV Surveillance Data sources from the Centers for Disease Control and Prevention. These data included the weekly percentage of seasonal influenza and RSV specimens with positive results for pandemic 2009 influenza A(H1N1), human influenza A(H3N2), influenza B, and RSV polymerase chain reaction tests. Weekly data from the clinical and public health reporting laboratories of the Centers for Disease Control and Prevention were combined through the entire study period.
Study Design and Population
The study cohort was derived from a national source population of LTCF residents with more than 21 million Minimum Data Set–defined episodes of care between July 3, 2011, and July 1, 2017. The entire study period included 6 distinct respiratory seasons, with each season starting on the Sunday of Morbidity and Mortality Weekly Report (MMWR) week 27 of one year and ending on the Saturday of MMWR week 26 of the following year.28 Eligible long-stay LTCF residents had a total stay of 100 consecutive days or more and no more than 10 days outside of the facility. Index dates were assigned as the 100th day of a stay for long-stay residents. Follow-up ranged from each resident’s index date until hospitalization, discharge from the LTCF, disenrollment from Medicare, death, or the end of the study period, whichever occurred first. The first long-stay episode of care was identified within a respiratory season, and subsequent stays were excluded. If LTCF residents were censored in 1 season, they could re-enter during a subsequent season. Person-time for LTCF residents was then aggregated within the MMWR-defined weeks. For example, if residents were in an LTCF for 7 person-days from Sunday to Saturday, they were associated with 1 person-week during a specific MMWR-defined week. Long-stay residents included in the study population had 6 months of continuous enrollment in Medicare Part A immediately before and were at least aged 65 years at the index date in each season. Individuals were categorized into the following age groups according to their age at index date in each season: 65 to 74 years, 75 to 84 years, and 85 years or older.
Cardiorespiratory Hospitalizations
Using MedPAR inpatient claims, we identified hospitalizations that occurred while individuals were residents of an LTCF. Hospitalizations were identified by the presence of an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) or International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis code in the principal position on the claim.29 Cardiovascular hospitalizations (ICD-9-CM codes 390.XX-459.XX; ICD-10-CM codes I00.XX-I99.XX) and respiratory hospitalizations (ICD-9-CM codes 460XX-519.XX; ICD-10-CM codes J00.XX-J08.XX and J12.XX-J99.XX) were identified as cardiorespiratory events. We identified explicit hospitalizations for pneumonia and influenza (ICD-9-CM codes 480.XX-488.XX; ICD-10-CM codes J09.XX-J18.XX) and RSV (ICD-9-CM codes 079.6. 480.1 and 466.11; ICD-10-CM codes J121, J205, J210, and B974) in which the virus was directly named in the diagnosis associated with the ICD-9-CM or ICD-10-CM code (eg, “Pneumonia due to respiratory syncytial virus”). This identification was done to quantify the incidence of admissions specifically for influenza and RSV infections. We chose to group pneumonia and influenza because pneumonia is often preceded by influenza infection, and these infections are difficult to distinguish using claims data.23,30 We estimated the cardiorespiratory events attributable to influenza and RSV, which were defined as any cardiorespiratory hospitalizations other than the aforementioned explicit pneumonia and influenza and RSV hospitalizations.
Statistical Analysis
We obtained estimates for seasonal influenza- and RSV-attributable cardiorespiratory hospitalizations by fitting negative binomial regression excess models, a method commonly used in surveillance studies.8,31,32 Candidate models that were fit and compared consisted of different linear combinations of (1) a continuous measure of week number transformed with sine and cosine harmonic terms (ie, Fourier series) to allow annual or semiannual periodicity trends; (2) polynomial terms (quadratic and cubic) for number of weeks from the first observed time point to model nonlinear, aperiodic time trends; and (3) indicators for viral activity, both influenza viral subtype and RSV, with or without 1- to 2-week lags to account for delays between viral testing and attributable hospitalizations. Model selection was guided by the Akaike information criteria, with the best model chosen on the basis of the lowest Akaike information criteria. The final model contained an annual Fourier term; polynomial week terms (quadratic and cubic); and 2-week lagged viral terms for pandemic 2009 influenza A(H1N1), human influenza A(H3N2), influenza B, and RSV; the models were offset with the natural log-transformed number of person-weeks at risk. The final binomial regression model containing polynomial terms for time trends, annual sine (sin) and cosine (cos) harmonic terms, and 2-week lagged viral terms for percentage of weekly influenza and respiratory syncytial virus (RSV) specimens with positive test results is as follows:
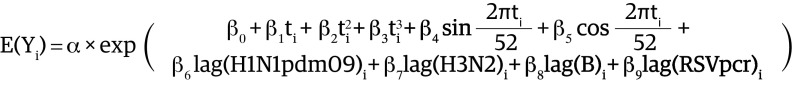 , ,
|
where E(Y) is the expected number of cardiorespiratory hospitalizations during a given week, H1N1pdm09 is pandemic 2009 influenza A(H1N1), H3N2 is seasonal human influenza A(H3N2), B indicates influenza B, and PCR is polymerase chain reaction.
