Abstract
Digital technologies have the potential to empower individuals with autism and their families. The COVID-19 pandemic emphasized and accelerated the drive towards technology for information, communication, training, clinical care and research, also in the autism community. However, 95% of individuals with autism live in low- and middle-income countries (LMIC) where access to electricity, internet and the ever-increasing range of digital devices may be highly limited. The World Bank coined the term ‘the digital divide’ to describe the disparities in access to digital technologies between high-income and LMIC contexts. Here we evaluated the feasibility of six emerging technologies for autism spectrum disorders, and reflected on key considerations for implementation in LMIC contexts to ensure that we do not inadvertently widen the pre-existing digital divide.
Keywords: Digital technology, Autism spectrum disorder, Digital disparities, Low-resource contexts, Africa, India
Introduction
Autism spectrum disorders (ASD) are neurodevelopmental disorders characterised by a wide range of features, including difficulty with social interaction and communication, restricted interests, and stereotyped behaviours (American Psychiatric Association, 2013). As a group people with ASD have a broad range of abilities, allowing some to lead independent and productive lives with varying levels of support, while others are severely affected by manifestations that may persist throughout the lifespan (Farley et al., 2009). However, there is growing evidence that early identification and treatment and a range of other interventions can reduce the manifestations and improve the functional outcomes of ASD for many affected individuals (Bradshaw et al., 2015; Dawson et al., 2012; Rogers & Dawson, 2010).
Given the global prevalence of ASD estimated in excess of 1% (Elsabbagh et al., 2012; Fombonne, 2009), the World Health Organization recognised ASD as a global public health concern and a major cause of disease burden (World Health Organization, 2013). However, 95% of individuals with ASD and other developmental disabilities live in low- or middle-income countries (LMIC) (Franz et al., 2017; Olusanya et al., 2018, 2020), where they are typically either undiagnosed or diagnosed much later than those living in high-income countries (HIC), and where they may receive no or very limited intervention and support (Daley, 2004; Lagunju et al., 2014; Pillay et al., 2021). Disparities in access to ASD screening, diagnosis, and treatment in low-resourced communities exist globally (Patel et al., 2008). Factors such as symptom severity, geographic location, socio-economic status (SES), race/ethnicity and culture impact both the age of first assessment and subsequent intervention (Lagunju et al., 2014; Williams et al., 2014).
Over the last 30 years, the rates of ASD and other disabilities have increased most significantly in sub-Saharan Africa (SSA) and in South-East Asia (Olusanya et al., 2018) where the majority of communities face significant challenges to access skilled professionals and appropriate services (de Vries, 2016; Franz et al., 2017; Saxena et al., 2007). Families who live in remote, low-resource areas typically have to travel considerable distances, sometimes for hours or days, for their children and adult family members to receive the services they need (Divan et al., 2012; Mahapatra et al., 2019). The lack of reliable transport infrastructure, shortage of trained professionals and lengthy waiting times may result in these visits taking days rather than hours (Daley, 2004; Durkin et al., 2015). Compounding the infrastructural challenges, people living in rural or remote areas of LMIC typically also have limited awareness of and poor knowledge about ASD. This, unfortunately, also includes educational and healthcare professionals (Bakare et al., 2009; de Vries, 2016; Franz et al., 2017; Ruparelia et al., 2014). Lack of knowledge about ASD combined with local cultural and traditional beliefs contribute to social stigma and discrimination, often depriving these already disadvantaged groups of opportunities to improve their health, education and community participation (Harrison et al., 2017; Harrison et al., 2017; Keusch et al., 2006; Michels et al., 2006).
Apart from gaps in clinical care and knowledge, there is also a significant disparity in the proportion of ASD research that has been conducted in LMIC as opposed to HIC settings. Taking sub-Saharan Africa as example, in a comprehensive scoping review Franz et al. (2017) showed that less than 1% of global ASD research had taken place in Africa. The review by Franz did not directly compare the proportion of research in all LMIC to research from all HIC, but it was clear that the majority of ASD research to date has come from HIC where the minority of people with ASD live.
Emerging Digital Technologies for Autism Spectrum Disorder
In recent years, there has been a rapid increase in utilising technology for identification, intervention and training to address the various challenges in delivering health and other care to families living with ASD (Grynszpan et al., 2014; Odom et al., 2015; Ploog et al., 2013). Unlike traditional service delivery models (involving highly skilled professionals in one-to-one, in-person sessions), technology allows the possibility to increase access on a large scale at relatively low cost, and to utilise a diverse workforce in local settings where these services are poor or non-existent. Technology therefore has the potential to reduce the disparities in service delivery between HIC and LMIC communities (Naslund et al., 2017).
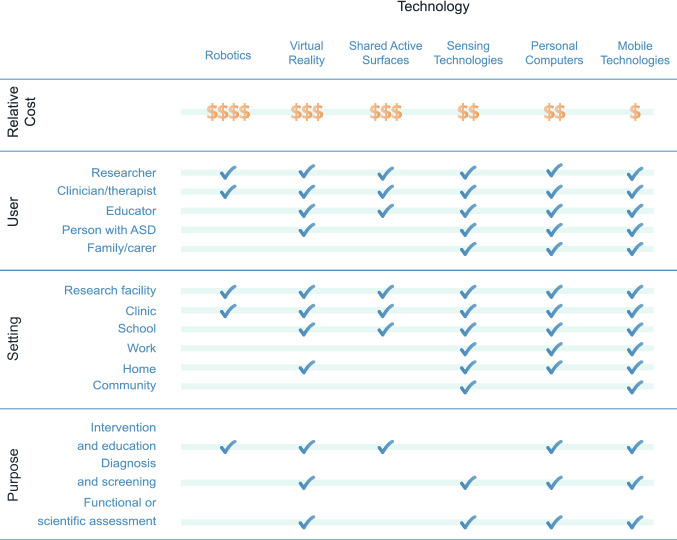
In a comprehensive review of technologies for ASD, Kientz et al. (2014) identified six main emerging interactive technology platforms (personal computers, robotics, virtual reality, shared active surfaces, sensing technologies, and mobile devices) and used a classification scheme to review these key technologies. The classification included examination of the technology in relation to domain of interest (e.g. social/emotional or language/communication), purpose (e.g. functional assessment or diagnosis/screening), the target end user (e.g. person with ASD or family/caregiver), setting (e.g. home or school), nature of the empirical support (e.g. descriptive or experimental research) and technology maturity (e.g. design, prototype or publicly available). Odom et al., (2015) used similar criteria to examine technology for adolescents with ASD and presented a conceptual framework that identified the ‘human’ (user), ‘activity’ (purpose) and ‘technology’ as key constructs in relation to the ‘context’ (home, school, community). Building on these earlier reviews, below we present a brief summary of the same technologies and their purpose, settings for use, users and relative cost, using the Kientz et al., (2014) and Odom et al., (2015) frameworks. See Fig. 1 for a visual summary.
Fig. 1.
Summary of emerging technologies for ASD in terms of their purpose, settings for use, potential users, and relative cost
Personal Computers
Personal Computers (PCs) are found in most homes, schools, universities, offices and shops in high-income countries (International Telecommunication Union (ITU), 2010). Computer-based interventions for autistic children have been known since the early 1970s (Colby, 1973; Colby & Smith, 1971) and used by individuals with ASD and their caregivers to address a wide variety of areas that require attention, from early identification to rehabilitation in a variety of settings (Fig. 1). Today, online platforms (e.g. https://babynavigator.com, Florida State University, 2021) enable parents to track their child’s development prompting them into action if a developmental delay is suspected. Web-based courses (e.g. www.autismnavigator.com, Wetherby et al., n.d.) provide professionals and families access to the latest evidence-based diagnostic tools and intervention techniques. Computer-based training of community-based health care providers has been shown to be as effective as in-person didactic training (Vismara et al., 2009). Even without access to the internet, standard desktop computers with audio-visual presentation software (e.g. PowerPoint) of ASD-related educational material for healthcare professionals, teachers and carers can improve knowledge about ASD. According to Statista (2020a) the average selling price of personal computers in 2019 was US$632 with prices ranging from around US$150 (for refurbished PCs) to several thousand dollars (Statista, 2020a).
