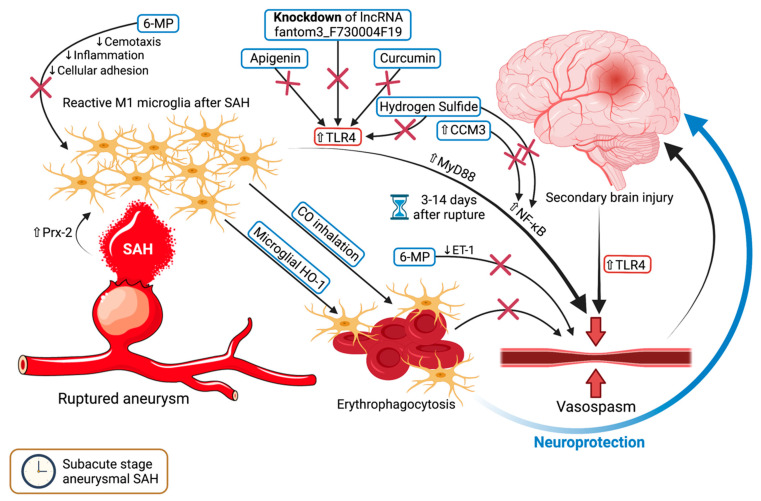
Figure 2.
The mechanisms and pathways involving microglia in the subacute stage of subarachnoid hemorrhage (SAH), primarily vasospasm. The reactive M1 microglia that had been stimulated by SAH via Prx-2, in conjunction with the upregulation of TLR4, will result in an anarchic constriction of the cerebral vasculature, aggravating the preexisting brain injury. This occurs between days 3 and 14 after aneurysmal rupture. Certain agents have been shown to suppress the TLR4-dependent pathways by targeting TLR4, namely apigenin, curcumin, hydrogen sulfide, and the knockdown of the long non-coding RNA fantom3_F730004F19. Hydrogen sulfide and CCM3 upregulation also affect a downstream component of the pathophysiological cascade, namely NF-κB. 6-mercaptopurine restricts vasospasm via endothelin-1 inhibition, while additionally reducing microglial-mediated, inflammation, chemotaxis, and cellular adhesion. CO inhalation and microglial HO-1 stimulate erythrophagocytosis, which in turn alleviates vasospasm and reduces brain damage. A transparent upward-pointing arrow denotes upregulation, whereas a thin downward pointing arrow signifies an inhibition of the mentioned process or protein. Red crosses mark an inhibitory effect. Abbreviations (in alphabetical order): 6-MP, 6-mercaptopurine; CO, carbon monoxide; CCM3, cerebral cavernous malformation 3 gene; ET-1, endothelin 1; HO-1, heme oxygenase isoform 1; lncRNA, long non-coding RNA; MyD88, myeloid differentiation primary response gene 88; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; Prx-2, peroxiredoxin 2; SAH, subarachnoid hemorrhage; TLR4, toll-like receptor 4.