The final model was fit to obtain estimated values for cardiorespiratory hospitalizations in the presence of influenza and RSV over the entire study period. A second model was fit with weekly viral terms set to 0, representing the cardiorespiratory events expected in the absence of influenza and RSV. The difference between the 2 estimates represents the influenza- and RSV-attributable cardiorespiratory hospitalizations. Weekly influenza- and RSV-attributable events and long-stay LTCF resident person-weeks at risk were summed across the entire study window. In the primary analysis, weekly estimates for negative (ie, less than 0) influenza- and RSV-attributable events were set to 0 because of the infeasibility of negative attributable events. A stability analysis was performed without setting negative weekly events to 0 to assess the robustness of the results to this assumption. Attributable cardiorespiratory events were also estimated separately for both influenza and RSV. Incidence rates were calculated by dividing the attributable events by the total person-time at risk. Incidence rates were then scaled to 100 000 person-years. This process was repeated separately in each age group.
The overall cost in US dollars, derived from the Medicare reimbursement for hospitalization, and LOS of attributable events were estimated using information from the MedPAR inpatient claims. Claim reimbursements throughout each year were converted to 2017 inflation-adjusted dollars using the gross domestic product price index.33 Within each age group, the distributions of observed cardiorespiratory hospitalizations were selected and the top and bottom 0.5% of each distribution were excluded to remove outliers. The mean costs of cardiorespiratory hospitalizations and LOS were then taken and multiplied by the attributable events within each age group. Attributable hospitalization costs and LOS were then summed across age groups to obtain overall totals. We estimated CIs for a difference in means to obtain 95% CIs for attributable events.
Data were analyzed with SAS, version 9.4 (SAS Institute Inc) and R, version 3.5.1 (R Foundation for Statistical Computing) using the package flumodelr, a publicly available R package developed by members of our team (K.W.M., R.v.A, and A.R.Z.).34 Data analysis was performed between January 1 and September 30, 2020.
Results
Throughout the 6 respiratory seasons, the study population of 2 909 106 LTCF residents were associated with 3 138 962 long-stay episodes (eFigure 1 in the Supplement), including 581 423 episodes (18.5%) for the 65 to 74 years age group; 1 062 587 episodes (33.9%) for the 75 to 84 years age group; and 1 494 952 episodes (47.6%) for the 85 years or older age group as well as 2 134 400 episodes (68.0%) among female and 2 626 867 episodes (83.7%) among non-Hispanic White LTCF residents. A total of 5 079 872 person-years of follow-up and 606 140 observed cardiorespiratory events occurred (Table 1). Long-stay residents 85 years or older were associated with the greatest amount of person-time (2 655 918 person-years) and observed cardiorespiratory events (287 354 events, or 47.4% of all events), whereas those in the 65 to 74 years age group were associated with the least, with 783 660 person-years and 107 824 cardiorespiratory events (17.8% of all events). Across all age groups, observed cardiovascular events were more frequent than observed respiratory events (371 621 vs 234 519). Pneumonia and influenza and RSV were less frequently identified as a primary reason for hospitalization compared with cardiorespiratory events (Table 1).
Table 1. Observed Hospitalizations for Pneumonia and Influenza; Respiratory Syncytial Virus (RSV); and Respiratory, Cardiovascular, and Cardiorespiratory Events, 2011-2017.
| Age group, y | No. of observed hospitalizations (%)a | |||||
|---|---|---|---|---|---|---|
| Pneumonia and influenzab | RSVc | Respiratory eventd | Cardiovascular evente | Cardiorespiratory eventf | Person-years | |
| 65-74 | 26 025 (14.8) | 40 (13.6) | 48 089 (20.5) | 59 735 (16.1) | 107 824 (17.8) | 783 660 (15.4) |
| 75-84 | 57 528 (32.8) | 101 (34.2) | 84 891 (36.2) | 126 071 (33.9) | 210 962 (34.8) | 1 640 294 (32.3) |
| ≥85 | 91 707 (52.3) | 154 (52.2) | 101 539 (43.3) | 185 815 (50.0) | 287 354 (47.4) | 2 655 918 (52.3) |
| Overall | 175 260 | 295 | 234 519 | 371 621 | 606 140 | 5 079 872 |
The observed hospitalizations identified represent the number of long-stay episodes that ended in a specific type of hospitalization.
Pneumonia and influenza hospitalizations were identified using the following ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) and International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes in primary diagnosis position: 480.XX-488.XX and J09.XX-J18.XX.
RSV hospitalizations were identified using the following ICD-9-CM and ICD-10-CM codes in the primary diagnosis position: 079.6. 480.1, 466.11, J121, J205, J210, and B974.
Respiratory hospitalizations were identified using the following ICD-9-CM and ICD-10-CM codes in the primary diagnosis position: 460.XX-519.XX, J00.XX-J08.XX, and J19.XX-J99.XX (excluding pneumonia and influenza and RSV hospitalizations).
Cardiovascular hospitalizations were identified using the following ICD-9-CM and ICD-10-CM codes in the primary diagnosis position: ICD-9-CM: 390.XX-459.XX; ICD-10-CM: I00.XX-I99.XX (excluding pneumonia and influenza and RSV hospitalizations).
