Supplemental Digital Content is available in the text.
Keywords: cardiovascular disease, cerebrovascular disease, COVID-19, health disparities, pandemic, mortality, race/ethnicity
Background:
Cardiovascular deaths increased during the early phase of the COVID-19 pandemic in the United States. However, it is unclear whether diverse racial/ethnic populations have experienced a disproportionate rise in heart disease and cerebrovascular disease deaths.
Methods:
We used the National Center for Health Statistics to identify heart disease and cerebrovascular disease deaths for non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic individuals from March to August 2020 (pandemic period), as well as for the corresponding months in 2019 (historical control). We determined the age- and sex-standardized deaths per million by race/ethnicity for each year. We then fit a modified Poisson model with robust SEs to compare change in deaths by race/ethnicity for each condition in 2020 versus 2019.
Results:
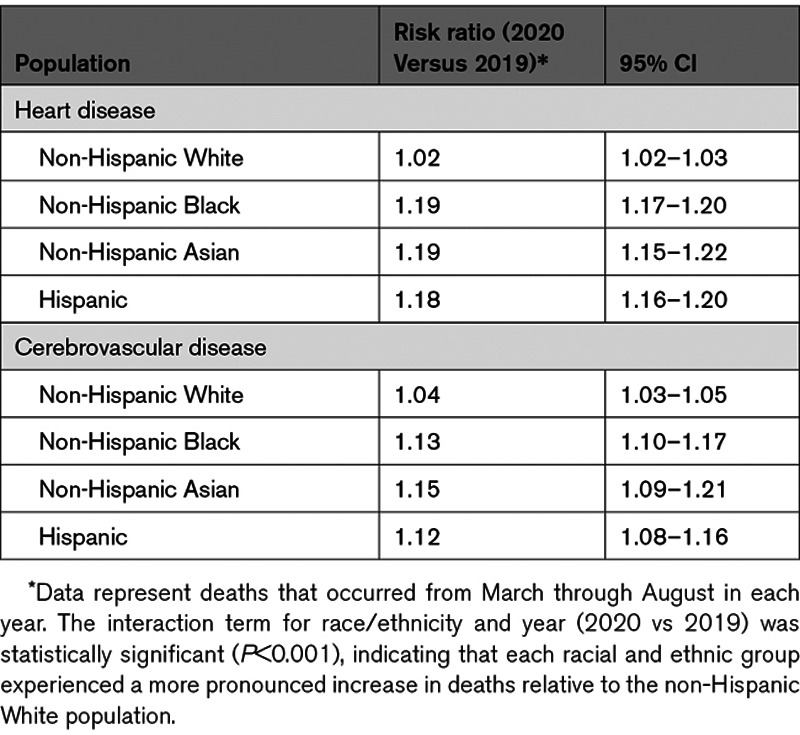
There were a total of 339 076 heart disease and 76 767 cerebrovascular disease deaths from March through August 2020, compared with 321 218 and 72 190 deaths during the same months in 2019. Heart disease deaths increased during the pandemic in 2020, compared with the corresponding period in 2019, for non-Hispanic White (age–sex standardized deaths per million, 1234.2 versus 1208.7; risk ratio for death [RR], 1.02 [95% CI, 1.02–1.03]), non-Hispanic Black (1783.7 versus 1503.8; RR, 1.19 [95% CI, 1.17–1.20]), non-Hispanic Asian (685.7 versus 577.4; RR, 1.19 [95% CI, 1.15–1.22]), and Hispanic (968.5 versus 820.4; RR, 1.18 [95% CI, 1.16–1.20]) populations. Cerebrovascular disease deaths also increased for non-Hispanic White (268.7 versus 258.2; RR, 1.04 [95% CI, 1.03–1.05]), non-Hispanic Black (430.7 versus 379.7; RR, 1.13 [95% CI, 1.10–1.17]), non-Hispanic Asian (236.5 versus 207.4; RR, 1.15 [95% CI, 1.09–1.21]), and Hispanic (264.4 versus 235.9; RR, 1.12 [95% CI, 1.08–1.16]) populations. For both heart disease and cerebrovascular disease deaths, Black, Asian, and Hispanic populations experienced a larger relative increase in deaths than the non-Hispanic White population (interaction term, P<0.001).
Conclusions:
During the COVID-19 pandemic in the United States, Black, Hispanic, and Asian populations experienced a disproportionate rise in deaths caused by heart disease and cerebrovascular disease, suggesting that these groups have been most impacted by the indirect effects of the pandemic. Public health and policy strategies are needed to mitigate the short- and long-term adverse effects of the pandemic on the cardiovascular health of diverse populations.
Clinical Perspective.
What Is New?
Although cardiovascular deaths increased during the coronavirus disease 2019 (COVID-19) pandemic in the United States, it is unclear whether racial and ethnic diverse populations were disproportionately affected.