Robotics
Robot-based diagnosis and treatment for ASD has been a rapidly developing area of research in HICs for more than a decade (Dautenhahn & Werry, 2004; Scassellati, 2007). Researchers investigating robotic interventions for ASD typically report increased engagement and levels of attention when robots are part of the interaction, including individuals who routinely are unlikely or unwilling to interact socially with their healthcare provider and teachers (Diehl et al., 2012; Scassellati, 2007). Robots have been designed to address a variety of behavioural objectives such as joint attention (Kumazaki et al., 2018), social interaction and communication skills (David et al., 2020; Kim et al., 2012) in school, clinic or home settings (Dickstein-Fischer et al., 2011, 2017). However, most robotic interventions for ASD have not yet progressed passed the developmental stage and require skilled operators. As a result, their use at present is mostly limited to research and specialised clinical settings. Their costs are substantial, ranging from hundreds to upwards of thousands of U.S. dollars (Boccanfuso et al., 2017; Dickstein-Fischer et al., 2011, 2018) making them the most expensive of the technologies discussed here (Fig. 1).
Virtual Reality
Virtual Reality (VR) technologies provide realistic safe and repeatable simulated real-world environments well-suited for teaching individuals with ASD the necessary skills required for independent living and employment (Parsons et al., 2004; Standen & Brown, 2005). VR based interventions for ASD have been used for improving social skills (Kandalaft et al., 2013), teaching individuals how to navigate and cross streets (Saiano et al., 2015), use public transport or find a table in a café or restaurant (Parsons et al., 2006). Virtual learning environments have been used for distance education to teach social and communication skills in low or under-resourced areas (Stichter et al., 2014). Head-mounted VR devices (like the Oculus Quest for example—https://www.oculus.com/compare/) are easily portable, not difficult to operate and can therefore be used in most settings and cost around US$300 (https://www.oculus.com/compare/, Facebook Technologies, 2021) for the hardware alone. Most state-of-the-art VR technologies for ASD, however, require powerful computers with advanced specifications and access to high speed broadband internet costing thousands rather than hundreds of US dollars (Fig. 1).
Shared Active Surfaces
Collaborative Interface (CI) or Shared Active Surface (SAS) technologies are large touch-screen computer-based interactive surfaces that can be placed on tabletops, be operated by more than one person simultaneously and therefore be utilized to enhance social and collaborative face-to-face interaction among multiple users (Dietz & Leigh, 2001; Travers & Fefer, 2016) Several published studies have documented the potential of using SAS technologies and cooperative games to improve social skills such as eye contact, sharing of emotions, showing interest toward a partner, and collaborative play in children with ASD (Bauminger-Zviely et al., 2013; Ben-Sasson et al., 2013; Gal et al., 2016). Multi-user surfaces are not easily transportable due to their size and weight. By its nature, touchscreen devices are not hardwearing and therefore susceptible to damage that could render them unserviceable and very expensive to repair or replace. It is possible that this technology could be useful in very specific settings such as specialist schools, clinics or research facilities (Fig. 1). However, they may not represent a very naturalistic opportunity for assessment or intervention for individuals with ASD. Commercially available multi-user touch tables currently cost from US$6,500 excluding any software (POP Communications, 2010).
Sensing Technologies
Sensing technologies (STs) embedded in everyday accessories such as glasses, wrist watches, clothing, or ultra-thin adhesive epidermal patches have been used to collect specific data to identify ASD symptoms (Cabibihan et al., 2017). STs include a variety of devices for tracking eye movement to detect atypical gaze (Constantino et al., 2017; Vidal et al., 2012; Ye et al., 2012), physical activity trackers to detect stereotypical behaviours (Goodwin, et al., 2011; Min & Tewfik, 2010; Sarker et al., 2018), sensors to detect internal state changes related to stress and anxiety (Fletcher et al., 2010; Goodwin et al., 2006), and sensors to detect atypical prosody and speech (Paul et al., 2005; Warren et al., 2010). However, many wearable physiological and physical activity-sensing devices require direct contact with the skin and may not be tolerated by some children with ASD (Cabibihan et al., 2017). Smart watches (e.g. the Apple Watch) are increasingly utilized both for assisting and monitoring individuals with ASD (Koumpouros & Kafazis, 2019) in any setting (Fig. 1). Sensing technologies are relatively expensive. The average selling price of smartwatches is around US$300 (Gartner, 2018; International Data Corporation, 2019) and typically require additional computer software and hardware, as well as highly skilled professionals to analyse and use collected data.
Mobile and Smartphone Technologies
It is estimated that around 74% of the population in HIC and around 45% of those living in LMIC own a smartphone while the estimates for tablet ownership are close to 50% and 20% respectively (Silver, 2019; Statista, 2020b). Even simple features such as task lists, calendars and address book applications can improve the day-to-day independence of school-going young people with ASD (Gentry et al., 2010; Hedges et al., 2018). Smartphone applications can potentially provide parents and carers with objective early screening (Egger et al., 2018; Kanne, et al., 2018) and intervention tools (Law et al., 2018; Parsons et al., 2019; Rogerson et al., 2019). Using online social media platforms (e.g. WhatsApp, Twitter, Facebook) can for some open the door to social engagement and being part of a community (Hedges et al., 2018; van Schalkwyk et al., 2017). The release of the first Apple iPhone in 2007 set in motion the rapidly evolving novel domain of healthcare referred to as ‘mobile health’ or ‘mHealth’. Currently, there are more than 100,000 mHealth applications (‘apps’) available globally for download from app stores (Statista, 2021). Despite a paucity of empirical evidence, Smartphone apps for ASD continue to disrupt older technologies in several areas such as communication devices (e.g. WhatsApp) and access to personal medical information. The average selling price of smartphones in 2020 was US$309 (Statista, 2020b) with a wide range between lower specification smartphones (< US$100) and ultra-premium phones (> US$1,000) (International Data Corporation, 2020). Similar to PCs, mobile and smartphone technologies are used by individuals with ASD as well as their caregivers and service providers in most settings and for a wide variety of objectives but at relatively lower cost than many of the other emerging technologies for ASD (Fig. 1).
The ‘Digital Divide’ Between High-Income and Low/Middle-Income Countries
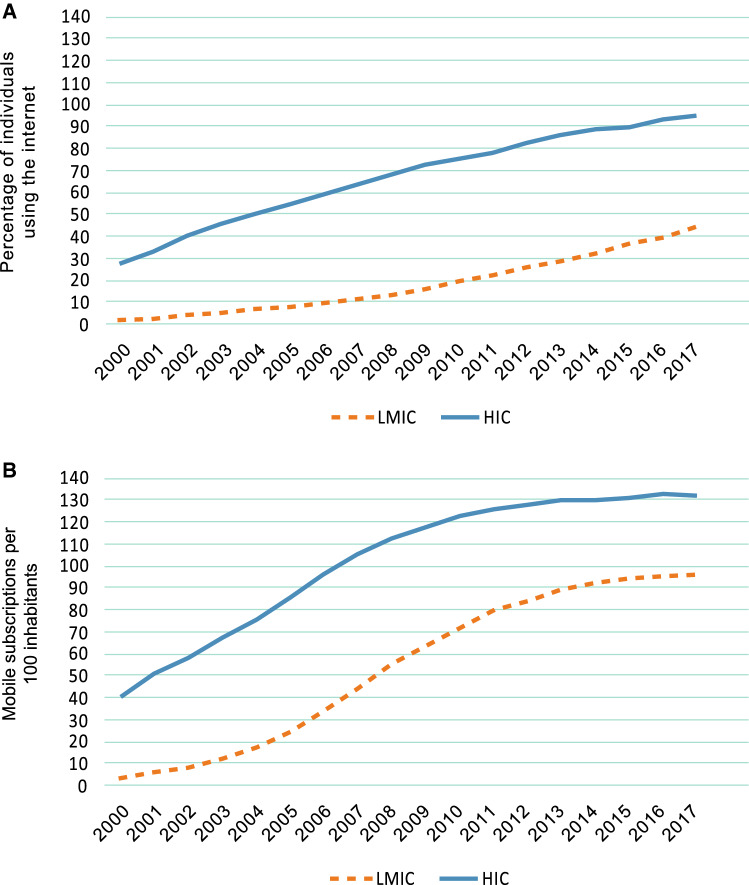
The World Development Report published by the World Bank in 2016 focused on digital technologies in a publication entitled ‘Digital Dividends’ (World Bank, 2016). The report pointed out that digital technologies have spread rapidly across the globe, but that the ‘digital dividends’—the developmental benefits of using these technologies—had lagged behind. The report emphasized that emerging technologies had disproportionately benefited the higher-educated and wealthier sectors of society, and commented that nearly 60% of the world still had no access to the internet. The internet therefore remains unavailable, inaccessible and unaffordable to a majority of the world’s population. “For digital technologies to benefit everyone everywhere therefore requires closing the remaining digital divide, especially in internet access” (World Bank, 2016, p. 2). Figure 2 shows a graphic representation of fixed internet users (panel A) and mobile phone subscriptions (panel B) in HIC and LMIC between 2000 and 2017 (data from ITU, 2019 and World Bank, 2020) to illustrate the digital divide. Panel A shows how internet usage increased significantly from 2000 in HIC and LMIC settings, but indicates that the digital divide had increased, rather than reduced, over time with fewer than 40% of households in LMIC having fixed internet access, in contrast to more than 90% in HIC. Panel B shows that the digital divide has remained across the last 2 decades in terms of mobile/cellular subscriptions, but indicates that both in HIC and LMIC settings there were more than 90 subscriptions to mobile/cellular networks per 100 inhabitants by the end of 2017.