Cardiorespiratory hospitalizations are the combined total of cardiovascular and respiratory hospitalizations (excluding pneumonia and influenza and RSV hospitalizations).
Influenza- and RSV-Attributable Cardiorespiratory Events
Overall, 10 939 (95% CI, 9413-12 464) influenza- and RSV-attributable cardiorespiratory events occurred across the entire study period for an incidence rate of 215 (95% CI, 185-245) events per 100 000 person-years (Table 2). Long-stay residents 85 years or older experienced the greatest number of attributable events, with 7852 (95% CI, 7204-8501) events and a rate of 296 (95% CI, 271-320) attributable events per 100 000 person-years. The fewest attributable events occurred among long-stay residents aged 65 to 74 years, with 741 (95% CI, 415-1067) events and a rate of 95 (95% CI, 53-136) attributable events per 100 000 person-years (Table 2).
Table 2. Influenza- and Respiratory Syncytial Virus–Attributable Cardiorespiratory Hospitalizationsa .
| Age group, y | Attributable events, No. (95% CI) | Person-years, No. | Attributable event rate per 100 000 person-years, No. (95% CI) |
|---|---|---|---|
| 65-74 | 741 (415-1067) | 783 660 | 95 (53-136) |
| 75-84 | 2345 (1795-2896) | 1 640 294 | 143 (109-177) |
| ≥85 | 7852 (7204-8501) | 2 655 918 | 296 (271-320) |
| Total | 10 939 (9413-12 464) | 5 079 872 | 215 (185-245) |
Final negative binomial regression model was used to estimate hospitalizations. Estimates for each age group were rounded to the nearest whole number and thus may not perfectly reflect the sum total.
Attributable events occurred most frequently in respiratory seasons 2011 to 2012, 2012 to 2013, 2014 to 2015, and 2016 to 2017, which were predominated by seasonal human influenza A(H3N2) rather than pandemic 2009 influenza A(H1N1) (eFigures 2 and 3 in the Supplement). The 2013 to 2014 season was predominated by pandemic 2009 influenza A(H1N1), which corresponded with few attributable cardiorespiratory events across all age groups, particularly those aged 75 to 84 years and those 85 years or older. Attributable events were most common between November and March of each respiratory season (Figure). A decreasing time trend in expected hospitalizations was observed across all ages for the 6 included seasons (Figure). When estimated separately, 6883 (95% CI, 5684-8082) events were attributed to influenza across all age groups, and 6196 (95% CI, 4736-7656) events were attributed to RSV (eTable 1 and eFigures 4-6 in the Supplement). Estimates were slightly lower in the stability analysis, in which negative weekly events were set to 0, with 7723 (95% CI, 6198-9249) estimated attributable events at a rate of 152 (95% CI, 122-182) per 100 000 person-years (eTable 2 in the Supplement).
Figure. Weekly Observed and Model-Estimated Cardiorespiratory Hospitalization Rates Among Long-term Care Facility (LTCF) Residents Between 2011 and 2017.
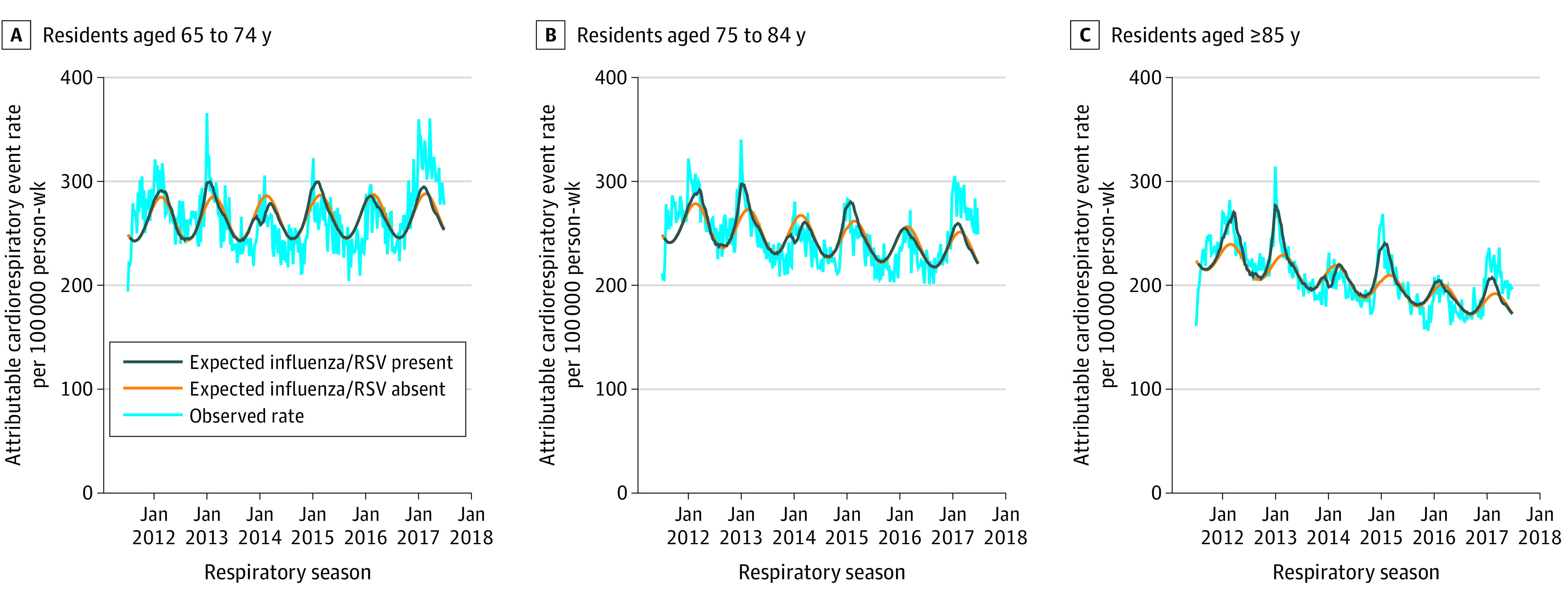
