Abstract
Intimate partner violence (IPV) is a serious mental and physical health concern worldwide. Although previous research suggests that childhood maltreatment increases the risk for IPV, the underlying psychological mechanisms of this relationship are not yet entirely understood. Borderline personality (BP) features may play an important role in the cycle of violence, being associated with interpersonal violence in both childhood and adult relationships. The present study investigated whether BP features mediate the relationship between childhood maltreatment and IPV, differentiating between perpetration and victimization, and taking maladaptive stress coping and gender into account. Self-reports on IPV, childhood trauma, BP features, and maladaptive stress coping were collected in a mixed (nonclinical and clinical) sample of 703 adults (n = 537 female, n = 166 male), using an online survey. A serial mediation analysis (PROCESS) was performed to quantify the direct effect of childhood maltreatment on IPV and its indirect effects through BP features and maladaptive coping. Childhood maltreatment severity significantly positively predicted IPV perpetration as well as victimization. BP features, but not coping, partially mediated this relationship. Follow-up analyses suggest that affective instability and interpersonal disturbances (e.g., separation concerns) play an important role in IPV perpetration, while interpersonal and identity disturbances may mediate the effect of childhood maltreatment on IPV victimization. In clinical practice, attention should be paid not only to histories of childhood abuse and neglect but also to BP features, which may be possible risk factors for IPV.
Keywords: child abuse, neglect, predicting domestic violence, domestic violence, intergenerational transmission of trauma, revictimization, sexual assault
Introduction
Intimate partner violence (IPV), defined as violent or coercive acts perpetrated by one intimate partner against the other, either in an existing or past relationship, is a serious physical and mental health concern worldwide (Afifi et al., 2009). According to recent surveys, approximately 15% to 35% of women and 20% to 25% of men in the United States have experienced one or multiple forms of psychological, physical, and sexual IPV at some point in their life, either as a perpetrator or as a victim (Afifi et al., 2009; Cameranesi, 2016; Capaldi et al., 2009; Whitaker, Haileyesus, Swahn, & Saltzman, 2007). In most cases, IPV is reciprocal, that is, both partners engage in violent behavior when conflicts escalate (Whitaker et al., 2007). Although there is some evidence that IPV, especially physical aggression in men toward their partners, decreases over time (Kim, Laurent, Capaldi, & Feingold, 2008), this seems to depend on psychological risk factors, such as psychiatric symptoms (Johnson, Giordano, Manning, & Longmore, 2015), and consequences of IPV can be lifelong and even lethal (Capaldi, Knoble, Shortt, & Kim, 2012; Peterman, Bleck, & Palermo, 2015). IPV is the leading cause of homicide death in the United States and a risk factor for suicidal attempts. Other serious physical and mental health outcomes include an increased risk for depression, anxiety disorders, posttraumatic stress disorder (PTSD), substance abuse, and personality disorders (Afifi et al., 2009; Capaldi et al., 2012; Devries et al., 2013; Willie et al., 2019). These mental conditions are not only frequent consequences of IPV but also increase the risk for IPV (Devries et al., 2013; Dutton, Tetreault, Karakanta, & White, 2015; Maneta, Cohen, Schulz, & Waldinger, 2013; Stith, Smith, Penn, Ward, & Tritt, 2004), establishing a vicious cycle. Given the high prevalence, complexity, and burden of IPV, identifying risk and contributing factors remains of utmost importance (Riggs, Caulfield, & Street, 2000).
Evidence suggests that childhood maltreatment, such as abuse and neglect, increases the risk for perpetrating and/or re-experiencing interpersonal violence in adult relationships (Gilbert et al., 2009; Linder & Collins, 2005; McMahon et al., 2015; Swinford, DeMaris, Cernkovich, & Giordano, 2000; Whitfield, Anda, Dube, & Felitti, 2003; Widom, Czaja, & Dutton, 2014). However, meta-analyses of studies on the intergenerational transmission of abuse found only low to moderate effect sizes (Capaldi et al., 2012; Stith et al., 2000, 2004). This suggests that the link between growing up in an abusive family and IPV is more complex and cannot be fully explained by reenactment (e.g., individuals, who experienced violence in childhood, may have learned to believe that it is an acceptable strategy for coping with conflicts; Bandura, 1973; Cappell & Heiner, 1990; Franklin & Kercher, 2012; Walker, 1977).