Our findings demonstrate that Black, Hispanic, and Asian populations each experienced a ≈20% relative increase in heart disease deaths, and an ≈13% relative increase in cerebrovascular disease deaths, during the COVID-19 pandemic. In contrast, the non-Hispanic White population experienced a 2% and 4% relative increase in deaths due to these causes, respectively.
Black, Asian, and Hispanic populations experienced a larger relative increase in heart disease and cerebrovascular disease deaths than the non-Hispanic White population.
What Are the Clinical Implications?
During the COVID-19 pandemic, Black, Hispanic, and Asian populations experienced a disproportionate rise in deaths caused by heart disease and cerebrovascular disease compared with non-Hispanic White people, suggesting that these racial/ethnic groups have been most impacted by the indirect effects of the pandemic.
Public health and policy strategies are urgently needed to mitigate the short- and long-term adverse effects of the pandemic on the cardiovascular health of diverse racial/ethnic populations.
The novel coronavirus disease 2019 (COVID-19) pandemic has disrupted the delivery of health care services to patients with cardiovascular disease in the United States. During the early phase of the pandemic, hospitalizations for acute cardiovascular conditions such as myocardial infarction and stroke declined by 40% to 50% across the country.1–4 At the same time, population-level deaths caused by cardiac and cerebrovascular causes increased in some geographic regions,5 raising concern that the pandemic has had a substantial, indirect toll on patients with non—COVID-19–related medical conditions.
Despite the concerning national rise in cardiovascular deaths during the pandemic, little is known about whether these increases have been disproportionately concentrated among racially and ethnically diverse populations. A large body of evidence has shown that Black and Hispanic communities have borne a high burden of COVID-19.6–10 It is possible that these communities have also been disproportionately affected by factors that have contributed to an increase in heart and cerebrovascular disease deaths, including reduced access to health care services, increased health system strain, and hospital avoidance caused by fear of contracting the virus in high-burden areas.11–14 In addition, inequities in the social determinants of health that are associated with cardiovascular risk, such as poverty and stress, have worsened for these groups.15–17 Understanding how deaths have changed across different racial and ethnic populations is critically important, and could inform public health strategies to mitigate the short- and long-term adverse effects of the pandemic on cardiovascular health.
Therefore, in this study, we aimed to characterize heart disease and cerebrovascular deaths by race and ethnicity (non-Hispanic White, non-Hispanic Black, Asian, and Hispanic populations) during the US COVID-19 pandemic in 2020 compared with a historical control (2019). In addition, we evaluated whether relative increases in deaths were more pronounced among diverse racial and ethnic groups, compared with non-Hispanic White persons, after the onset of the pandemic in 2020 relative to corresponding months in 2019.
Methods
The data that support the findings of this study are publicly available from the National Center for Health Statistics (NCHS).
Data
We obtained monthly cause of death data from the NCHS from March through August 2020, as well as for the corresponding months in 2019.18,19 We focused on deaths beginning in March because this is when many states began to experience a rapid rise in COVID-19 cases and issued stay-at-home orders. International Classification of Diseases, Tenth Revision codes were used to identify underlying causes of death caused by heart diseases (I00-I09, I11, I13, I20-I51) and cerebrovascular diseases (I60-I69). Deaths with an underlying cause of COVID-19 were excluded.
Race and Ethnicity
Information about the race/ethnicity for deaths is obtained from death certificates by the NCHS. We included the following racial/ethnic groups in the analysis: non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic. We excluded American Indian/Alaska Natives and racial/ethnic groups designated as “other” because data for these groups were often suppressed because of low counts in accordance with NCHS confidentiality standards. Population data for each race/ethnicity were obtained from the American Community Survey files.
Statistical Analysis
To determine heart disease and cerebrovascular disease deaths by race and ethnicity, we divided the total number of deaths (March through August of each respective year) for each condition by the total population (per million) of each group. We then calculated age- and sex-standardized deaths per million for each racial and ethnic group (non-Hispanic Black, non-Hispanic Asian, and Hispanic) by applying direct standardization using census counts of the White population (in 2019) as the reference. Using the same reference population, the direct standardization approach was also applied to determine monthly age- and sex-standardized deaths per million for each racial and ethnic group. The relative and absolute monthly difference in deaths per million in 2020 versus 2019 was calculated for each racial and ethnic group.
Next, we fit a modified Poisson regression model with robust SEs to calculate the risk ratio for death in 2020 versus 2019 for each racial/ethnic group after adjustment for age and sex.20 We used this approach because information on deaths for each condition was available as summarized (grouped tabular) binomial data (eg, the number of deaths for each unique combination of age strata in 5-year intervals, sex, and racial/ethnic group). The modified Poisson model is a numerically stable procedure, and use of the robust variance allows for valid inference (eg, accounting for heteroscedasticity).20,21 Our model included an interaction term for race/ethnicity and year, which allowed us to compare the relative risk of death for each racial/ethnic group (versus non-Hispanic White) in 2020 versus 2019.
Two-sided P<0.05 defined statistical significance. Analyses were performed using R 3.5.2. Institutional Board Review approval from Beth Israel Deaconess Medical Center was not required because of the use of publicly available, deidentified datasets.
