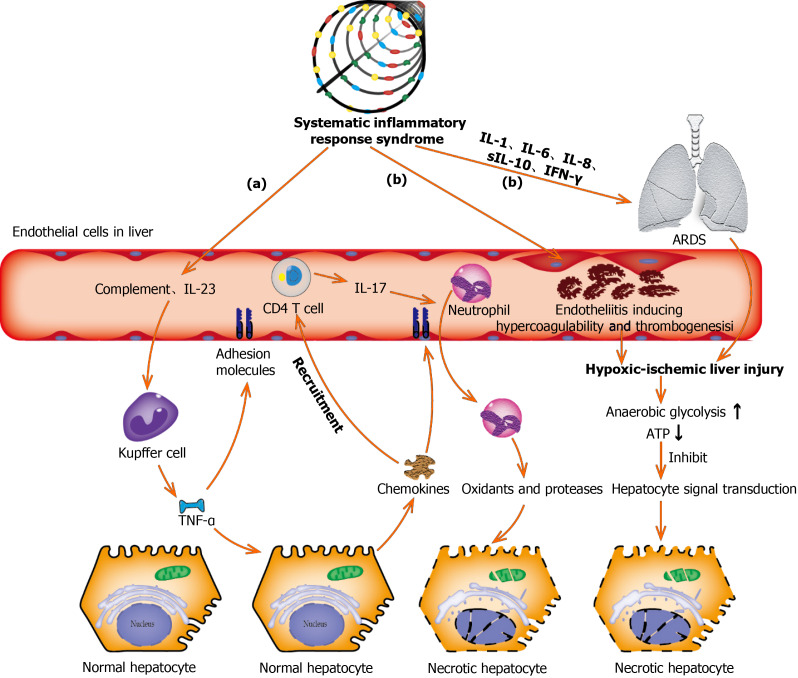
Figure 3.
Underlying molecular mechanisms of coronavirus disease-19-associated liver injury caused by systematic inflammatory response syndrome and hypoxic ischemia. (a): Complement and interleukin-23 are released into the blood during the systemic inflammation, which subsequently activate Kupffer cells and induce their production of tumor necrosis factor α (TNF-α). As a pro-inflammatory cytokine, TNF-α aggravates the inflammation responses by up-regulating the expression of endothelial cell adhesion molecules and inducing hepatocytes to secrete chemokines. Under the induction of chemokines, CD4 T cells and neutrophils are rapidly recruited to the liver, in which CD4 T cells assist mucosal molecules to promote neutrophils into the liver parenchyma. Finally, neutrophils directly damage liver cells by releasing oxidants and proteases, leading to necrotic cell death; (b): Acute respiratory distress syndrome and endotheliitis are the two main causes leading to hypoxic-ischemic liver injury in the period of systematic inflammatory response syndrome. Increased anaerobic glycolysis leads to a decrease in ATP production, which ultimately leads to the death of hepatocytes by inhibiting hepatocyte signal transduction. ARDS: Acute respiratory distress syndrome; TNF-α: Tumor necrosis factor α; IL: Interleukin; IFN-γ: Interferon-γ.