Identifying factors that may increase the vulnerability to re-experience or transmit abuse over generations can help to detect targets for prevention and treatment. The presence of borderline personality disorder (BPD) features and maladaptive coping may be important psychological factors in this relationship (Clift & Dutton, 2011; Dutton, 2002; Mauricio, 2007).
BPD core features, namely, affective instability, disturbed sense of self, instable identity, interpersonal disturbances, and self-harming impulsivity (American Psychiatric Association [APA], 2013), are thought to develop under the influence of childhood maltreatment (Ball & Links, 2009; Battle et al., 2004; Crowell, Beauchaine, & Linehan, 2009; Herman, Perry, & van der Kolk, 1989) and are associated with increased IPV (González, Igoumenou, Kallis, & Coid, 2016; Hines, 2008; Mauricio, 2007; Moore et al., 2018; Newhill, Eack, & Mulvey, 2009; Reuter, Sharp, Temple, & Babcock, 2014; Weinstein, Gleason, & Oltmanns, 2012; Whisman & Schonbrun, 2009). Although BPD symptoms may decrease over time, interpersonal problems and difficulties establishing meaningful relationships usually persist (Soloff & Chiappetta, 2018). Interpersonal stressors, such as real or perceived social rejection and abandonment, are among the most potent triggers of emotional distress in BPD (Emmelkamp & Kamphuis, 2007; Krause-Utz, Niedtfeld, Knauber, & Schmahl, 2017; Stiglmayr et al., 2005). Increased emotional distress due to rejection sensitivity, separation concerns, fear of abandonment, and intolerance of being alone, may in turn lead to impulsive aggression in BPD (Cackowski et al., 2017; Cackowski et al., 2014; Krause-Utz et al., 2016; Krause-Utz et al., 2013; Peters, Derefinko, & Lynam, 2017; Scott, Stepp, & Pilkonis, 2014; Scott et al., 2017).
Yet, it remains unclear whether a combination of borderline personality (BP) features (affective instability, self-harming impulsivity, instable self-image, and interpersonal disturbances) contributes to IPV in individuals with childhood trauma history. Although the link between BPD and IPV has been supported by several studies, most of these studies have focused on IPV perpetration (Clift & Dutton, 2011; Dutton, Lane, Koren, & Bartholomew, 2016; Hughes, Stuart, Gordon, & Moore, 2007; Jackson, Sippel, Mota, Whalen, & Schumacher, 2015; Weinstein et al., 2012). Even though both forms of IPV likely co-occur, the underlying mechanisms (e.g., role of specific BP features) regarding IPV perpetrating and victimization may not be the same.
Maladaptive stress coping might be another mechanism underlying the link between childhood maltreatment and IPV (Devries et al., 2013; Riggs et al., 2000; Stith et al., 2004), especially in individuals with BPD features who often lack functional coping and problem-solving skills (Lieb, Zanarini, Schmahl, Linehan, & Bohus, 2004; Peters et al., 2017; Scott et al., 2014; Scott et al., 2017).
Whether gender plays a significant role in this relationship is not yet completely understood. Men were found to perpetrate forms of IPV that cause physical injury at higher rates than women (see, for example, Archer, 2000). In BPD, intense anger and impulsive aggression, such as violent behavior in response to provocation, may be particularly prominent in men (Bradley, Conklin, & Westen, 2005; Ross & Babcock, 2009; Zlotnick, Rothschild, & Zimmerman, 2002). Maneta and colleagues (2013) found that BPD features are associated with both IPV perpetration and victimization in men, but with only victimization in women.
All in all, previous research revealed associations between childhood maltreatment, BPD, coping, and IPV. However, studies investigating links between all of these factors, differentiating between perpetration and victimization in both genders, are still needed. Understanding mechanisms through which BPD may contribute to IPV is key for prevention efforts.