Results
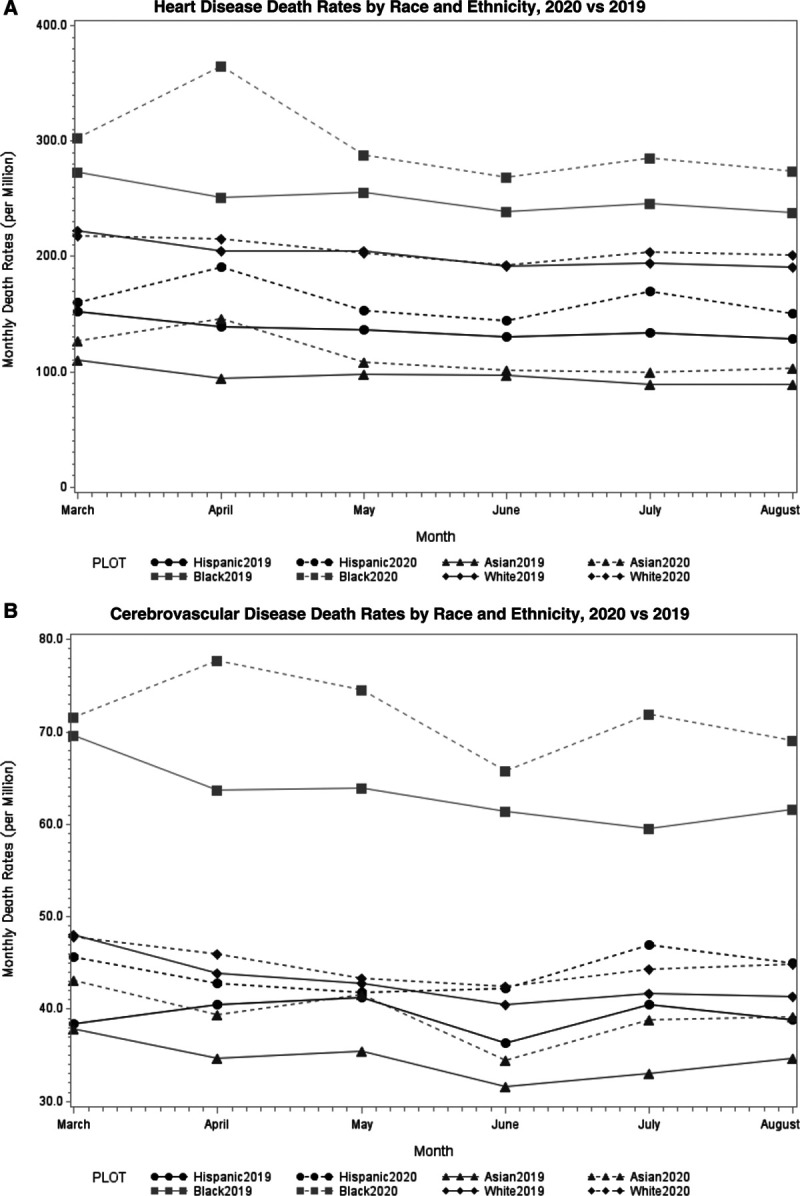
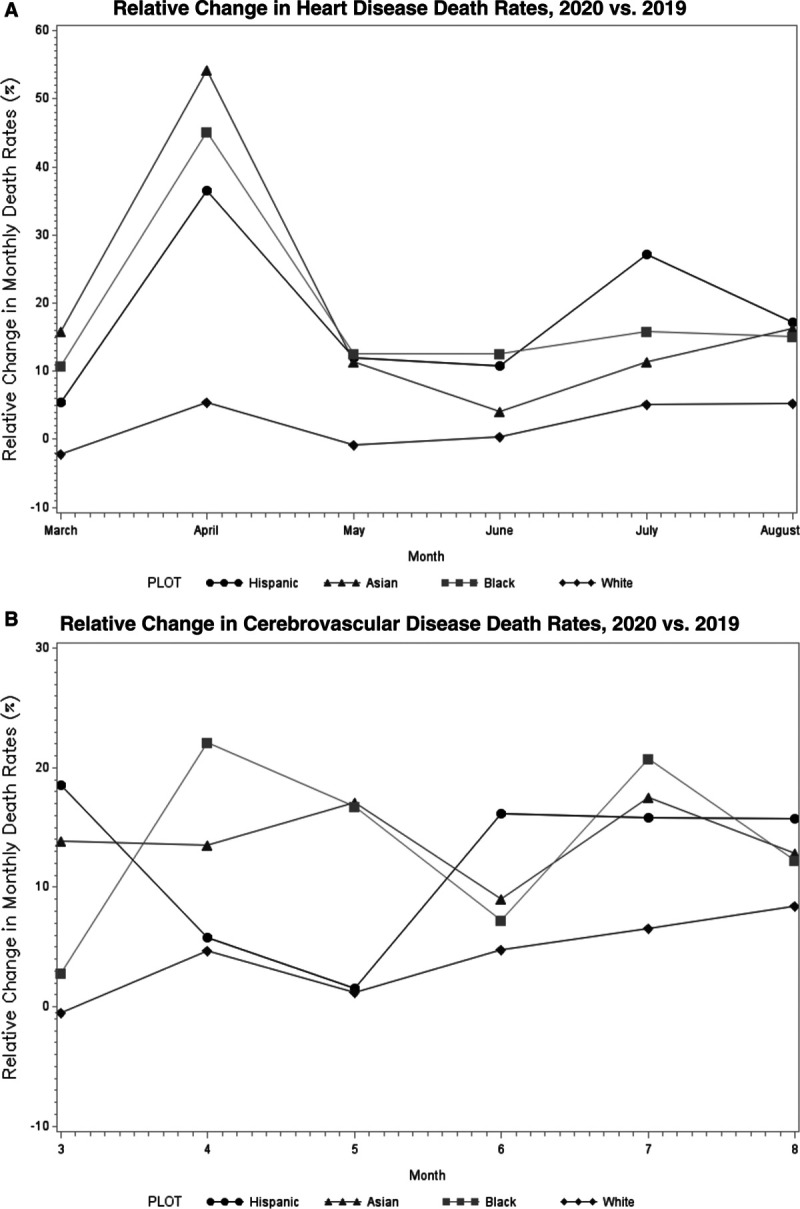
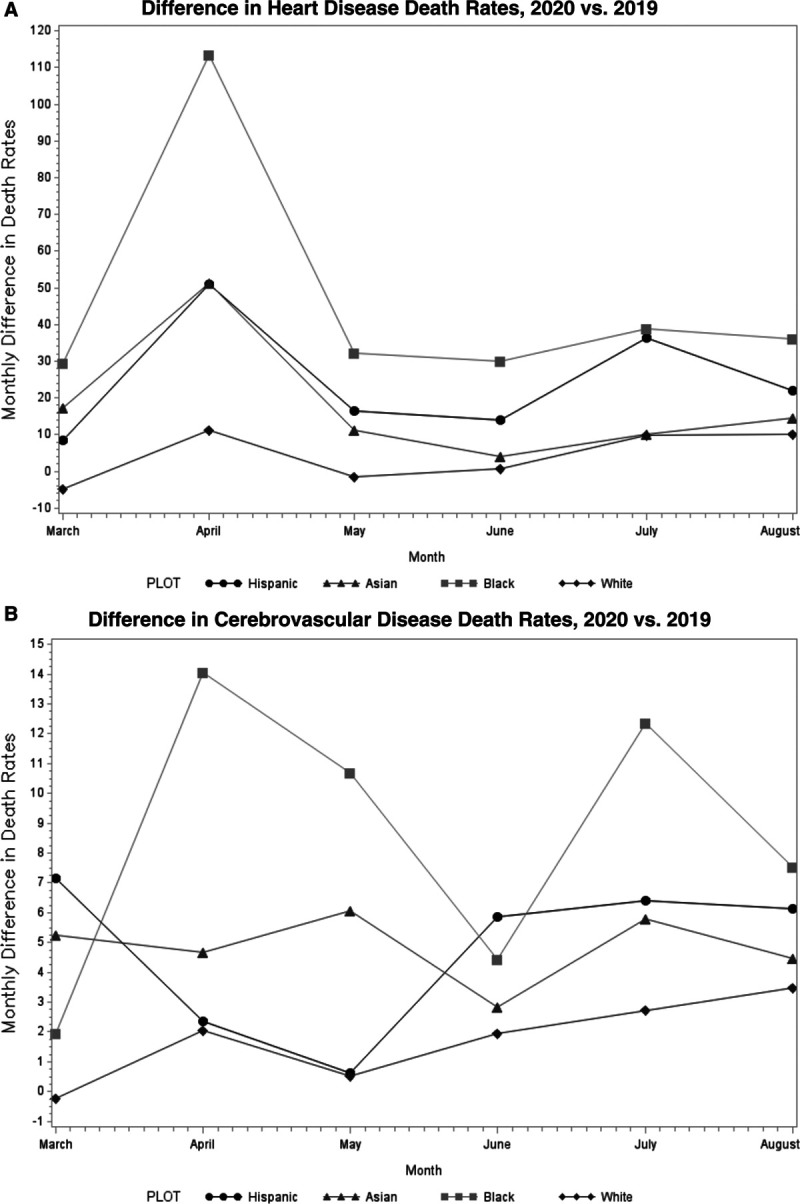
In the United States, there were a total of 339 076 heart disease and 76 767 cerebrovascular disease deaths during the pandemic from March through August 2020, compared with 321 218 and 72 190 deaths during the corresponding months in 2019. Observed heart disease and cerebrovascular disease deaths per million for each year are shown by race and ethnicity in Table I in the Data Supplement, and age–sex standardized deaths per million are shown in Table 1. In addition, monthly age–sex standardized deaths per million are shown in Figure 1. The relative and absolute monthly differences are shown by race/ethnicity (2020 versus 2019) in Figures 2 and 3.