The light blue line represents the observed cardiorespiratory hospitalizations per 100 000 person-weeks during a given week. The dark blue line represents the expected cardiorespiratory hospitalizations per 100 000 person-weeks when influenza and respiratory syncytial virus (RSV) are present. The orange line represents the expected cardiorespiratory hospitalization per 100 000 person-weeks when influenza and RSV are not circulating (ie, the viral terms are set to 0). The difference between the orange and blue lines represents the influenza- and RSV-attributable cardiorespiratory hospitalizations among LTCF residents. Weeks with the dark blue line above the orange line represent positive (ie, greater than 0) attributable hospitalization estimates, whereas weeks with the dark blue line below the orange line represent negative (ie, less than 0) attributable hospitalization estimates.
Cost and LOS of Influenza- and RSV-Attributable Hospitalizations
The overall cost of inpatient influenza- and RSV-attributable cardiorespiratory events across 6 respiratory seasons among long-stay LTCF residents in the US was $91 055 393 (95% CI, $77 885 316-$104 225 470), with an attributable LOS of 56 858 (95% CI, 48 757-64 968) days (Table 3). The mean cost and LOS of attributable events were highest among long-stay residents aged 65 to 74 years; however, these older adults were associated with the lowest attributable cost ($7 251 327; 95% CI, $4 062 650-$10 440 003) and LOS (4150 days; 95% CI, 2324-5975) of cardiorespiratory events. Long-stay residents 85 years or older had the lowest mean cost ($63 705 272; 95% CI, $58 441 926-$68 968 617) and LOS (40 045 days; 95% CI, 36 740-43 355) of attributable events (Table 3). When estimated separately, the total inpatient cost of $57 430 571 (95% CI, $47 081 375-$67 779 766) and LOS of 35 772 (95% CI, 29 416-42 129) days across all age groups were attributable to influenza, whereas a total inpatient cost of $51 503 105 (95% CI, $38 899 971-$64 106 240) and LOS of 32 008 (95% CI, 24 267-39 749) days were attributable to RSV (eTable 3 in the Supplement). In the stability analysis, the attributable costs were $63 165 257 (95% CI, $50 004 725-$76 342 473) and the attributable LOS was 39 703 (95% CI, 31 602-47 864) days (eTable 4 in the Supplement).
Table 3. Mean Cost and Length of Stay (LOS) for Influenza- and Respiratory Syncytial Virus–Attributable Cardiorespiratory Hospitalizations.
| Age group, y | Attributable event, No. (95% CI) | Mean cost (SE), $a | Attributable cost (95% CI), $ | Mean LOS (SE), da | Attributable LOS (95% CI), d |
|---|---|---|---|---|---|
| 65-74 | 741 (415-1067) | 9783 (7655) | 7 251 327 (4 062 650-10 440 003) | 5.6 (4.9) | 4150 (2324-5975) |
| 75-84 | 2345 (1795-2896) | 8571 (6167) | 20 098 795 (15 380 740-24 816 850) | 5.4 (4.6) | 12 663 (9693-15 638) |
| ≥85 | 7852 (7204-8501) | 8113 (5150) | 63 705 272 (58 441 926-68 968 617) | 5.1 (4.1) | 40 045 (36 740-43 355) |
| Total | 10 939 (9413-12 464) | 8738 (6274) | 91 055 393 (77 885 316-104 225 470) | 5.3 (4.6) | 56 858 (48 757-64 968) |
Mean cost and LOS were calculated using the middle 99% of the distribution for cost and LOS of cardiorespiratory hospitalizations for each age group. Cost estimates represent 2017 inflation-adjusted costs.