Fig. 2.
Internet users and mobile phone subscriptions in HIC and LMIC between 2000 and 2017 (data from ITU, 2019 and World Bank, 2020). Panel A shows the percentage of households with access to fixed internet; Panel B shows the number of mobile/cellular subscriptions per 100 individuals
The COVID-19 pandemic that swept across the globe from the end of 2019, throughout 2020 and into 2021 very rapidly shifted the majority of the world from in-person interactions towards remote interactions using technology for information, communication, teaching and research, including in the ASD community. A collection of commentaries about the impact of COVID-19 on ASD research (Amaral & de Vries, 2020) showed many examples of technological solutions, pivoting of research towards remote modalities, and so on. However, a few notable examples from lower-resource environments and LMIC expressed concern that the COVID-19 pandemic may simply have magnified pre-existing digital (and social) disparities (see e.g. de Vries et al., and Divan et al., in the Amaral and de Vries commentaries, 2020).
In order to ensure that we do not inadvertently increase the digital divide in the global ASD community, there is therefore a need to reflect on the feasibility of the increasing number and types of digital technologies for ASD. In the implementation science research literature, feasibility is defined as the extent to which a treatment or innovation can be used or carried out by a specific agent or used successfully within a given context (Karsh, 2004; Proctor et al., 2011). Feasibility is conceptually linked to a number of other implementation outcomes, including the accessibility, affordability, acceptability/cultural appropriateness, and scalability of a treatment or innovation. Short definitions of these key implementation science terms as relevant to digital technologies are presented in Table 1.
Table 1.
Implementation constructs evaluated in this study in relation to digital technologies
| Construct | Definition | Reference |
|---|---|---|
| Feasibility | The extent to which a new technology can be used successfully within a given setting | Karsh (2004) |
| Accessibility | The ease or difficulty for users to access a particular technology. Distance is often an important indicator to measure the accessibility of resources | Ye et al. (2019) |
| Affordability | The true cost of implementing a particular technology. The construct depends on the costs of the particular technology, the cost of implementation, and the cost of accessing the technology in a particular location | Proctor et al. (2011) |
| Acceptability and cultural appropriateness | The perceived fit, relevance, or compatibility of the technology to a particular user, provider, community or setting | Proctor et al. (2011) |
| Scalability | The ability of a technology (shown to be efficacious on a small scale and/or under controlled conditions) to be expanded under real world conditions to reach a greater proportion of the eligible population, while retaining effectiveness | Aarons et al. (2017) |
Combining the global drive towards digital technologies for ASD, the fact that the majority of people with ASD live in LMIC, and the pre-existing digital divide as outlined by the World Bank, there is a significant risk that, without due reflection and consideration of the real-world feasibility of technologies, the global ASD community may increase this digital divide, and thus compound the well-known disparities that exist between HIC and LMIC in health, education, social integration and economic outcomes of families who live with ASD.
Here, we therefore set out to evaluate the six key technologies outlined earlier in terms of their overall feasibility for implementation in LMIC and low-resource contexts.
Methods
Study Participants and Procedure
A narrative feasibility evaluation was performed by three reviewers with clinical and research expertise in the use of technologies for ASD in LMIC. Each reviewer was provided with access to a recent review of digital technologies for autism, and to PDFs of all publications summarised in the background review of the six emerging technologies for ASD. After review of the literature each reviewer was asked to provide feasibility ratings of the implementation constructs selected.
Implementation Science Constructs Evaluated
In order to evaluate feasibility, four implementation constructs were selected for this study—acceptability, accessibility, appropriateness and scalability (see Table 1 for definitions). After rating each construct, reviewers were asked to provide an ‘overall feasibility’ judgment incorporating all constructs. In the absence of any existing criteria for feasibility rating of technologies, reviewers were asked to rate constructs as ‘very low’, ‘low’, ‘high’ or ‘very high’. Reviewers were asked to provide comments and a narrative motivation for their ratings. The three reviewers were then asked to reach consensus on their feasibility rating for all categories through an iterative process until consensus was reached. Weighted kappa scores were calculated for initial ratings in relation to consensus ratings. Narrative comments were collated as collective motivation for final ratings.
Results
Feasibility Evaluation of Technologies for ASD in LMIC
Categorical Ratings
Figure 3 shows the consensus rating of each of the technologies in terms of their accessibility, affordability, acceptability/cultural appropriateness, scalability and overall feasibility in LMIC. Individual ratings showed weighted kappa scores of 0.714–1.000 for accessibility, 0.850–1.000 for affordability, 0.615–1.000 for acceptability/cultural appropriateness and 0.850–1.000 for scalability. Overall feasibility showed weighted kappa scores ranging from 0.850–1.000.
Fig. 3.
Feasibility of evidence-based technologies for autism spectrum disorder in low and middle-income countries (LMIC)
Narrative Motivation for Feasibility Ratings
Accessibility
As shown in Fig. 2, the ‘digital divide’ is strongly associated with the income classification of countries, and represents the gap between high-resource and low-resource settings in physical access to ICT and related skills/resources to use these technologies (Dutta et al., 2015; World Bank, 2016). However, access to and usage of technology is also associated with gender, level of education, literacy, urbanisation and socioeconomic status (Alozie & Akpan‐Obong, 2017; World Bank, 2016). In most LMIC, use of ICT is skewed towards young educated males of higher SES living in large towns or cities (Gomez, 2014; Wesolowski et al., 2015; World Bank, 2016). Even within LMIC there are therefore higher- and lower-resourced communities with differential access to technology. Most of the technologies reviewed here require access to reliable power supply. In sub-Saharan Africa 60% of people and in South-East Asia 30% of people do not have direct access to electricity (World Bank, 2016). In addition, health services such as remote consultations utilising interactive video conferencing (telemedicine) depend on access to a PC and reliable internet connection with sufficient speed and bandwidth. Fewer than 25% of households in sub-Saharan Africa own a working computer, and even fewer connect to the internet using fixed (wired) broadband services (Gillwald, 2013; ITU, 2019). Access to PCs is becoming more widespread in LMIC as public access computing venues including libraries and internet cafes are being set up in many towns and villages (Gomez, 2014). In many underserved communities in Africa, mobile phone sharing or informal telecentres (where mobile phones can be used for a fee) are also improving access to ICT services. Close to 70% of people living in the poorest 20% of households globally have access to and are familiar with mobile phones (World Bank, 2016). Familiarity and proficiency with the technology are known to contribute to implementation success of technology-based healthcare initiatives (Zurovac et al., 2011, 2012). For these reasons, consensus ratings for accessibility were ‘very high’ for smartphone-based technologies, ‘high’ for personal computers, ‘low’ for sensing and virtual reality technologies, and ‘very low’ for robotics.
Affordability
As shown in Fig. 1, robots are by far the most expensive of the technologies reviewed here, ranging from several hundreds to upwards of thousands of US dollars, and typically require highly skilled technicians to operate and maintain them (Scassellati et al., 2012). Shared active surfaces and sensing technologies can also be very expensive, particularly when they require importing into LMIC. Costs associated with purchasing and installation of specialist equipment, software licencing, training and maintenance are likely to limit or even preclude the use of most technology platforms in LMIC community settings (Weiss et al., 2014). In most LMIC the internet connection speed and bandwidth required for technologies like telemedicine, IVC and VR are typically only available in large cities and can be up to four times more expensive than in HIC (ITU, 2016). It is also cheaper to access the internet using pre-paid mobile broadband data than fixed broadband services in these countries (ITU, 2016). Given the lower cost of android smartphones and greater access to cheaper mobile broadband services, an estimated 3.8 billion people worldwide were connecting to broadband internet services using their smartphones in 2019, 75% of whom from LMIC (Groupe Spéciale Mobile Association, 2020). For these reasons consensus ratings for affordability were ‘high’ for smartphone-based technologies and personal computers, ‘low’ for sensing and virtual reality technologies, and ‘very low’ for shared active surfaces and robotics.