Table 1.
Age–Sex Standardized Heart Disease and Cerebrovascular Disease Deaths per Million by Race and Ethnicity
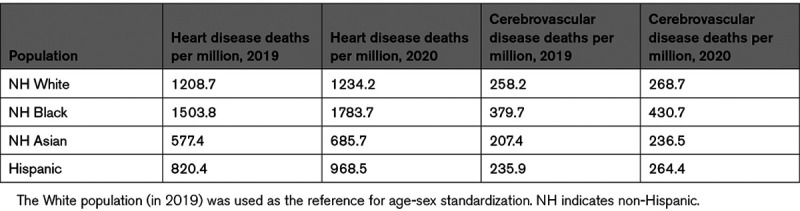
Figure 1.
Monthly age–sex standardized heart disease and cerebrovascular disease deaths per million by race and ethnicity, 2020 vs 2019. Age–sex standardized heart disease (A) and cerebrovascular disease (B) deaths per million from March through August 2020 (dashed lines) compared with corresponding months in 2019 (solid lines) for non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic populations.
Figure 2.
Relative monthly change in age–sex standardized heart disease and cerebrovascular disease deaths per million by race and ethnicity, 2020 vs 2019. Relative (%) change in age–sex standardized heart disease (A) and cerebrovascular disease (B) deaths per million from March through August (2020 vs 2019) for non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic populations.
Figure 3.
Absolute monthly differences in age–sex standardized heart disease and cerebrovascular disease deaths per million by race and ethnicity, 2020 vs 2019. Absolute differences in age–sex standardized heart disease (A) and cerebrovascular disease (B) deaths per million from March through August (2020 vs 2019) for non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, and Hispanic populations.
Overall, heart disease deaths increased during the pandemic in 2020 compared with the corresponding period in 2019 for non-Hispanic White (age–sex standardized deaths per million, 1234.2 versus 1208.7; risk ratio [RR], 1.02 [95% CI, 1.02–1.03]), non-Hispanic Black (1783.7 versus 1503.8; RR, 1.19 [95% CI, 1.17–1.20]), non-Hispanic Asian (685.7 versus 577.4; RR, 1.19 [95% CI, 1.15–1.22]), and Hispanic (968.5 versus 820.4; RR, 1.18 [95% CI, 1.16–1.20]) populations (Table 2 and Figure I in the Data Supplement). Cerebrovascular disease deaths also increased for non-Hispanic White (age–sex standardized deaths per million, 268.7 versus 258.2; RR, 1.04 [95% CI, 1.03–1.05]), non-Hispanic Black (430.7 versus 379.7; RR, 1.13 [95% CI, 1.10–1.17]), non-Hispanic Asian (236.5 versus 207.4; RR, 1.15 [95% CI, 1.09–1.21]), and Hispanic (264.4 versus 235.9; RR, 1.12 [95% CI, 1.08–1.16]) populations (Table 2). For both heart disease and cerebrovascular disease deaths, the interaction term for each racial/ethnic group (versus non-Hispanic White people) and year was statistically significant (P<0.001), indicating that the non-Hispanic Black, non-Hispanic Asian, and Hispanic populations each experienced a larger relative increase in deaths compared with non-Hispanic White people during the pandemic (2020 versus 2019).
Table 2.
Heart Disease and Cerebrovascular Disease Deaths by Race/Ethnicity (2020 Versus 2019)
Discussion
In the United States, across all racial and ethnic groups, heart disease and cerebrovascular disease deaths were higher after the onset of the COVID-19 pandemic between the months of March and August in 2020 relative to corresponding months in 2019. Black, Hispanic, and Asian populations each experienced a ≈20% relative increase in heart disease deaths, and a ≈13% relative increase in cerebrovascular disease deaths, during the pandemic. The increase in deaths caused by heart disease and cerebrovascular disease was significantly more pronounced among these groups compared with the non-Hispanic White population.
The racial and ethnic disparities in cardiovascular deaths that have emerged amid the COVID-19 pandemic are concerning. Although the direct toll of COVID-19 on Black and Hispanic adults as well as subgroups of the Asian population has been substantial,6–10,22,23 the marked rise in heart disease and cerebrovascular disease deaths suggests that these groups have also disproportionately been impacted by the indirect effects of the pandemic. Disruptions in access to health care services during the pandemic may have had a larger impact on the health outcomes of Black and Hispanic individuals, as these populations have a higher burden of cardiovascular risk factors, including hypertension,24 obesity,25 and diabetes,26 as well as cardiovascular disease. At the same time, the strain imposed on already resource-constrained health care systems in these communities may have led to issues in care delivery, such as delays in access to hospital services, the deferral of cardiovascular procedures, and the delivery of suboptimal inpatient care for non–COVID-19 conditions.27–29
The avoidance of health care systems has likely also played a role in the disproportionate rise in cardiac and cerebrovascular deaths among diverse populations, particularly during the early phase of the pandemic, when less was known about severe acute respiratory syndrome coronavirus 2 (SARS-CoV2).14 Because COVID-19 case rates have been highest in Black and Hispanic communities,6–9 individuals residing in these areas may have been more reluctant to seek hospital care for acute conditions. For example, a recent survey by the American Heart Association found that 41% of Hispanic Americans and 33% of Black Americans would stay at home if they thought they were experiencing a heart attack or stroke because of fear of exposure to COVID-19 at the hospital.30 Although the use of telemedicine increased during the early phase of the COVID-19 pandemic to bridge gaps in care, Black, Hispanic, and Asian patients have experienced unequal access to video telemedicine, and these services alone may not be adequate for acute conditions.31 Overall, our data highlight the urgent need to improve public health messaging and provide reassurance that hospitals are safe places to receive care.