Discussion
In this national retrospective cohort study, we combined weekly viral surveillance data with inpatient claims and nursing home assessments from 2011 to 2017 to quantify influenza- and RSV-attributable cardiorespiratory events among LTCF residents. We found that influenza and RSV were associated with cardiorespiratory morbidity in LTCF residents and were followed by hospital stays and a large economic burden to the health care system. Specifically, we estimated that 10 939 cardiorespiratory hospitalizations among LTCF residents could be attributed to influenza and RSV. Attributable cardiorespiratory events were most common in the 4 respiratory seasons in which seasonal human influenza A(H3N2) was predominant. This finding was expected: it is well documented that seasonal human influenza A(H3N2)–predominant seasons are associated with greater morbidity and mortality among older adults in the general public compared with pandemic 2009 influenza A(H1N1) and influenza B.31,35 Most attributable cardiorespiratory hospitalizations occurred among the oldest long-stay LTCF residents (aged ≥85 years), thereby generating the largest share of attributable costs and LOSs. Hospitalizations cost a total of $91 055 393 in 2017 inflation-adjusted dollars and lasted more than 56 858 days. However, adults 85 years or older had the lowest mean cost of hospitalization compared with other age groups, which has also been observed among community-dwelling adults who were hospitalized for influenza, and may reflect less aggressive treatment for individuals with the most advanced age or a greater competing risk of mortality.36 Overall, we found that influenza and RSV accounted for more than $15 million in inpatient costs to Medicare each year. This work extends what is currently known about the implications of influenza and RSV for community-dwelling older adults by quantifying the associated cardiorespiratory illnesses among the national population of LTCF residents who are highly susceptible to influenza and RSV infection because of a multitude of predisposing physical and environmental risk factors.
The finding that long-stay residents 85 years or older had attributable event rates that were double the rates for those aged 75 to 84 years and more than triple for those aged 65 to 74 years was expected. Decreased durability of the immune response to influenza vaccination and waning antibody titers may be associated with further increased susceptibility to infection among older adults.37 Likewise, declines in T-cell function have been correlated with severe RSV infections among older adults.38 Moreover, it has been well described that inflammation associated with infections can trigger thrombotic events, such as acute myocardial infarction or stroke.39,40,41,42 Acute respiratory infections can also exacerbate existing cardiovascular conditions, such as heart failure, or respiratory conditions, such as asthma or chronic obstructive pulmonary disease.43,44,45 Given that the prevalence of cardiovascular and respiratory comorbidities increases with age, adults 85 years or older may be at a greater risk for a cardiorespiratory event after a respiratory infection compared with middle-aged and younger adults. It is also possible that cardiorespiratory sequelae capture the attention of clinicians, leaving underlying respiratory infections unrecognized. In this case, infections that are not evaluated through diagnostic testing will go undiagnosed. The findings of this study support this explanation given the relative magnitude of observed influenza and RSV diagnoses compared with influenza- and RSV-attributable cardiorespiratory events.
Studies of the consequences of influenza and RSV among older adults in the US have focused on excess mortality and few have estimated attributable cardiorespiratory hospitalizations and their costs.4,7,8,9,10,11,12,13,14 One previous study estimated the cardiopulmonary hospitalizations attributed to influenza among residents of 381 LTCFs in Tennessee from 1995 to 1999 (4 influenza seasons).7 The authors used a rate-differencing approach and found an incidence of 660 (95% CI, 410-920) cardiorespiratory hospitalizations per 100 000 person-years among LTCF residents in Tennessee during influenza season.7 Another study among older adults enrolled in health care organizations in Oregon, Washington, and California applied a rate-differencing approach during 4 influenza seasons (from 1996 to 1999).9 Mullooly et al9 found influenza-attributable cardiorespiratory hospitalization rates of 107.5 (95% CI, 87.1-127.8) among high-risk and 28.3 (95% CI, 17.9-38.8) among low-risk adults 65 years or older per 10 000 person-periods, stratified by high-risk comorbidities. The present study calculated the mean outcome of influenza over 6 full seasons, generating higher time at risk and lower incidence rates. This approach differed from the approach in Mullooly et al9 of restricting to time at risk when circulating influenza was greatest. Thus, the incidence estimate in the present study of 215 events per 100 000 person-years for the entire study period is comparable to the incidence in high-risk older adults found in the previous study.9
Among the US Department of Veterans Affairs population, the largest influenza-attributable cardiorespiratory hospitalizations have been reported for those 65 years or older.32 The annual costs in this population were $36 million for influenza-related inpatient visits and $6.2 million for emergency department visits.32 Young-Xu et al32 incorporated circulating RSV data when adjusting for influenza-attributable hospitalizations but did not report both influenza- and RSV-attributable events. In Colorado, influenza-attributable cardiorespiratory events were most frequent during seasonal human influenza A(H3N2)–predominant seasons.8 With regard to circulating RSV, a landmark study estimated the association between laboratory-confirmed RSV infection and cardiopulmonary events in older adults and high-risk individuals who were admitted to several hospitals over 4 respiratory seasons.4 Falsey et al4 found that RSV accounted for the following rates of hospital admissions: 10.6% for pneumonia, 11.4% for chronic obstructive pulmonary disease, 5.4% for heart failure, and 7.2% for asthma. Overall, Falsey et al4 provided high-quality evidence of the large burden RSV places on older adults and high-risk individuals.