Acceptability and Cultural Appropriateness
Telemedicine can transport specialist clinicians virtually to meet with families in their homes in low-resourced communities where in-person care is not available. However, telemedicine may not be acceptable to all. Some cultural groups do not allow any photography or video recordings of people at all (Boujarwah et al., 2011) or disapprove of the use of mobile phones by women in public (Wei & Kolko, 2005). In addition, it is not known how culturally acceptable virtual environments, the use of avatars, or participating in virtual reality-based activities would be in the culturally diverse communities in LMIC. Cultural beliefs often limit the adoption and use of technologies in LMIC (Bartneck et al., 2007; Rojas-Méndez et al., 2017). Many investigators of mHealth have highlighted the fact that access to mobile phones do not necessarily mean ownership of the device (Kumar et al., 2016). Sharing of or paying for mobile phone use is common practice and important in many African societies (Wesolowski et al., 2012). Ethical issues around confidentiality of health information and stigma therefore need careful consideration when determining if such services are appropriate and acceptable (Kaplan, 2006). However, given the increasing availability of cheaper mobile phones, the practice of sharing seems to be declining (Kumar et al., 2016; Wesolowski et al., 2015). Engaging the intended end-user community early should facilitate addressing local cultural, as well as practical challenges which may impede successful implementation (Grinker et al., 2012; Pickard et al., 2016). For these reasons, consensus ratings for acceptability/cultural appropriateness were ‘very high’ for smartphone-based technologies, ‘high’ for personal computers, sensing technologies and shared active surfaces, and ‘low’ for virtual reality and robotics.
Scalability
Technology can potentially address many of the challenges faced by people with ASD who live in LMIC. Successful use of such tools will depend on it being effective, acceptable, affordable and—importantly—have the capacity to reach individuals in under-served areas and to be applied on a large scale in a variety of settings (Kazdin & Rabbitt, 2013). A very overt aim of technology should therefore be to reach people wherever they are. Enabling community participation can further build capacity by increasing the number of people who can deliver services to those in need (Patel et al., 2008). Technology best suited to achieve this in LMIC would have to be familiar and widely used, not be dependent on uninterrupted electricity supply, and be able to receive and send information effectively and at low cost from almost anywhere. Advanced technologies such as VR and robotics typically require highly skilled people to operate and maintain them, as well as reliable and powerful internet and electricity infrastructure. Very high procurement and service costs are additional and important barriers to their widespread use. Even though PCs are increasingly accessible to many people in LMIC and telemedicine is gaining traction as a novel means of providing services to those in need who live in areas not well served by healthcare professionals, mobile phones today can perform most of the functions traditionally done on PCs. Accessing the internet via widely available mobile broadband services, using solar powered batteries to recharge the mobile phone’s power supply, sharing of phones or informal telecentres represent some of the ways in which mobile phones can overcome many of the unique challenges faced in LMIC. The evolution of mobile technology, the ever-expanding mobile broadband network as well as phones and data becoming more affordable, gives mobile health (mHealth) the greatest scalability potential to expand the reach of health, educational and other services to those in need. For these reasons, consensus ratings for scalability were ‘very high’ for smartphone-based technologies, ‘high’ for personal computers, ‘low’ for sensing technologies, shared active surfaces and virtual reality, and ‘very low’ for robotics.
Overall Feasibility
Taking together all implementation-related constructs, consensus ratings for overall feasibility in LMIC were ‘very high’ for smartphone-based technologies, ‘high’ for personal computers, ‘low’ for sensing technologies, shared active surfaces and virtual reality technologies, and ‘very low’ for robotics.
Discussion
Digital technologies have a very significant potential to improve the lives of people who live with ASD, and an increasing volume of ASD technology research has emerged in recent years. The COVID-19 pandemic accelerated the drive towards remote technologies for all aspects of life across the globe. However, mindful that most people with ASD live in low- or middle-income countries (LMIC), and given the pronounced digital divide between high-income countries (HIC) and LMIC, we set out to explore the feasibility of implementing these technologies in LMIC settings. We selected four implementation constructs—accessibility, affordability, appropriateness, scalability—for consensus evaluation towards an overall feasibility rating. Review of the technologies identified and highlighted a range of exciting developments in ASD research over the last 2 decades. Feasibility ratings, however, showed how technologies had very different strengths and weaknesses across different implementation constructs when the ‘implementation lens’ was focused on LMIC contexts. Of all technologies examined, mobile/cellular technologies showed the most consistent ‘high’ and ‘very high’ ratings across implementation constructs and had the highest overall feasibility ratings for implementation in LMIC. Taken together, mobile technologies therefore seem to have the greatest potential to ensure we do not inadvertently increase the pre-existing digital disparities between individuals with ASD and their families who live in HIC versus LMIC.
The narrative findings of the study underlined the fundamental importance of the context for technology. Earlier work by Kientz et al., (2014) and Odom et al., (2015) recognised the importance of ‘context’ as a variable. However, previous research used the term to refer to home, school, clinic, research as ‘context’. To date, no ASD technology research has used the term to refer to the macro-economic and/or cultural and linguistically diverse ‘contexts’ where people with ASD live. We propose to use the term ‘setting’ to refer to the specific place where a technology might be used (such as the school, home or clinic), and to use the term ‘context’ to refer to the broader socio/economic/cultural/linguistic environment into which a technology may be implemented. While robotics, shared active surfaces and virtual reality technologies may have significant potential application in various HIC contexts, the feasibility of implementation may look significantly different in LMIC contexts. It is laudable and important to examine how technology can be used to address the practical and day-to-day challenges of people who live with ASD. However, the global ASD community is culturally, linguistic, socio-economically and geographically immensely diverse. If our overarching goal is to address the disparities in access to ASD screening, diagnosis, and treatment between HIC and LMIC contexts using technology, these technologies need to be designed from the outset not only with the end-user, purpose, domain and setting in mind, but also with the accessibility, affordability, acceptability and scalability of the technology in the specific context and community of the end-user in mind. This highlights the need for all technological developments for ASD to include contextual implementation science evaluation (Proctor et al., 2011). Figure 4 represents our adaptation of the conceptual framework as presented by Odom et al., (2015) to incorporate the contextual implementation science lens (see Fig. 4). We propose that it is of fundamental importance to incorporate this broader view of ‘context’ to ensure that our technological solutions reduce, rather than inadvertently increase, the digital divide.
Fig. 4.
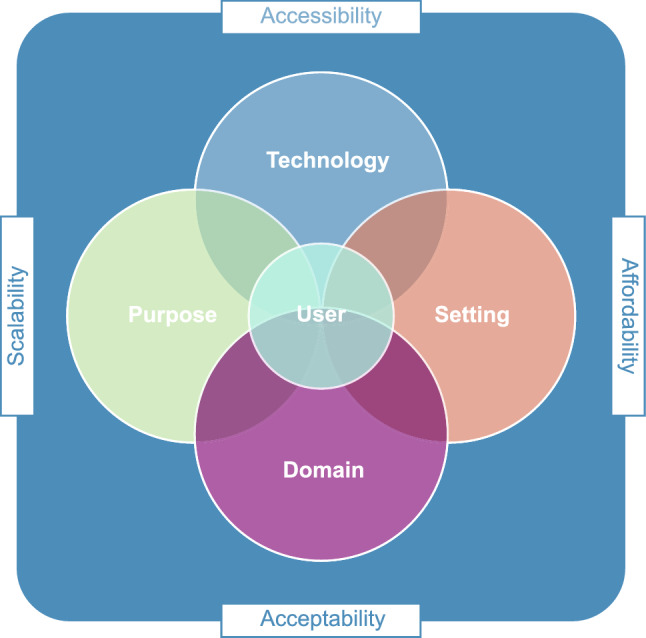
Key considerations in the development of technologies for low- and middle-income countries
Limitations of the Study
We acknowledge that this was a feasibility evaluation through expert consensus. The participants included only three expert reviewers based in the same global region. It is therefore possible that reviewers brought limited perspectives and their own biases that may have influenced overall feasibility ratings. However, reviewers represented three different professional groups, all had experience of working in multiple countries (across HIC and LMIC), all had expertise in technology and technology development for health applications, and weighted kappa values showed substantial agreement between raters and consensus. It would be very valuable for future studies to include stakeholders from diverse (but particularly LMIC) contexts. We further acknowledge that categorical ratings were performed without operationalised criteria. At present there are no global criteria for feasibility ratings of health technologies. For this reason, we included narrative comments to ‘motivate’ consensus ratings. Given the importance of the feasibility of technology, it may be helpful to develop a shared evaluation framework for technology in ASD, akin to the evaluation framework developed for parent education and training in ASD (Dawson-Squibb & de Vries, 2019). Notwithstanding these limitations, this was the first study to our knowledge to perform feasibility rating of ASD technologies. We hope that our approach may stimulate reflection about these constructs in research.
