Fig 1. The role of obesity and exercise on perivascular adipose tissue induced aortic (dys)function.
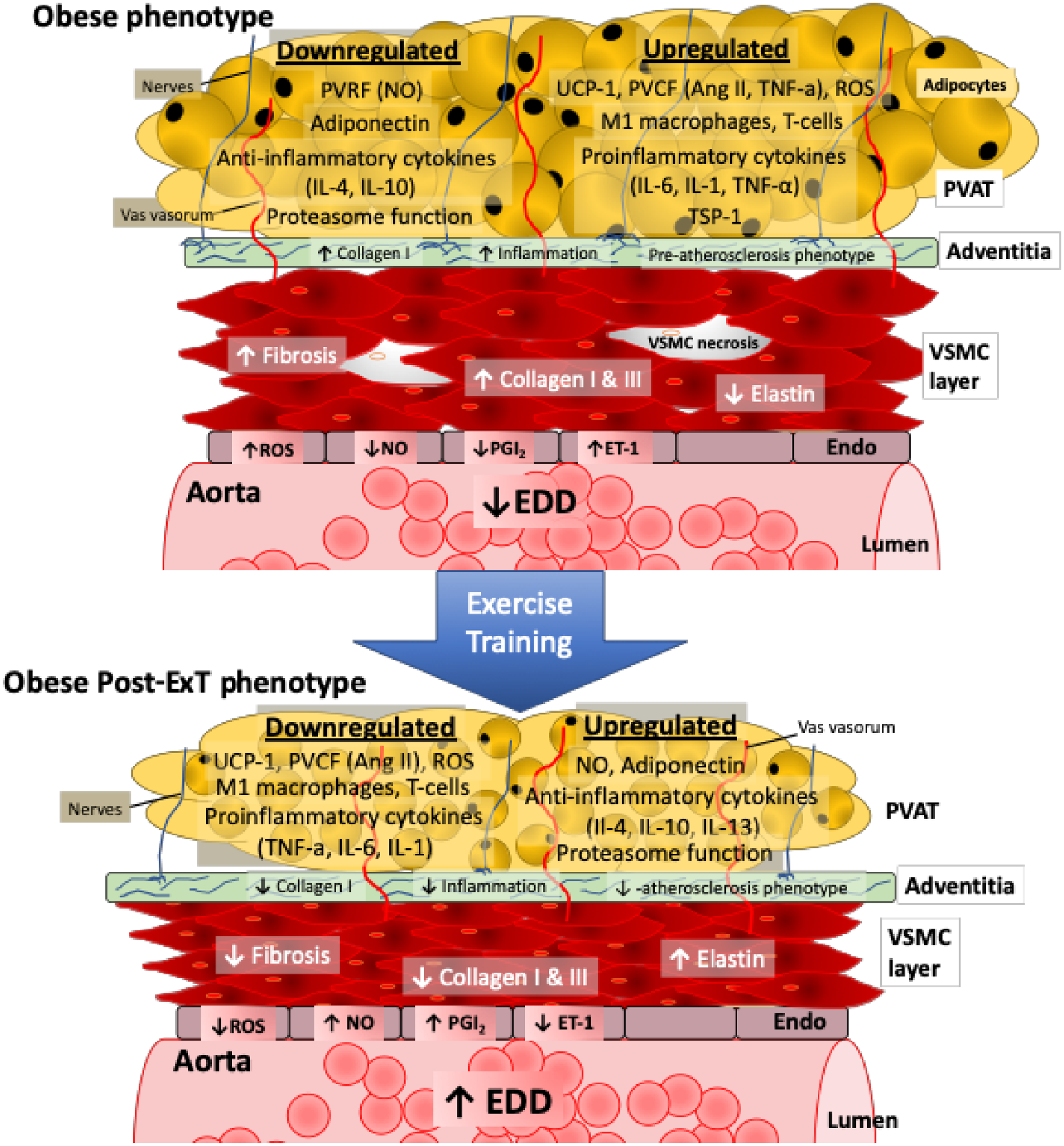
With obesity the PVAT becomes more white (decreased UCP-1) and dysfunctional, reflected by a greater infiltration of M1 macrophages and T-cells with a corresponding increase in pro-inflammatory cytokines, and ROS coupled with a downregulation in proteasome function and anti-inflammatory cytokines. This dysfunctional PVAT phenotype results in a decrease in PVRF (NO, adiponectin) and an increase in PVCF (ET-1, Ang II). As PVAT is closely positioned to the vascular adventitia without an anatomic barrier, it can directly communicate with vascular cells by transferring cytokines. Further, cytokines can be transferred through the vasa vasorum to VSMCs. As such, obesity increases collagen 1 content and inflammation to promote a pre-atherosclerotic phenotype in the adventitia. Significant changes also occur to the VSMC, reflected by an increase in fibrosis and collagen content, with a reduction in elastin content with more necrotic cells. In the endothelium, there is an impaired release of NO and PGI2 with an increase in ROS, and ET-1, which leads to reduced aortic EDD and increased stiffness. However, when obese animals under exercise training (blue arrow) the dysfunctional PVAT is partly reversed. That is obese-ExT PVAT reflects a more brown like phenotype, with reduced pro-inflammatory cytokines, ROS, and increased anti-inflammatory cytokines and proteasome function. Ultimately, exercise training improves PVRF and reduces PVCF so that aortic EDD and stiffness are improved.
Abbreviations: PVAT, perivascular adipose tissue; VSMCs, vascular smooth muscles cells; Endo, endothelium; EDD, endothelial dependent dilation; PVRF, perivascular derived relaxation factor; PVCF, perivascular derived contraction factors; NO, nitric oxide; IL-1, interlukin-1; IL-4, interlukin-4; IL-6, interlukin-6; IL-10, interlukin-10; IL-13, interlukin-13; UCP-1, uncoupling protein 1; Ang II, angiotensin II; TNF-a, Tumor necrosis factor-alpha; ROS, reactive oxygen species; TSP-1, thrombospondin-1; PGI2, prostacyclin; ET-1, endothelial-1