The results of the present study support the need to implement preventive strategies in LTCFs to reduce the transmission of influenza and RSV, particularly among those at greatest risk of adverse events.46,47 Furthermore, the emergence of SARS-CoV-2 in early 2020 and the resulting COVID-19 pandemic demonstrated the susceptibility of LTCF residents to respiratory viruses and reinforced the need for LTCFs to devote resources to infection prevention and control programs. We believe the information from this study is helpful for seasonal planning and for allocating scarce resources to obtain critical supplies (eg, personal protective equipment). These findings may also help with calculations of plausible estimates for how interventions to reduce the risk of COVID-19 (eg, personal protective equipment) may be applied to other respiratory viruses, such as influenza and RSV in LTCFs, and how such interventions might be compared with one another. Vaccination of LTCF residents and staff remains one of the most important means of preventing influenza infection. States can support LTCF vaccination efforts by developing vaccine supply programs to prevent supply chain disruptions and reduce barriers to vaccine acquisition.48
Limitations
This study has several limitations. The national measures of weekly influenza and RSV activity that we used do not take into account the geographic heterogeneity of seasonal virus circulation, which potentially masks the implications of influenza and RSV for regions with varied demographics. We also did not account for outbreaks in LTCFs, which are common and may result in excess cardiorespiratory hospitalizations.15,16 In addition, the study period did not include pandemic seasons (eg, pandemic 2009 influenza A[H1N1]), and thus the findings should be interpreted as non-pandemic estimates. The outcome of cardiorespiratory hospitalizations considered only those patients who were admitted for inpatient care and did not reflect the events managed in the LTCFs by clinicians. Long-stay residents who were sent to the emergency department and then returned to the LTCF or those who were placed under observation were not captured.49 Despite these limitations, this study presents conservative estimates of cardiorespiratory illnesses among residents of LTCFs.
Conclusions
Older adults in LTCFs remain vulnerable to influenza and RSV infections, which are associated with morbidity. Resources should be devoted to prevent the transmission of seasonal influenza and RSV in LTCFs and to reduce the burden on LTCF residents and the health care system.
eFigure 1. Flow Diagram
eFigure 2. United States Weekly Influenza and RSV Positive Tests Reported from the CDC Clinical and Public Health Laboratories Between 2011-2017
eFigure 3. Weekly Observed Cardiorespiratory Hospitalizations Among LTCF Residents from 2011-2017
eTable 1. Attributable Cardiorespiratory Hospitalizations Estimated Using Final Negative Binomial Model
eFigure 4. Influenza and RSV-Attributable Events
eFigure 5. Influenza-Attributable Events
eFigure 6. RSV-Attributable Events
eTable 2. Stability Analysis—Influenza and RSV-Attributable Cardiorespiratory Hospitalizations Estimated Using Final Negative Binomial Model
eTable 3. Average Cost and LOS of Attributable Cardiorespiratory Hospitalizations Estimated Using Final Negative Binomial Model
eTable 4. Stability Analysis—Average Cost and Length of Stay for Influenza and RSV-Attributable Cardiorespiratory Hospitalizations
References
- 1.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179-186. doi: 10.1001/jama.289.2.179 [DOI] [PubMed] [Google Scholar]
- 2.Ozawa S, Portnoy A, Getaneh H, et al. Modeling the economic burden of adult vaccine-preventable diseases in the United States. Health Aff (Millwood). 2016;35(11):2124-2132. doi: 10.1377/hlthaff.2016.0462 [DOI] [PubMed] [Google Scholar]
- 3.Rolfes MA, Foppa IM, Garg S, et al. 2015-2016 Estimated influenza illnesses, medical visits, hospitalizations, and deaths averted by vaccination in the United States. Accessed April 3, 2021. https://www.cdc.gov/flu/about/disease/2015-16.htm
- 4.Falsey AR, Hennessey PA, Formica MA, Cox C, Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352(17):1749-1759. doi: 10.1056/NEJMoa043951 [DOI] [PubMed] [Google Scholar]
- 5.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1(3):274-281. doi: 10.1001/jamacardio.2016.0433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sellers SA, Hagan RS, Hayden FG, Fischer WA II. The hidden burden of influenza: a review of the extra-pulmonary complications of influenza infection. Influenza Other Respir Viruses. 2017;11(5):372-393. doi: 10.1111/irv.12470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ellis SE, Coffey CS, Mitchel EF Jr, Dittus RS, Griffin MR. Influenza- and respiratory syncytial virus-associated morbidity and mortality in the nursing home population. J Am Geriatr Soc. 2003;51(6):761-767. doi: 10.1046/j.1365-2389.2003.51254.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Czaja CA, Miller L, Colborn K, et al. State-level estimates of excess hospitalizations and deaths associated with influenza. Influenza Other Respir Viruses. 2020;14(2):111-121. doi: 10.1111/irv.12700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mullooly JP, Bridges CB, Thompson WW, et al. ; Vaccine Safety Datalink Adult Working Group . Influenza- and RSV-associated hospitalizations among adults. Vaccine. 2007;25(5):846-855. doi: 10.1016/j.vaccine.2006.09.041 [DOI] [PubMed] [Google Scholar]