Conclusion
Evidence-based technologies for ASD can play a tremendous role to ensure that the majority of people living in under-served areas have timely access to appropriate services and support. Digital technologies may therefore have utility for identification, diagnostic procedures, intervention, training and research in HIC and LMIC settings. Here we reflected on the feasibility of six examples of such technologies in LMIC contexts. Our findings suggest that feasibility of the use of such technologies in LMIC will depend on the fundamental principles of affordability, accessibility, acceptability and cultural appropriateness. These will determine the likely scale-up (increasing the reach in the community of interest) and scale-out (expanding the reach to new or different communities) (Aarons et al., 2017), and will ensure that we do not inadvertently exacerbate the pre-exisiting digital disparities between HIC and LMIC contexts.
Given the widespread usage of mobile and smartphones and the increasing availability of affordable high-speed mobile internet access in the majority of LMIC, mHealth has the greatest potential to increase access to ASD screening, diagnosis and treatment globally. However, the evidence-base for mobile technologies in LMIC settings remains extremely limited. For instance, there are almost no Apps for ASD to date that have been evaluated specifically for a LMIC context. To address this knowledge gap careful and nuanced research will be required to establish the feasibility of using mobile applications to provide access to quality health, educational and other services and care to the culturally, linguistic, socio-economically and geographically diverse global ASD community.
Author Contributions
AJK and PJDV conceptualized and designed the study. AJK and MV collected and analyzed data. AJK and PJDV drafted and revised the manuscript. All authors read and approved the final manuscript.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aarons GA, Sklar M, Mustanski B, Benbow N, Brown CH. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implementation Science. 2017;12(1):111. doi: 10.1186/s13012-017-0640-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alozie NO, Akpan-Obong P. The digital gender divide: Confronting obstacles to women’s development in Africa. Development Policy Review. 2017;35(2):137–160. doi: 10.1111/dpr.12204. [DOI] [Google Scholar]
- Amaral DG, de Vries PJ. COVID-19 and autism research: Perspectives from around the globe. Autism Research. 2020;13(6):844–869. doi: 10.1002/aur.2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-5. American Psychiatric Association; 2013. [Google Scholar]
- Bakare MO, Agomoh AO, Ebigbo PO, Eaton J, Okonkwo KO, Onwukwe JU, Onyeama GM. Etiological explanation, treatability and preventability of childhood autism: A survey of Nigerian healthcare workers’ opinion. Annals of General Psychiatry. 2009;8(1):6. doi: 10.1186/1744-859X-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartneck C, Suzuki T, Kanda T, Nomura T. The influence of people’s culture and prior experiences with Aibo on their attitude towards robots. AI & SOCIETY. 2007;21(1):217–230. doi: 10.1007/s00146-006-0052-7. [DOI] [Google Scholar]
- Bauminger-Zviely N, Eden S, Zancanaro M, Weiss PL, Gal E. Increasing social engagement in children with high-functioning autism spectrum disorder using collaborative technologies in the school environment. Autism. 2013;17(3):317–339. doi: 10.1177/1362361312472989. [DOI] [PubMed] [Google Scholar]
- Ben-Sasson A, Lamash L, Gal E. To enforce or not to enforce? The use of collaborative interfaces to promote social skills in children with high functioning autism spectrum disorder. Autism. 2013;17(5):608–622. doi: 10.1177/1362361312451526. [DOI] [PubMed] [Google Scholar]
- Boccanfuso L, Scarborough S, Abramson RK, Hall AV, Wright HH, O’Kane JM. A low-cost socially assistive robot and robot-assisted intervention for children with autism spectrum disorder: Field trials and lessons learned. Autonomous Robots. 2017;41(3):637–655. doi: 10.1007/s10514-016-9554-4. [DOI] [Google Scholar]
- Boujarwah, F. A., Hong, H., Abowd, G. D., Arriaga, R. I. (2011). Towards a framework to situate assistive technology design in the context of culture. Paper presented at the proceedings of the 13th international ACM SIGACCESS conference on Computers and accessibility. Doi: 10.1145/2049536.2049542
- Bradshaw J, Steiner AM, Gengoux G, Koegel LK. Feasibility and effectiveness of very early intervention for infants at-risk for autism spectrum disorder: A systematic review. Journal of Autism and Developmental Disorders. 2015;45(3):778–794. doi: 10.1007/s10803-014-2235-2. [DOI] [PubMed] [Google Scholar]
- Cabibihan JJ, Javed H, Aldosari M, Frazier TW, Elbashir H. Sensing technologies for autism spectrum disorder screening and intervention. Sensors (Basel, Switzerland) 2017;17(1):46. doi: 10.3390/s17010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby KM. The rationale for computer-based treatment of language difficulties in nonspeaking autistic children. Journal of Autism and Childhood Schizophrenia. 1973;3(3):254–260. doi: 10.1007/BF01538283. [DOI] [PubMed] [Google Scholar]
- Colby KM, Smith DC. Computers in the treatment of nonspeaking autistic children. Current Psychiatric Therapies. 1971;11:1–17. [PubMed] [Google Scholar]
- Constantino JN, Kennon-McGill S, Weichselbaum C, Marrus N, Haider A, Glowinski AL, Gillespie S, Klaiman C, Klin A, Jones W. Infant viewing of social scenes is under genetic control and is atypical in autism. Nature. 2017;547(7663):340–344. doi: 10.1038/nature22999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daley TC. From symptom recognition to diagnosis: Children with autism in urban India. Social Science and Medicine. 2004;58(7):1323–1335. doi: 10.1016/S0277-9536(03)00330-7. [DOI] [PubMed] [Google Scholar]
- Dautenhahn K, Werry I. Towards interactive robots in autism therapy: Background, motivation and challenges. Pragmatics & Cognition. 2004;12(1):1–35. doi: 10.1075/pc.12.1.03dau. [DOI] [Google Scholar]
- David DO, Costescu CA, Matu S, Szentagotai A, Dobrean A. Effects of a robot-enhanced intervention for children with ASD on teaching turn-taking skills. Journal of Educational Computing Research. 2020;58(1):29–62. doi: 10.1177/0735633119830344. [DOI] [Google Scholar]
- Dawson G, Jones EJ, Merkle K, Venema K, Lowy R, Faja S, Kamara D, Murias M, Greenson J, Winter J, Smith M, Rogers SJ, Webb SJ. Early behavioral intervention is associated with normalized brain activity in young children with autism. Journal of the America Academy of Child & Adolescent Psychiatry. 2012;51(11):1150–1159. doi: 10.1016/j.jaac.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson-Squibb JJ, de Vries PJ. Developing an evaluation framework for parent education and training in autism spectrum disorder: Results of a multi-stakeholder process. Journal of Autism and Developmental Disorders. 2019;49(11):4468–4481. doi: 10.1007/s10803-019-04176-w. [DOI] [PubMed] [Google Scholar]
- de Vries PJ. Thinking globally to meet local needs: Autism spectrum disorders in Africa and other low-resource environments. Current Opinion in Neurology. 2016;29(2):130–136. doi: 10.1097/WCO.0000000000000297. [DOI] [PubMed] [Google Scholar]
- Dickstein-Fischer L, Alexander E, Yan X, Su H, Harrington K, Fischer GS. An affordable compact humanoid robot for Autism Spectrum Disorder interventions in children. IEEE Engineering in Medicine and Biology Society. Annual Conference. 2011;2011:5319–5322. doi: 10.1109/IEMBS.2011.6091316. [DOI] [PubMed] [Google Scholar]
- Dickstein-Fischer LA, Crone-Todd DE, Chapman IM, Fathima AT, Fischer GS. Socially assistive robots: current status and future prospects for autism interventions. Innovation and Entrepreneurship in Health. 2018;5:15–25. doi: 10.2147/IEH.S138753. [DOI] [Google Scholar]
- Dickstein-Fischer, L. A., Pereira, R. H., Gandomi, K. Y., Fathima, A. T., & Fischer, G. S. (2017). Interactive tracking for robot-assisted autism therapy. Paper presented at the Proceedings of the Companion of the 2017 ACM/IEEE International Conference on Human-Robot Interaction, Vienna, Austria. 10.1145/3029798.3038390