The pandemic has also impacted the social determinants of health associated with cardiovascular risk.15–17 Racial and ethnic minority groups disproportionately experience poverty in the United States,32 and 60% of Black and 72% of Hispanic households reported serious financial problems during the pandemic, compared with only 36% of White households.33 As a result of financial strain and job losses, Black and Hispanic households have experienced large increases in housing and food insecurity.34 Communities of color have also disproportionately been exposed to psychosocial stressors associated with the pandemic.16,35 These social risk factors, which collectively worsened for Black and Hispanic communities during the pandemic, have likely contributed to the disparate rise in cardiovascular deaths in these groups. The ensuing socioeconomic repercussions of the pandemic, coupled with delays in care, may also explain why heart disease and cerebrovascular disease deaths increased again for some racial/ethnic groups in July and August 2020.
Policy-level factors may have also contributed to worse cardiovascular outcomes during the pandemic. In early 2020, just before the onset of the US pandemic, the Trump administration implemented a revised “public charge” immigration rule. Under this policy, legal immigrants who used public benefits from the government, such as Medicaid insurance or the Supplemental Nutrition Assistance Program, or were in poor health could be at risk of being denied permanent residency status.36 As a result, Hispanic and Asian immigrant families may have avoided seeking care for non—COVID-19–related illnesses, such as cardiovascular disease, because of concerns related to this policy.8,37,38 The extent to which the avoidance of health care systems, either because of fear of contracting COVID-19 or immigration concerns, contributed to the increase in heart disease and cerebrovascular deaths observed in our study remains an important area for future study.
Limitations
This study has limitations. First, our analysis was based on provisional death counts from the NCHS, which may be incomplete in recent weeks because of reporting delays. To minimize the impact of reporting delays, we analyzed data only through August 2020. Second, although our analysis only included underlying causes of death as a result of heart or cerebrovascular diseases, and excluded underlying causes as a result of COVID-19, it is possible that undiagnosed cases of COVID-19 partially contributed to the increase in deaths. However, our analysis is consistent with observations from other nations, such as England and Wales, that have also experienced an increase in cardiovascular deaths caused by the indirect effects of the pandemic.39,40 Third, the identification of race and ethnicity relied on death certification information, which may have been misclassified.
Conclusions
During the COVID-19 pandemic in the United States, Black, Asian, and Hispanic populations experienced a disproportionate rise in deaths caused by heart disease and cerebrovascular disease compared with the non-Hispanic White population. These findings suggest that Black, Asian, and Hispanic populations have been most impacted by the indirect effects of the pandemic. Public health and policy strategies are urgently needed to mitigate the short- and long-term adverse effects of the pandemic on the cardiovascular health of diverse populations.
Sources of Funding
This work was funded by the National Heart, Lung, and Blood Institute at the National Institutes of Health (K23HL148525).
Disclosures
Dr Wadhera receives research support from the National Heart, Lung, and Blood Institute (grant K23HL148525) at the National Institutes of Health. He serves as a consultant for Abbott outside the submitted work. Dr Figueroa receives research support from the Commonwealth Fund, the Robert Wood Johnson Foundation, Arnold Ventures, Harvard Center for AIDS Research, and the Mass Consortium for Pathogen Readiness. Dr Rodriguez has received consulting fees from Novartis, Janssen, NovoNordisk, and HealthPals, unrelated to this work. Dr Yeh receives research support from the National Heart, Lung, and Blood Institute (R01HL136708) and the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology; receives personal fees from Biosense Webster; and receives grants and personal fees from Abbott Vascular, AstraZeneca, Boston Scientific, and Medtronic, outside the submitted work. Dr Maddox receives research support from the National Heart, Lung, and Blood Institute (R01HL143421) and National Institute on Aging (R01AG060935). The other authors report no conflicts.
Supplemental Materials
Data Supplement Table I
Data Supplement Figure I
Supplementary Material
Nonstandard Abbreviations and Acronyms
- COVID-19
- Coronavirus disease 2019
- NCHS
- National Center for Health Statistics
The Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/CIRCULATIONAHA.121.054378.
For Sources of Funding and Disclosures, see page 2353.
