Abstract
This report provides perspectives concerning dual roles of serum ferritin as a measure of both iron status and of inflammation. We suggest benefits of a lower range of serum ferritin as has occurred for total serum cholesterol and fasting blood glucose levels. Observations during a prospective randomized study using phlebotomy in patients with peripheral arterial disease (PAD) offered unique insights into dual roles of serum ferritin both as an iron status marker and acute phase reactant. Robust positive associations between serum ferritin, interleukin 6 [IL-6], tissue necrosis factor-alpha (TNF-a), and high sensitivity C-reactive protein (hsCRP) were discovered. Elevated serum ferritin and IL-6 levels associated with increased mortality and with reduced mortality at ferritin levels < 100 ng/mL. Epidemiologic studies demonstrate similar outcomes. Extremely elevated ferritin and IL-6 levels also occur in individuals with high mortality due to SARS-CoV-2 infection. Disordered iron metabolism reflected by a high range of serum ferritin level signals disease severity and outcomes. Based upon experimental and epidemiologic data, we suggest testing the hypotheses that optimal ferritin levels for cardiovascular mortality reduction range from 20—100 ng/mL with % transferrin levels from 20–50%, to ensure adequate iron status and that ferritin levels above 194 ng/mL associate with all-cause mortality in population cohorts.
Keywords: ferritin, iron metabolism, inflammatory cytokines, atherosclerosis, Covid-19, hyperferritinemic syndromes
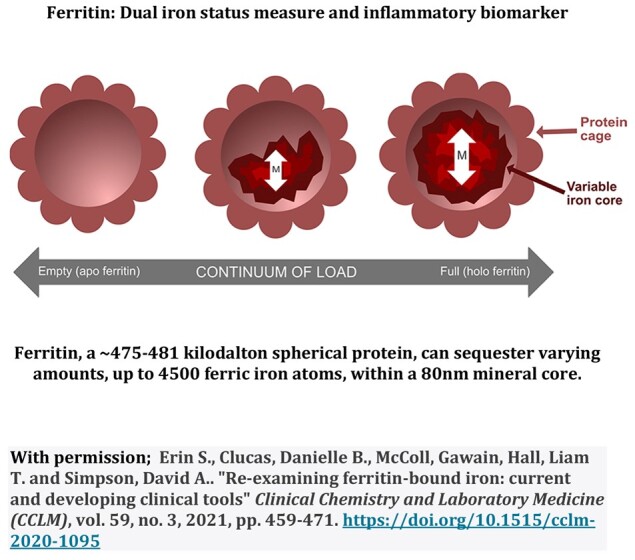
Graphical Abstract
Graphical Abstract.