- Diehl JJ, Schmitt LM, Villano M, Crowell CR. The clinical use of robots for individuals with autism spectrum disorders: A critical review. Research in Autism Spectrum Disorders. 2012;6(1):249–262. doi: 10.1016/j.rasd.2011.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz, P., & Leigh, D. (2001). DiamondTouch: a multi-user touch technology. Paper presented at the Proceedings of the 14th annual ACM symposium on User interface software and technology. 10.1145/502348.502389
- Divan G, Vajaratkar V, Desai MU, Strik-Lievers L, Patel V. Challenges, coping strategies, and unmet needs of families with a child with autism spectrum disorder in Goa, India. Autism Research. 2012;5(3):190–200. doi: 10.1002/aur.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkin MS, Elsabbagh M, Barbaro J, Gladstone M, Happe F, Hoekstra RA, Shih A. Autism screening and diagnosis in low resource settings: Challenges and opportunities to enhance research and services worldwide. Autism Research. 2015;8(5):473–476. doi: 10.1002/aur.1575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta, S., Geiger, T., & Lanvin, B. (2015). The Global Information Technology Report. ICTs for Inclusive Growth. Paper presented at the Geneva, World Economic Forum and INSEAD. Retrieved from http://www3.weforum.org/docs/WEF_Global_IT_Report_2015.pdf. (Accessed 21 Nov 2020)
- Egger HL, Dawson G, Hashemi J, Carpenter KL, Espinosa S, Campbell K, Tepper M. Automatic emotion and attention analysis of young children at home: A ResearchKit autism feasibility study. NPJ Digital Medicine. 2018;1(1):1–10. doi: 10.1038/s41746-018-0024-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsabbagh M, Divan G, Koh YJ, Kim YS, Kauchali S, Marcín C, Montiel-Nava C, Pate V, Paula CS, Wang C, Yasamy MT, Fombonne E. Global prevalence of autism and other pervasive developmental disorders. Autism Research. 2012;5(3):160–179. doi: 10.1002/aur.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facebook Technologies. (2021). Compare headsets. Retrieved from https://www.oculus.com/compare/. (Accessed 12 Jan 2021)
- Farley MA, McMahon WM, JensonFombonne WRE, Miller J, Gardner M, Block H, Pingree CB, Ritvo ER, Ritvo RA, Coon H. Twenty-year outcome for individuals with autism and average or near-average cognitive abilities. Autism Research. 2009;2(2):109–118. doi: 10.1002/aur.69. [DOI] [PubMed] [Google Scholar]
- Fletcher RR, Dobson K, Goodwin MS, Eydgahi H, Wilder-Smith O, Fernholz D, Picard RW. iCalm: Wearable sensor and network architecture for wirelessly communicating and logging autonomic activity. IEEE Transactions on Information Technology in Biomedicine. 2010;14(2):215–223. doi: 10.1109/titb.2009.2038692. [DOI] [PubMed] [Google Scholar]
- Florida State University. (2021). Baby Navigator. Retrieved from https://babynavigator.com. (Accessed 6 Jan 2021)
- Fombonne E. Epidemiology of pervasive developmental disorders. Pediatric Research. 2009;65(6):591–598. doi: 10.1203/PDR.0b013e31819e7203. [DOI] [PubMed] [Google Scholar]
- Franz L, Chambers N, von Isenburg M, de Vries PJ. Autism spectrum disorder in sub-saharan africa: A comprehensive scoping review. Autism Research. 2017;10(5):723–749. doi: 10.1002/aur.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gal E, Lamash L, Bauminger-Zviely N, Zancanaro M, Weiss PL. Using multitouch collaboration technology to enhance social interaction of children with high-functioning autism. Physical & Occupational Therapy in Pediatrics. 2016;36(1):46–58. doi: 10.3109/01942638.2015.1040572. [DOI] [PubMed] [Google Scholar]
- Gartner. (2018). Gartner Says Worldwide Wearable Device Sales to Grow 26 Percent in 2019. https://www.gartner.com/en/newsroom/press-releases/2018-11-29-gartner-says-worldwide-wearable-device-sales-to-grow. (Accessed 22 Nov 2020)
- Gentry T, Wallace J, Kvarfordt C, Lynch KB. Personal digital assistants as cognitive aids for high school students with autism: Results of a community-based trial. Journal of Vocational Rehabilitation. 2010;32(2):101–107. doi: 10.3233/JVR-2010-0499. [DOI] [Google Scholar]
- Gillwald, A. (2013). Towards an understanding of ICT access and use in Africa. Retrieved from https://www.researchictafrica.net/presentations/Presentations/2013%20Gillwald%20-%20Towards%20an%20understanding%20of%20%20ICT%20access%20and%20use%20in%20Africa.pdf. (Accessed 22 Nov 2020)
- Gomez R. When you do not have a computer: Public-access computing in developing countries. Information Technology for Development. 2014;20(3):274–291. doi: 10.1080/02681102.2012.751573. [DOI] [Google Scholar]
- Goodwin MS, Groden J, Velicer WF, Lipsitt LP, Baron MG, Hofmann SG, Groden G. Cardiovascular arousal in individuals with autism. Focus on Autism and Other Developmental Disabilities. 2006;21(2):100–123. doi: 10.1177/10883576060210020101. [DOI] [Google Scholar]
- Goodwin MS, Intille SS, Albinali F, Velicer WF. Automated detection of stereotypical motor movements. Journal of Autism and Developmental Disorders. 2011;41(6):770–782. doi: 10.1007/s10803-010-1102-z. [DOI] [PubMed] [Google Scholar]
- Grinker RR, Chambers N, Njongwe N, Lagman AE, Guthrie W, Stronach S, Richard BO, Kauchali S, Killian B, Chhagan M, Yucel F, Kumudu M, Baker-Cummings C, Grether J, Wetherby AM. “Communities” in community engagement: lessons learned from autism research in South Korea and South Africa. Autism Research. 2012;5(3):201–210. doi: 10.1002/aur.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groupe Spéciale Mobile Association. (2020). The state of mobile internet connectivitiy 2020. Retrieved from https://www.gsma.com/r/wp-content/uploads/2020/09/GSMA-State-of-Mobile-Internet-Connectivity-Report-2020.pdf. (Accessed 23 Nov 2020)
- Grynszpan O, Weiss PL, Perez-Diaz F, Gal E. Innovative technology-based interventions for autism spectrum disorders: A meta-analysis. Autism. 2014;18(4):346–361. doi: 10.1177/1362361313476767. [DOI] [PubMed] [Google Scholar]
- Harrison AJ, Bradshaw LP, Naqvi NC, Paff ML, Campbell JM. Development and psychometric evaluation of the autism stigma and knowledge questionnaire (ASK-Q) Journal of Autism and Developmental Disorders. 2017;47(10):3281–3295. doi: 10.1007/s10803-017-3242-x. [DOI] [PubMed] [Google Scholar]
- Harrison AJ, Long KA, Tommet DC, Jones RN. Examining the role of race, ethnicity, and gender on social and behavioral ratings within the autism diagnostic observation schedule. Journal of Autism and Developmental Disorders. 2017;47(2):2770–2782. doi: 10.1007/s10803-017-3176-3. [DOI] [PubMed] [Google Scholar]
- Hedges SH, Odom SL, Hume K, Sam A. Technology use as a support tool by secondary students with autism. Autism. 2018;22(1):70–79. doi: 10.1177/1362361317717976. [DOI] [PubMed] [Google Scholar]
- International Data Corporation (IDC). (2019). Worldwide Wearables Market to Top 300 Million Units in 2019 and Nearly 500 Million Units in 2023, Says IDC. Retrieved from https://www.idc.com/getdoc.jsp?containerId=prUS45737919. (Accessed 23 Nov 2020)
- International Data Corporation (IDC). (2020). Low- to Mid-Range Smartphones Dominate Worldwide Smartphone Forecast with the Fastest Growth Expected in $400–600 Price Band, According to IDC. Retrieved from https://www.idc.com/getdoc.jsp?containerId=prUS46865120. (Accessed 23 Nov 2020)
- International Telecommunication Union (ITU). (2010). ICT Facts and Figures 2010. Retrieved from https://www.itu.int/ITU-D/ict/material/FactsFigures2010.pdf. (Accessed 23 Nov 2020)
- International Telecommunication Union (ITU). (2016). ICT Facts and Figures 2016. Retrieved from https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2016.pdf. (Accessed 23 Nov 2020)
- International Telecommunication Union (ITU). (2019). Statistics. Global and Regional ICT Data (2005–2019). Retrieved fromhttps://www.itu.int/en/ITU-D/Statistics/Pages/stat/default.aspx. (Accessed 23 Nov 2020)