Contributor Information
Jose F. Figueroa, Email: Jfigueroa@hsph.Harvard.edu.
Fatima Rodriguez, Email: frodrigu@stanford.edu.
Michael Liu, Email: liu.michael222@gmail.com.
Wei Tian, Email: wtian@bidmc.harvard.edu.
Dhruv S. Kazi, Email: dkazi@bidmc.harvard.edu.
Yang Song, Email: ysong5@bidmc.harvard.edu.
Robert W. Yeh, Email: ryeh@bidmc.harvard.edu.
Karen E. Joynt Maddox, Email: kjoyntmaddox@wustl.edu.
References
- 1.Baum A, Schwartz MD. Admissions to Veterans Affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020;324:96–99. doi:10.1001/jama.2020.9972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, Januzzi JL, Butler J, Adler DS, Solomon SD, et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76:280–288. doi: 10.1016/j.jacc.2020.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gluckman TJ, Wilson MA, Chiu ST, Penny BW, Chepuri VB, Waggoner JW, Spinelli KJ. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020;5:1419–1424. doi: 10.1001/jamacardio.2020.3629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, Ambrosy AP, Sidney S, Go AS. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630 [DOI] [PubMed] [Google Scholar]
- 5.Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS, Yeh RW. Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am Coll Cardiol. 2021;77:159–169. doi: 10.1016/j.jacc.2020.10.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, Shen C. Variation in COVID-19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Price-Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid-19. N Engl J Med. 2020;382:2534–2543. doi: 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Figueroa JF, Wadhera RK, Lee D, Yeh RW, Sommers BD. Community-level factors associated with racial and ethnic disparities in COVID-19 rates in Massachusetts. Health Aff (Millwood). 2020;39:1984–1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Figueroa JF, Wadhera RK, Mehtsun WT, Riley K, Phelan J, Jha AK. Association of race, ethnicity, and community-level factors with COVID-19 cases and deaths across U.S. counties. Healthc (Amst). 2021;9:100495. doi: 10.1016/j.hjdsi.2020.100495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodriguez F, Solomon N, de Lemos JA, Das SR, Morrow DA, Bradley SM, Elkind MSV, Joseph I, Williams H, Holmes D, et al. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the American Heart Association’s COVID-19 Cardiovascular Disease Registry [published online November 17, 2020]. Circulation. 2020. 10.1161/CIRCULATIONAHA.120.052278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karan A, Wadhera RK. Healthcare system stress due to Covid-19: evading an evolving crisis. J Hosp Med. 2021;16:127. doi: 10.12788/jhm.3583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehrotra A, Chernew M, Linetsky D, Hatch H, D C, Scheider E. The Impact of the COVID-19 Pandemic on Outpatient Visits: Changing Patterns of Care in the Newest COVID-19 Hot Spots. 2020. The Commonwealth Fund; https://www.commonwealthfund.org/publications/2020/aug/impact-covid-19-pandemic-outpatient-visits-changing-patterns-care-newest. Accessed October 13, 2020. [Google Scholar]
- 13.Young MN, Iribarne A, Malenka D. COVID-19 and cardiovascular health: this is a public service announcement. J Am Coll Cardiol. 2021;77:170–172. doi: 10.1016/j.jacc.2020.11.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD, et al. Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. doi: 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wadhera RK, Wang Y, Figueroa JF, Dominici F, Yeh RW, Joynt Maddox KE. Mortality and hospitalizations for dually enrolled and nondually enrolled Medicare beneficiaries aged 65 years or older, 2004 to 2017. JAMA. 2020;323:961–969. doi: 10.1001/jama.2020.1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stress and Health Disparities. 2017. American Psychological Association; https://www.apa.org/pi/health-disparities/resources/stress-report.pdf. Accessed April 12, 2021. [Google Scholar]
- 17.Mensah GA. Socioeconomic status and heart health-time to tackle the gradient. JAMA Cardiol. 2020;5:908–909. doi: 10.1001/jamacardio.2020.1471 [DOI] [PubMed] [Google Scholar]
- 18.Provisional Death Counts for Coronavirus Disease (COVID-19): Index of COVID-19 Surveillance and Ad-hoc Data Files. 2021. National Center for Health Statistics; https://www.cdc.gov/nchs/covid19/covid-19-mortality-data-files.htm. Accessed January 8, 2021. [Google Scholar]
- 19.COVID-19 Death Data and Resources. 2021. National Center for Health Statistics; https://www.cdc.gov/nchs/nvss/covid-19.htm#understanding-death-data-quality. Accessed April 19, 2021. [Google Scholar]
- 20.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090 [DOI] [PubMed] [Google Scholar]
- 21.Lumley T, Kronmal R, Ma S. Relative Risk Regression in Medical Research: Models, Contrasts, Estimators, and Algorithm. 2006. UW Biostatistics Working Paper Series; https://biostats.bepress.com/cgi/viewcontent.cgi?article=1128&context=uwbiostat. Accessed April 13, 2021. [Google Scholar]
- 22. Deleted in proof.