This study aimed at investigating (a) whether BP features mediate the relationship between childhood maltreatment and IPV perpetration and victimization, (b) whether coping mediated this indirect effect, and (c) whether gender had a significant effect in this model. As previous research suggests that attachment may be a confounding factor in this relationship (Cameranesi, 2016; Dutton & White, 2012; Lawson & Brossart, 2013; McKeown, 2014), we additionally tested whether anxious attachment affected the results. More specifically, we were interested in both direct effect of childhood maltreatment on IPV and its indirect effect through BP features and coping, in female and male participants, while controlling for age and attachment style. We hypothesized that childhood maltreatment would positively predict IPV and that BP features would mediate this relationship. We further hypothesized that the mediating effect of BP features would be mediated by coping.
Material and Methods
Participants
The study was conducted at Leiden University, Leiden, the Netherlands. Participants were primarily (80%) recruited through online platforms for sufferer from domestic violence, BPD, and survivors of childhood maltreatment (international mental health online platforms that gave permission to post the survey on their home page). To gain a preferably large sample of participants with diverse background (mixed clinical and nonclinical community sample), participants were further recruited via the research participation website of Leiden University, the Netherlands (20%). Inclusion criteria were ability to understand and provide informed consent, age above 18 years, sufficient English proficiency, 1 indicating gender as either female or male, and having been in a long-term relationship, either at the moment or in the past. Overall, 1,864 responses were collected. Out of these respondents, 14 cases were post hoc excluded because they had indicated a lack of English proficiency. In addition, several respondents had to be excluded because they were not in a long-term relationship (n = 216) or terminated the survey before completing all scales (n = 925). Twenty participants indicated a gender other than female or male (“both” or “neither”) and were excluded from the final analysis. The final sample comprised 703 participants. Overall age ranged between 18 and 75 years (M ± SD = 28.49 ± 10.83). Approximately 75% (n = 537) were female, 25% were male (n = 166). Most participants were European (63%), followed by North American (28%), Asian (3%), South American and Middle East (1.5% each) and others (3%). Majority of the sample was single (33%), almost half (45%) reported that they have been in a relationship within the last 6 months. Approximately 63% have received higher education. Complete demographic variables of the sample (n = 703) can be found in Supplemental Table 2. Women and men did not differ significantly in age (28.20 ± 10.23 vs. 29.31 ± 10.93), t(702) = 1.21, p = .228; education, = 39.71, p = .196; nationality, = 7.49, p = .278; employment, = 0.10, p = .951; and relationship status, = 17.34, p = .299.
The final sample did not differ significantly from participants who provided demographic information but did not complete the survey, regarding age, t(536) = 0.46, p = .536; gender, = 0.04, p = .836; nationality, = 149.76, p = .252; employment, = 2.67, p = .262; and relationship status, = 0.11, p = .741. However, they differed in education level, = 25.28, p = .008, with those competing the survey reporting higher education level.
Material
Childhood maltreatment severity was assessed using the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998), a self-report scale assessing emotional, sexual, and physical abuse; emotional neglect; and physical neglect (25 items, between 1 = never true and 5 = very often true). Each of the five subscales comprises five items. The CTQ has demonstrated good psychometric properties, with test–retest reliability ranging from .79 to .84, internal consistency coefficients between α = .66 and .92, and good convergent validity with therapist ratings (Bernstein & Fink, 1998). In the current sample, internal consistency (Cronbach’s α) was very good to excellent for all subscales (emotional abuse: α = .93; emotional neglect: α = .93; sexual abuse: α = .99; physical abuse: α = .88), except for physical neglect, which showed good internal consistency (α = .68).
BPD features were assessed using the Personality Assessment Inventory–Borderline Feature Scale (PAI-BOR; Jackson & Trull, 2001). This self-report scale was derived from the Personality Assessment Inventory (Morey, 1991), guided by theoretical (diagnostic) conceptualizations, empirical research, and evaluation of psychometric properties. The final 24 items (between 0 = false and 3 = very true) refer to the four subscales “Affective Instability,” “Identity Diffusion,” “Self-Harm,” and “Negative Relationships.” These four subscales were used to assess the specific BPD features of interest: (a) “Affective Instability” (intense and instable emotions, for example, “My moods get quite intense,” “My mood can shift quite suddenly”); (b) “Identity Diffusion” (instable self-image and sense of self, for example, “My attitude about myself changes a lot”); (c) “Negative Relationships” (interpersonal disturbances, such as fear of abandonment, [“I worry a lot about other people leaving me,” “I can’t handle separation from those close to me very well”] and instable and intense relationships [“Once someone is my friend, we stay friends.” [R], “My relationships have been stormy”]); and (d) “Self-harm” (potentially self-damaging impulsivity, for example, “I’m too impulsive for my own good,” “I sometimes do things so impulsively that I get into trouble,” “When I’m upset, I typically do something to hurt myself”). A total score above of ≥60 suggests clinically significant BP features (Jackson & Trull, 2001). The PAI-BOR has shown strong psychometric properties (internal consistencies between α = .81 and .86) across normative, student and clinical samples (Jackson & Trull, 2001). In the present sample, Cronbach’s α of the PAI-BOR subscales was good to very good for all subscales (between α = .72 and .84).