- Kandalaft MR, Didehbani N, Krawczyk DC, Allen TT, Chapman SB. Virtual reality social cognition training for young adults with high-functioning autism. Journal of Autism and Developmental Disorders. 2013;43(1):34–44. doi: 10.1007/s10803-012-1544-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanne SM, Carpenter LA, Warren Z. Screening in toddlers and preschoolers at risk for autism spectrum disorder: Evaluating a novel mobile-health screening tool. Autism Research. 2018;11(7):1038–1049. doi: 10.1002/aur.1959. [DOI] [PubMed] [Google Scholar]
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Globalization and Health. 2006;2(1):9. doi: 10.1186/1744-8603-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karsh BT. Beyond usability: Designing effective technology implementation systems to promote patient safety. Quality and Safety in Health Care. 2004;13:388–394. doi: 10.1136/qhc.13.5.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science. 2013;1(2):170–191. doi: 10.1177/2167702612463566. [DOI] [Google Scholar]
- Keusch GT, Wilentz J, Kleinman A. Stigma and global health: developing a research agenda. Lancet. 2006;367(9509):525–527. doi: 10.1016/S0140-6736(06)68183-X. [DOI] [PubMed] [Google Scholar]
- Kientz JA, Goodwin MS, Hayes GR, Abowd GD. Interactive technologies for autism. Synthesis Lectures on Assistive, Rehabilitative, and Health-Preserving Technologies. 2014;2(2):1–177. doi: 10.2200/S00533ED1V01Y201309ARH004. [DOI] [Google Scholar]
- Kim ES, Berkovits LD, Bernier EP, Leyzberg D, Shic F, Paul R, Scassellati B. Social robots as embedded reinforcers of social behavior in children with autism. Journal of Autism and Developmental Disorders. 2012;43(5):1038–1049. doi: 10.1007/s10803-012-1645-2. [DOI] [PubMed] [Google Scholar]
- Koumpouros Y, Kafazis T. Wearables and mobile technologies in autism spectrum disorder interventions: A systematic literature review. Research in Autism Spectrum Disorders. 2019;66:1–25. doi: 10.1016/j.rasd.2019.05.005. [DOI] [Google Scholar]
- Kumar P, Paton C, Kirigia D. I’ve got 99 problems but a phone ain’t one: Electronic and mobile health in low and middle income countries. Archives of Diseases in Childhood. 2016;101(10):974–979. doi: 10.1136/archdischild-2015-308556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumazaki H, Yoshikawa Y, Yoshimura Y, Ikeda T, Hasegawa C, Saito DN, Ishiguro H. The impact of robotic intervention on joint attention in children with autism spectrum disorders. Molecular Autism. 2018;9(1):1–10. doi: 10.1186/s13229-018-0230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagunju IA, Bella-Awusah TT, Omigbodun OO. Autistic disorder in Nigeria: Profile and challenges to management. Epilepsy & Behavior. 2014;39:126–129. doi: 10.1016/j.yebeh.2014.08.020. [DOI] [PubMed] [Google Scholar]
- Law GC, Neihart M, Dutt A. The use of behavior modeling training in a mobile app parent training program to improve functional communication of young children with autism spectrum disorder. Autism. 2018;22(4):424–439. doi: 10.1177/1362361316683887. [DOI] [PubMed] [Google Scholar]
- Mahapatra P, Pati S, Sinha R, Chauhan AS, Nanda RR, Nallala S. Parental care-seeking pathway and challenges for autistic spectrum disorders children: A mixed method study from Bhubaneswar, Odisha. Indian Journal of Psychiatry. 2019;61(1):37–44. doi: 10.4103/psychiatry.IndianJPsychiatry_257_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michels KM, Hofman KJ, Keusch GT, Hrynkow SH. Stigma and global health: Looking forward. Lancet. 2006;367(9509):538–539. doi: 10.1016/S0140-6736(06)68190-7. [DOI] [PubMed] [Google Scholar]
- Min, C. H., & Tewfik, A. H. (2010). Automatic characterization and detection of behavioral patterns using linear predictive coding of accelerometer sensor data. Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Annual Conference, 2010: 220–223. 10.1109/IEMBS.2010.5627850 [DOI] [PubMed]
- Naslund JA, Aschbrenner KA, Araya R, Marsch LA, Unutzer J, Patel V, Bartels SJ. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: A narrative review of the literature. Lancet Psychiatry. 2017;4(6):486–500. doi: 10.1016/S2215-0366(17)30096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odom SL, Thompson JL, Hedges S, Boyd BA, Dykstra JR, Duda MA, Bord A. Technology-aided interventions and instruction for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(12):3805–3819. doi: 10.1007/s10803-014-2320-6. [DOI] [PubMed] [Google Scholar]
- Olusanya BO, Davis AC, Wertlieb D, Boo NY, Nair M, Halpern R, Kuper H, Breinbauer C, de Vries PJ, Gladstone M, Halfon N, Kancherla V, Mulaudzi MC, Kakooza-Mwesige A, Ogbo FA, Olusanya JO, WrightWilliams SMAN, Manguerra H, Kassebaum NJ. Developmental disabilities among children younger than 5 years in 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet Global Health. 2018;6(10):e1100–e1121. doi: 10.1016/S2214-109X(18)30309-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olusanya BO, Wright SM, Nair MKC, Boo N-Y, Halpern R, Kuper H, Kassebaum NJ. Global burden of childhood epilepsy, intellectual disability, and sensory impairments. Pediatrics. 2020 doi: 10.1542/peds.2019-2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons D, Wilson NJ, Vaz S, Lee H, Cordier R. Appropriateness of the TOBY application, an iPad intervention for children with autism spectrum disorder: A thematic approach. Journal of Autism and Developmental Disorders. 2019;49(10):4053–4066. doi: 10.1007/s10803-019-04115-9. [DOI] [PubMed] [Google Scholar]
- Parsons S, Leonard A, Mitchell P. Virtual environments for social skills training: Comments from two adolescents with autistic spectrum disorder. Computers & Education. 2006;47(2):186–206. doi: 10.1016/j.compedu.2004.10.003. [DOI] [Google Scholar]
- Parsons S, Mitchell P, Leonard A. The use and understanding of virtual environments by adolescents with autistic spectrum disorders. Journal of Autism and Developmental Disorders. 2004;34(4):449–466. doi: 10.1023/b:jadd.0000037421.98517.8d. [DOI] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. Journal of Child Psychology and Psychiatry. 2008;49(3):313–334. doi: 10.1111/j.1469-7610.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- Paul R, Augustyn A, Klin A, Volkmar FR. Perception and production of prosody by speakers with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2005;35(2):205–220. doi: 10.1007/s10803-004-1999-1. [DOI] [PubMed] [Google Scholar]
- Pickard KE, Wainer AL, Bailey KM, Ingersoll BR. A mixed-method evaluation of the feasibility and acceptability of a telehealth-based parent-mediated intervention for children with autism spectrum disorder. Autism. 2016;20(7):845–855. doi: 10.1177/1362361315614496. [DOI] [PubMed] [Google Scholar]
- Pillay S, Duncan EM, de Vries PJ. Autism in the Western Cape province of South Africa: Rates, socio-demographics, disability and educational characteristics in one million school children. Autism. 2021;25(4):1076–1089. doi: 10.1177/1362361320978042. [DOI] [PubMed] [Google Scholar]
- Ploog BO, Scharf A, Nelson D, Brooks PJ. Use of computer-assisted technologies (CAT) to enhance social, communicative, and language development in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013;43(2):301–322. doi: 10.1007/s10803-012-1571-3. [DOI] [PubMed] [Google Scholar]
- POP Communications. (2020). How much should an interactive touchscreen solution cost?. https://www.popcomms.com/blog/much-interactive-touchscreen-solution-cost/ (Accessed 23 Nov 2020)
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Hensley M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers SJ, Dawson G. Early start Denver model for young children with autism: Promoting language, learning, and engagement. Guilford Press; 2010. [Google Scholar]
- Rogerson J, Falkmer M, Cuomo B, Falkmer T, Whitehouse AJO, Granich J, Vaz S. Parental experiences using the therapy outcomes by you (TOBY) application to deliver early intervention to their child with autism. Developmental Neurorehabilitation. 2019;22(4):219–227. doi: 10.1080/17518423.2018.1440259. [DOI] [PubMed] [Google Scholar]
- Rojas-Méndez JI, Parasuraman A, Papadopoulos N. Demographics, attdes, and technology readiness. Marketing Intelligence & Planning. 2017;35(1):18–39. doi: 10.1108/mip-08-2015-0163. [DOI] [Google Scholar]