- 10.Matias G, Taylor R, Haguinet F, Schuck-Paim C, Lustig R, Shinde V. Estimates of mortality attributable to influenza and RSV in the United States during 1997-2009 by influenza type or subtype, age, cause of death, and risk status. Influenza Other Respir Viruses. 2014;8(5):507-515. doi: 10.1111/irv.12258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matias G, Taylor R, Haguinet F, Schuck-Paim C, Lustig R, Shinde V. Estimates of hospitalization attributable to influenza and RSV in the US during 1997-2009, by age and risk status. BMC Public Health. 2017;17(1):271. doi: 10.1186/s12889-017-4177-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matias G, Taylor RJ, Haguinet F, Schuck-Paim C, Lustig RL, Fleming DM. Modelling estimates of age-specific influenza-related hospitalisation and mortality in the United Kingdom. BMC Public Health. 2016;16:481. doi: 10.1186/s12889-016-3128-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fleming DM, Taylor RJ, Lustig RL, et al. Modelling estimates of the burden of respiratory syncytial virus infection in adults and the elderly in the United Kingdom. BMC Infect Dis. 2015;15(1):443. doi: 10.1186/s12879-015-1218-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Falsey AR, McElhaney JE, Beran J, et al. Respiratory syncytial virus and other respiratory viral infections in older adults with moderate to severe influenza-like illness. J Infect Dis. 2014;209(12):1873-1881. doi: 10.1093/infdis/jit839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matheï C, Niclaes L, Suetens C, Jans B, Buntinx F. Infections in residents of nursing homes. Infect Dis Clin North Am. 2007;21(3):761-772, ix. doi: 10.1016/j.idc.2007.07.005 [DOI] [PubMed] [Google Scholar]
- 16.Simor AE. Influenza outbreaks in long-term-care facilities: how can we do better? Infect Control Hosp Epidemiol. 2002;23(10):564-567. doi: 10.1086/501971 [DOI] [PubMed] [Google Scholar]
- 17.Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006;1(3):253-260. doi: 10.2147/ciia.2006.1.3.253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lowery EM, Brubaker AL, Kuhlmann E, Kovacs EJ. The aging lung. Clin Interv Aging. 2013;8:1489-1496. doi: 10.2147/CIA.S51152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yanagi S, Tsubouchi H, Miura A, Matsuo A, Matsumoto N, Nakazato M. The impacts of cellular senescence in elderly pneumonia and in age-related lung diseases that increase the risk of respiratory infections. Int J Mol Sci. 2017;18(3):E503. doi: 10.3390/ijms18030503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moyo P, Zullo AR, McConeghy KW, et al. Risk factors for pneumonia and influenza hospitalizations in long-term care facility residents: a retrospective cohort study. BMC Geriatr. 2020;20(1):47. doi: 10.1186/s12877-020-1457-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marrie TJ. Pneumonia in the long-term-care facility. Infect Control Hosp Epidemiol. 2002;23(3):159-164. doi: 10.1086/502030 [DOI] [PubMed] [Google Scholar]
- 22.Jackson MM, Fierer J, Barrett-Connor E, et al. Intensive surveillance for infections in a three-year study of nursing home patients. Am J Epidemiol. 1992;135(6):685-696. doi: 10.1093/oxfordjournals.aje.a116348 [DOI] [PubMed] [Google Scholar]
- 23.Bosco E, Zullo AR, McConeghy KW, et al. Long-term care facility variation in the incidence of pneumonia and influenza. Open Forum Infect Dis. 2019;6(6):ofz230. doi: 10.1093/ofid/ofz230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gozalo PL, Pop-Vicas A, Feng Z, Gravenstein S, Mor V. Effect of influenza on functional decline. J Am Geriatr Soc. 2012;60(7):1260-1267. doi: 10.1111/j.1532-5415.2012.04048.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pop-Vicas A, Rahman M, Gozalo PL, Gravenstein S, Mor V. Estimating the effect of influenza vaccination on nursing home residents’ morbidity and mortality. J Am Geriatr Soc. 2015;63(9):1798-1804. doi: 10.1111/jgs.13617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bosco E, Zullo AR, McConeghy KW, et al. Geographic variation in pneumonia and influenza in long-term care facilities: a national study. Clin Infect Dis. 2020;71(8):e202-e205. doi: 10.1093/cid/ciaa081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med. 2007;45(4):247-251. doi: 10.1016/j.ypmed.2007.08.012 [DOI] [PubMed] [Google Scholar]
- 28.Midgley CM, Haynes AK, Baumgardner JL, et al. Determining the seasonality of respiratory syncytial virus in the United States: the impact of increased molecular testing. J Infect Dis. 2017;216(3):345-355. doi: 10.1093/infdis/jix275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) . Estimates of deaths associated with seasonal influenza—United States, 1976-2007. MMWR Morb Mortal Wkly Rep. 2010;59(33):1057-1062. [PubMed] [Google Scholar]