IPV was assessed using the Conflict Tactics Scale–Revised (CTS2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996). This 78-item scale asks pairs of questions, referring to both the “self” (perpetration) and “partner” (victimization). The five subscales measure “Negotiation” (e.g., “showed my partner I cared even though we disagreed”), “Psychological Aggression” (e.g., “called my partner fat or ugly,” “shouted or yelled at my partner”), “Physical Assault” (e.g., “threw something at my partner that could hurt,” “twisted my partner’s arm”), and “Sexual Coercion” (e.g., “used force to make my partner have sex”). “Injury” measures injuries of the “partner” (perpetration) and the “self” (victimization) Item are answered on a 6-point scale, indicating how often the respective behavior has occurred (between 0 = never and 6 = more than 20 times in the relationship). The CTS2 has shown strong psychometric properties, including good construct and good discriminant validity and good internal consistency (Cronbach’s α between .79 and .95; Straus et al., 1996). In the current study, Cronbach’s α was good to excellent for negotiation (self/partner: α = .93/.92), psychological aggression (α = .82/.86), physical assault (α = .86/.91), and injury (α = .78/.78), whereas for the subscale Sexual Coercion, internal consistency was good for the victimization items (α = .74) but low for the perpetration items (α = .57).
Coping was assessed using the 18-item short version of the Cognitive Emotion Regulation Strategies Inventory (CERQ; Garnefski & Kraaij, 2006), measuring the use of nine cognitive emotion regulation strategies after having experienced a negative life event: (between “1 = almost never” and “5 = almost always”). Higher scores on the subscales “Rumination” (repetitive thinking about aspects and feelings associated with the event), “Catastrophizing” (emphasizing the terror of the experience), “Self-Blame” and “Other-Blame” have been linked to more mental health problems, thus being regarded as “maladaptive” strategies (Garnefski, Kraaij, & Spinhoven, 2001). Higher use of “positive reappraisal” (attaching a positive meaning to the event, for example, in terms of personal growth), “positive refocusing,” “putting into perspective,” “planning,” and “ acceptance” has been associated with lower levels of stress, depression, and anxiety (Lazarus & Folkman, 1984; Martin & Dahlen, 2005), thus being regarded as “symptom protective” or “adaptive” strategies (Garnefski et al., 2001). All subscales showed good internal consistencies and reliability (Garnefski & Kraaij, 2006; Garnefski et al., 2001). In the current study, internal consistencies for the subscales were good (between α = .64 and .86) except for the subscales “Acceptance” and “Other-Blame” (α < .29).
Participants further completed the 18-item Revised Adult Attachment Scale (AAS-R, Collins & Read, 1990), which measures the three dimensions “close” (extent to which closeness and intimacy are comfortable), “dependent” (ability to depend on others’ availability in need), and “anxious” (vulnerability to abandonment and rejection; between “1 = not at all characteristic of me” and “5 = very characteristic of me”). Based on these item scores, attachment anxiety and security can be calculated (Graham & Unterschute, 2015; Cronbach’s α = .77-.86).