- 23.Chu JN, Tsoh JY, Ong E, Ponce NA. The hidden colors of coronavirus: the burden of attributable COVID-19 deaths. J Gen Intern Med. 2021;36:1463–1465. doi: 10.1007/s11606-020-06497-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muntner P, Hardy ST, Fine LJ, Jaeger BC, Wozniak G, Levitan EB, Colantonio LD. Trends in blood pressure control among US adults with hypertension, 1999-2000 to 2017-2018. JAMA. 2020;324:1190–1200. doi: 10.1001/jama.2020.14545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Racial and Ethnic Disparities in Heart Disease. Centers for Disease Control and Prevention. Health, United States Spotlight Web Site. 2019. https://www.cdc.gov/nchs/hus/spotlight/HeartDiseaseSpotlight_2019_0404.pdf. Accessed February 14, 2021.
- 26.Cheng YJ, Kanaya AM, Araneta MRG, Saydah SH, Kahn HS, Gregg EW, Fujimoto WY, Imperatore G. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA. 2019;322:2389–2398. doi: 10.1001/jama.2019.19365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asch DA, Sheils NE, Islam MN, Chen Y, Werner RM, Buresh J, Doshi JA. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021;181:471–478. doi: 10.1001/jamainternmed.2020.8193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ro R, Khera S, Tang GHL, Krishnamoorthy P, Sharma SK, Kini A, Lerakis S. Characteristics and outcomes of patients deferred for transcatheter aortic valve replacement because of COVID-19. JAMA Netw Open. 2020;3:e2019801. doi: 10.1001/jamanetworkopen.2020.19801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Uy-Evanado A, Chugh HS, Sargsyan A, Nakamura K, Mariani R, Hadduck K, Salvucci A, Jui J, Chugh SS, Reinier K. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin Electrophysiol. 2021;7:6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fueled by COVID-19 Fears, Approximately Half of Hispanics and Black Americans Would Fear Going to the Hospital if Experiencing Symptoms of a Heart Attack or Stroke. 2020. American Heart Association; https://newsroom.heart.org/news/fueled-by-covid-19-fears-approximately-half-of-hispanics-and-black-americans-would-fear-going-to-the-hospital-if-experiencing-symptoms-of-a-heart-attack-or-stroke#_ftn2. Accessed February 20, 2021. [Google Scholar]
- 31.Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, Snider C, Chokshi NP, Eneanya ND, Takvorian SU, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2031640. doi: 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poverty Rate by Race/Ethnicity. 2019. Kaiser Family Foundation; https://www.kff.org/other/state-indicator/poverty-rate-by-raceethnicity/. Accessed April 12, 2021. [Google Scholar]
- 33.The Impact of Coronavirus on Households, by Race/Ethnicity. 2020. Harvard T.H. Chan School of Public Health; https://drive.google.com/file/d/1XoV6pqzvtag4E9YQeLRTvHaWAlN-s830/view. Accessed April 12, 2021. [Google Scholar]
- 34.Housing Insecurity by Race and Place During the Pandemic. 2020. Center for Economic and Policy Research; https://cepr.net/report/housing-insecurity-by-race-and-place-during-the-pandemic/. Accessed April 5, 2021. [Google Scholar]
- 35.Panchal N, Kamal R, Cox C, Garfield R. The Implications of COVID-19 for Mental Health and Substance Use. 2021. Kaiser Family Foundation; https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/. Accessed April 20, 2021. [Google Scholar]
- 36.Khalid NS, Moore A. Immigration and Compliance Briefing: COVID-19 Summary of Government Relief and Potential “Public Charge Rule” Impact on Nonimmigrant and Immigrant Visa Applications. 2020. National Law Review; https://www.natlawreview.com/article/immigration-and-compliance-briefing-covid-19-summary-government-relief-and-potential. Accessed February 14, 2021. [Google Scholar]
- 37.Page KR, Venkataramani M, Beyrer C, Polk S. Undocumented U.S. immigrants and Covid-19. N Engl J Med. 2020;382:e62. doi: 10.1056/NEJMp2005953 [DOI] [PubMed] [Google Scholar]
- 38.Sommers BD, Allen H, Bhanja A, Blendon RJ, Orav EJ, Epstein AM. Assessment of perceptions of the public charge rule among low-income adults in Texas. JAMA Netw Open. 2020;3:e2010391. doi: 10.1001/jamanetworkopen.2020.10391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu J, Mamas MA, Mohamed MO, Kwok CS, Roebuck C, Humberstone B, Denwood T, Luescher T, de Belder MA, Deanfield JE, et al. Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart. 2021;107:113–119. doi: 10.1136/heartjnl-2020-317912 [DOI] [PubMed] [Google Scholar]
- 40.Pell R, Fryer E, Manek S, Winter L, Roberts ISD. Coronial autopsies identify the indirect effects of COVID-19. Lancet Public Health. 2020;5:e474. doi: 10.1016/S2468-2667(20)30180-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