- 30.Walter ND, Taylor TH, Shay DK, et al. ; Active Bacterial Core Surveillance Team . Influenza circulation and the burden of invasive pneumococcal pneumonia during a non-pandemic period in the United States. Clin Infect Dis. 2010;50(2):175-183. doi: 10.1086/649208 [DOI] [PubMed] [Google Scholar]
- 31.Thompson WW, Weintraub E, Dhankhar P, et al. Estimates of US influenza-associated deaths made using four different methods. Influenza Other Respir Viruses. 2009;3(1):37-49. doi: 10.1111/j.1750-2659.2009.00073.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young-Xu Y, van Aalst R, Russo E, Lee JK, Chit A. The annual burden of seasonal influenza in the US Veterans Affairs population. PLoS One. 2017;12(1):e0169344. doi: 10.1371/journal.pone.0169344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bureau of Economic Analysis . National income and product accounts: tables. Accessed April 4, 2021. https://apps.bea.gov/iTable/iTable.cfm?reqid=19&step=2#reqid=19&step=2&isuri=1&1921=survey
- 34.McConeghy KW, van Aalst R, Zullo A, Joyce N. Flumodelr: an R package for estimating attributable influenza morbidity and mortality. Accessed September 23, 2020. https://kmcconeghy.github.io/flumodelr/
- 35.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333-1340. doi: 10.1001/jama.292.11.1333 [DOI] [PubMed] [Google Scholar]
- 36.Fingar KR, Liang L, Stocks C. Inpatient hospital stays and emergency department visits involving influenza, 2006–2016. Statistical Brief #253. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality; 2019. [PubMed] [Google Scholar]
- 37.Dugan HL, Henry C, Wilson PC. Aging and influenza vaccine-induced immunity. Cell Immunol. 2020;348:103998. doi: 10.1016/j.cellimm.2019.103998 [DOI] [PubMed] [Google Scholar]
- 38.Cherukuri A, Patton K, Gasser RA Jr, et al. Adults 65 years old and older have reduced numbers of functional memory T cells to respiratory syncytial virus fusion protein. Clin Vaccine Immunol. 2013;20(2):239-247. doi: 10.1128/CVI.00580-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kytömaa S, Hegde S, Claggett B, et al. Association of influenza-like illness activity with hospitalizations for heart failure: the Atherosclerosis Risk in Communities Study. JAMA Cardiol. 2019;4(4):363-369. doi: 10.1001/jamacardio.2019.0549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Howard PA, Kleoppel JW. Influenza vaccine for cardiovascular risk reduction. Hosp Pharm. 2013;48(10):813-817. doi: 10.1310/hpj4810-813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Modin D, Jørgensen ME, Gislason G, et al. Influenza vaccine in heart failure: cumulative number of vaccinations, frequency, timing, and survival—a Danish nationwide cohort study. Circulation. 2019;139(5):575-586. doi: 10.1161/CIRCULATIONAHA.118.036788 [DOI] [PubMed] [Google Scholar]
- 42.Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345-353. doi: 10.1056/NEJMoa1702090 [DOI] [PubMed] [Google Scholar]
- 43.Viniol C, Vogelmeier CF. Exacerbations of COPD. Eur Respir Rev. 2018;27(147):170103. doi: 10.1183/16000617.0103-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwarze J, Openshaw P, Jha A, et al. Influenza burden, prevention, and treatment in asthma-A scoping review by the EAACI Influenza in Asthma Task Force. Allergy. 2018;73(6):1151-1181. doi: 10.1111/all.13333 [DOI] [PubMed] [Google Scholar]
- 45.Cates CJ, Rowe BH. Vaccines for preventing influenza in people with asthma. Cochrane Database Syst Rev. 2013;2013(2):CD000364. doi: 10.1002/14651858.CD000364.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kopsaftis Z, Wood-Baker R, Poole P. Influenza vaccine for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2018;6:CD002733. doi: 10.1002/14651858.CD002733.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith SC Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58(23):2432-2446. doi: 10.1016/j.jacc.2011.10.824 [DOI] [PubMed] [Google Scholar]
- 48.Ahmed F, Paine V, Zhang F, Gary E, Lindley MC. Evaluation of a legislatively mandated influenza vaccination program for adults in Rhode Island, USA. J Public Health Manag Pract. 2010;16(5):E01-E08. doi: 10.1097/PHH.0b013e3181c60ed4 [DOI] [PubMed] [Google Scholar]
- 49.Kramer A, Fish R, Lin M, Min S. National Variation in Hospitalization and Emergency Department/Observation Visits for Medicare Beneficiaries Receiving Long-term Care in Nursing Centers. Medicare Payment Advisory Committee; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Flow Diagram
eFigure 2. United States Weekly Influenza and RSV Positive Tests Reported from the CDC Clinical and Public Health Laboratories Between 2011-2017
eFigure 3. Weekly Observed Cardiorespiratory Hospitalizations Among LTCF Residents from 2011-2017
eTable 1. Attributable Cardiorespiratory Hospitalizations Estimated Using Final Negative Binomial Model
eFigure 4. Influenza and RSV-Attributable Events
eFigure 5. Influenza-Attributable Events
eFigure 6. RSV-Attributable Events
eTable 2. Stability Analysis—Influenza and RSV-Attributable Cardiorespiratory Hospitalizations Estimated Using Final Negative Binomial Model
eTable 3. Average Cost and LOS of Attributable Cardiorespiratory Hospitalizations Estimated Using Final Negative Binomial Model
eTable 4. Stability Analysis—Average Cost and Length of Stay for Influenza and RSV-Attributable Cardiorespiratory Hospitalizations