- Ruparelia K, Abubakar A, Badoe E, Bakare M, Visser K, Chugani DC, Chugani HT, Donald KA, Wilmshurst JM, Shih A, Skuse D, Newton CR. Autism spectrum disorders in Africa: Current challenges in identification, assessment, and treatment a report on the international child neurology association meeting on ASD in Africa, Ghana, April 3–5. Journal of Child Neurology. 2014;31(8):1018–1026. doi: 10.1177/0883073816635748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saiano M, Pellegrino L, Casadio M, Summa S, Garbarino E, Rossi V, Sanguineti V. Natural interfaces and virtual environments for the acquisition of street crossing and path following skills in adults with autism spectrum disorders: A feasibility study. Journal of Neuroengineering and Rehabilitation. 2015;12(1):17. doi: 10.1186/s12984-015-0010-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarker H, Tam A, Foreman M, Fay N, Dhuliawala M, Das A. Detection of stereotypical motor movements in autism using a smartwatch-based system. Annual Symposium Proceedings. AMIA Symposium. 2018;2018:952–960. [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370(9590):878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- Scassellati B. How social robots will help us to diagnose, treat, and understand autism. In: Thrun S, Brooks R, Durrant-Whyte H, editors. Robotics research. Springer tracts in advanced robotic. Berlin: Springer; 2007. pp. 552–563. [Google Scholar]
- Scassellati B, Admoni H, Matarić M. Robots for use in autism research. Annual Review of Biomedical Engineering. 2012;14:275–294. doi: 10.1146/annurev-bioeng-071811-150036. [DOI] [PubMed] [Google Scholar]
- Silver, L. (2019). Smartphone ownership is growing rapidly around the world, but not always equally. Pew Research Center. https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/. (Accessed 30 Apr 2020)
- Standen PJ, Brown DJ. Virtual reality in the rehabilitation of people with intellectual disabilities: Review. Cyberpsychology, Behavavior, and Social Networking. 2005;8(3):272–288. doi: 10.1089/cpb.2005.8.272. [DOI] [PubMed] [Google Scholar]
- Statista. (2020a). Average selling price of personal computers (PCs) worldwide from 2015 to 2019, in actual and constant currency. Retrieved from https://www.statista.com/statistics/722992/worldwide-personal-computers-average-selling-price/. (Accessed 22 Nov 2020)
- Statista. (2020b). Smartphone ownership rate by country 2018. https://www.statista.com/statistics/539395/smartphone-penetration-worldwide-by-country/. (Accessed 22 Nov 2020)
- Statista. (2021). Number of mHealth apps available in the Apple App Store from 1st quarter 2015 to 4th quarter 2020. Retrieved from https://www.statista.com/statistics/779910/health-apps-available-ios-worldwide/https://www.statista.com/statistics/779919/health-apps-available-google-play-worldwide/. (Accessed 22 Nov 2020)
- Stichter JP, Laffey J, Galyen K, Herzog M. iSocial: Delivering the social competence intervention for adolescents (SCI-A) in a 3D virtual learning environment for youth with high functioning autism. Journal of Autism and Developmental Disorders. 2014;44(2):417–430. doi: 10.1007/s10803-013-1881-0. [DOI] [PubMed] [Google Scholar]
- Travers JC, Fefer SA. Effects of shared active surface technology on the communication and speech of two preschool children with disabilities. Focus on Autism and Other Developmental Disabilities. 2016;32(1):44–54. doi: 10.1177/1088357615611390. [DOI] [Google Scholar]
- van Schalkwyk GI, Marin CE, Ortiz M, Rolison M, Qayyum Z, McPartland JC, Silverman WK. Social media use, friendship quality, and the moderating role of anxiety in adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2017;47(9):2805–2813. doi: 10.1007/s10803-017-3201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal M, Turner J, Bulling A, Gellersen H. Wearable eye tracking for mental health monitoring. Computer Communications. 2012;35(11):1306–1311. doi: 10.1016/j.comcom.2011.11.002. [DOI] [Google Scholar]
- Vismara LA, Young GS, Stahmer AC, Griffith EM, Rogers SJ. Dissemination of evidence-based practice: Can we train therapists from a distance? Journal of Autism and Developmental Disorders. 2009;39(12):1636–1651. doi: 10.1007/s10803-009-0796-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren SF, Gilkerson J, Richards JA, Oller DK, Xu D, Yapanel U, Gray S. What automated vocal analysis reveals about the vocal production and language learning environment of young children with autism. Journal of Autism and Developmental Disorders. 2010;40(5):555–569. doi: 10.1007/s10803-009-0902-5. [DOI] [PubMed] [Google Scholar]
- Wei C, Kolko BE. Studying mobile phone use in context: Cultural, political, and economic dimensions of mobile phone use. Paper Presented at the Professional Communication Conference. 2005 doi: 10.1109/IPCC.2005.1494179. [DOI] [Google Scholar]
- Weiss, P., Cobb, S., & Zancanaro, M. (2014). Challenges in developing new technologies for special needs education: A force-field analysis. Paper presented at the 10th International Conference on Disability, Virtual Reality and Associated Technologies, Sweden. Retrieved from https://pdfs.semanticscholar.org/46f3/083aa3ebfd6842503c443956c2488f49426a.pdf. (Accessed 30 Apr 2020)
- Wesolowski A, Eagle N, Noor AM, Snow RW, Buckee CO. Heterogeneous mobile phone ownership and usage patterns in Kenya. PLoS ONE. 2012 doi: 10.1371/journal.pone.0035319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesolowski A, O'Meara WP, Tatem AJ, Ndege S, Eagle N, Buckee CO. Quantifying the impact of accessibility on preventive healthcare in sub-Saharan Africa using mobile phone data. Epidemiology. 2015;26(2):223–228. doi: 10.1097/EDE.0000000000000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherby, A. M., Woods, J. J., Morgan, L., Holland, R. D., & Wiseman, N. D. R. (n.d.). Autism Navigator. Retrieved from http://www.autismnavigator.com. (Accessed 29 Apr 2020)
- Williams LW, Matson JL, Beighley JS, Konst M. Ethnic disparities in early autism assessment: A large scale screening study of infants and toddlers. Journal of Developmental and Physical Disabilities. 2014;27(2):141–148. doi: 10.1007/s10882-014-9406-0. [DOI] [Google Scholar]
- World Bank. (2016). World Development Report 2016—Digital Dividends. Retrieved from http://documents.worldbank.org/curated/en/896971468194972881/pdf/102725-PUB-Replacement-PUBLIC.pdf. (Accessed 22 Nov 2020)
- World Bank. (2020). Development Data Group. Income level/low- and middle-income countries. Retrieved from https://data.worldbank.org/income-level/low-and-middle-income. (Accessed 22 Nov 2020)
- World Health Organization. (2013). Meeting report: Autism spectrum disorders and other developmental disorders: From raising awareness to building capacity: World Health Organization, Geneva, Switzerland. Retrieved from https://apps.who.int/iris/handle/10665/103312. (Accessed 22 Nov 2020)
- Ye Q, Deng Z, Chen Y, Liao J, Li G, Lu Y. How resource scarcity and accessibility affect patients’ usage of mobile health in China: Resource competition perspective. JMIR mHealth and uHealth. 2019 doi: 10.2196/13491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye, Z., Li, Y., Fathi, A., Han, Y., Rozga, A., Abowd, G. D., & Rehg, J. M. (2012). Detecting eye contact using wearable eye-tracking glasses. In Proceedings of the 2012 ACM Conference on Ubiquitous Computing (UbiComp ’12). Association for Computing Machinery, New York, NY, USA, 699–704. 10.1145/2370216.2370368
- Zurovac D, Sudoi RK, Akhwale WS, Ndiritu M, Hamer DH, Rowe AK, Snow RW. The effect of mobile phone text-message reminders on Kenyan health workers’ adherence to malaria treatment guidelines: A cluster randomised trial. Lancet. 2011;378(9793):795–803. doi: 10.1016/S0140-6736(11)60783-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurovac D, Talisuna AO, Snow RW. Mobile phone text messaging: tool for malaria control in Africa. PLoS Medicine. 2012 doi: 10.1371/journal.pmed.1001176. [DOI] [PMC free article] [PubMed] [Google Scholar]