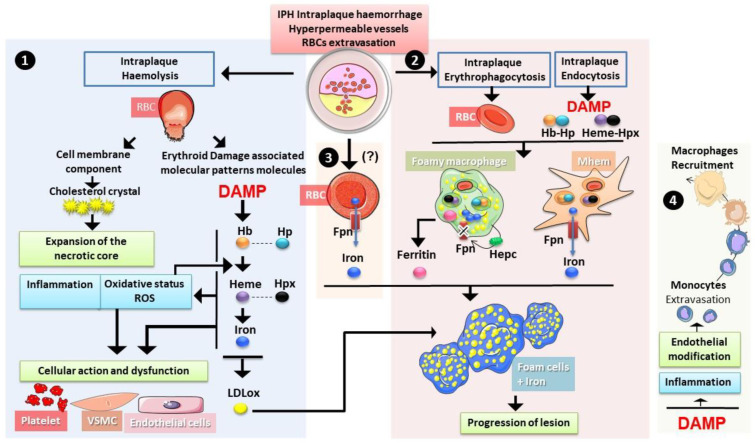
Figure 6.
Erythrocytes in intraplaque haemorrhage. During intraplaque haemolysis 1. and rupture lysis, RBCs liberate both cholesterol and erythroid damage-associated signalling molecule patterns ((DAMPs) haemoglobin Hb, heme and iron), both contributing to the expansion of the necrotic core and to the increase in oxidative stress and inflammation. Such changes could have an impact on the function of endothelial cells, vascular smooth muscle cells (VSMC) and platelets. Haemoglobin and iron can promote the oxidation of LDL particles accelerating the foam cell differentiation. Erythrophagocytosis as well as endocytosis of heme/hemopexin and haemoglobin/haptoglobin complexes 2. also occurs in the plaque with an important role of macrophages. The haemorrhage-associated macrophages (Mhem) are prone to recycling iron from both erythrophagocytosis and heme containing-complexes endocytosis, whereas foamy macrophages (Mox) tend to accumulate iron with lipids. Autocrine expression of hepcidin (Hepc) seems to play a role in iron retention. Ferritin secretion by these cells has been reported. Another source of iron could exist directly from erythrocytes via the expression of ferroportin (Fpn) 3. Both iron and ferritin present in the plaque with oxidised low-density lipoprotein (oxLDL) could trigger the formation of foam cells, promoting the progression of the lesion and the instability of the plaque. In addition, 4. erythroid DAMPs were shown to increase expression of adhesion molecules by endothelial cells and to have proinflammatory effects. Both phenomena contribute to the recruitment of more monocytes/macrophages in the plaque.