Procedure
The study was approved by the Ethics Committee of the psychology department of Leiden University. Participants were provided with contact details of the principal investigator (A.K.), a trained clinical psychologist, whom they could contact in case of discomfort experienced due to the intimate nature of the items. Data collection took place between March 2016 and July 2017 through an online survey using the software Qualtrics© (2015, Qualtrics, Provo, UT). All participants were informed about the aim and background of the study, including potential risks, reimbursement for study participation (chance of winning one of eleven 25€ vouchers or study credits), and the right to terminate the survey at any point of time without consequences. Access to the survey was only possible after agreeing on the informed consent and indicating sufficient English proficiency. First, respondents were asked to provide information on demographic variables (age, gender, education, nationality, and relationship status). Afterward, the CTQ, PAI-BOR, CTS2, CERQ, Multidimensional Scale of Perceived Social Support (MSPSS), Self-Harm Inventory (SHI), and AAS-R were presented in randomized order. Participants were further completed scales on self-harming behaviors (Self-Harm Inventory, Sansone & Sansone, 2010), and social support (MSPSS, Zimet, Powell, Farley, Werkman, & Berkoff, 1990). After completing these scales, participants were asked to provide information about current and previous psychopharmacological and psychotherapeutic treatment, and psychiatric diagnoses. Finally, participants were fully debriefed and asked whether they were “. . . unable to answer one or more questions due to a lack of English proficiency” (a YES response led to post hoc exclusion from the analysis). Participants were again explicitly encouraged to contact the principal investigator in case of discomfort experienced due to the intimate nature of the items (18 participants made use of this opportunity). The survey took ~35 to 45 min to complete. Respondents had the opportunity to participate in a lottery (chance of winning one of eleven 25€ Amazon© vouchers). Psychology students could alternatively choose to gain study credits.
Statistical Analysis
Software IBM SPSS Statistics for Windows (Version 21.0, Armonk, NY) was used for data analysis. Significance level for all analyses was set at p < .05, two-tailed. Childhood maltreatment severity and BP features were represented by sum scores of the CTQ and the PAI-BOR items, respectively. To create a score for coping, CERQ items for “positive reappraisal,” “positive refocusing,” “putting into perspective,” and “planning,” “self-blame,” “rumination,” and “catastrophizing” were created. The subscales “Other-Blame” and “Acceptance” were not included because internal consistency of these subscales was insufficient (α < .29). For scoring of the CTS2, midpoints for each response category were created (e.g., 3-5 times was recoded into 4; see Straus, 2004). To create a total score for IPV perpetration, scores for “psychological aggression,” “physical assault,” “sexual coercion” by the “self” and “injury” of the partner were summed up. To obtain a score for IPV victimization, a sum score for “psychological aggression (partner),” “physical assault (partner),” “sexual coercion (partner),” and “injury (self)” was created.
Prior to the analysis, assumptions of linearity, normality of residuals, homoscedasticity and independence of residuals, and outliers (Cook’s distance, Leverage values) were checked. Multicollinearity between predictors was not of concern according to tolerance values. Correlations between all measures can be found in Supplemental Table 1. To detect relevant covariates, correlations between CTQ and CTS2 scores with demographics (age, gender, education, nationality, employment, relationship status) were performed. Age and gender were identified as relevant covariates, being significantly correlated with both variables (p < .01, all other: p > .05).
Childhood maltreatment severity (CTQ scores) was considered as predictor (X variable). IPV (CTS2 scores for victimization and perpetration, respectively) was defined as dependent variables (Y variables). BP features (PAI-BOR scores) were conceptualized as primary mediator (M1) and coping strategies (CERQ score) as secondary mediator variable (M2). Path c corresponds to the total effect of childhood maltreatment severity on IPV outcomes, when the effect through BPD features and coping is not accounted for. Path c′ corresponds to the direct effect of childhood maltreatment on IPV, when taking effects of the mediator variables (BPD features, coping) into account. Path a corresponds to the effects of the predictor variable on the mediator variable, whereas Path b refers to the effect of each mediator variable on the outcome variable. The indirect effects of the X variable through the mediator variable on the Y variable are the product of these two paths. The model also evaluates interactions between the mediator variables in predicting the outcome variable, in terms of a mediation of mediation.
As it has been recommended to establish the basic association between the underlying factors of the mediation model (Baron & Kenny, 1986; Hayes, 2013), several linear regression analyses were performed prior to the mediation analysis: First, a multiple linear regression with CTQ sum score as predictor and CTS2 scores (for victimization and perpetration, respectively) as dependent variable was conducted, controlling for age and gender (Path c). In case of a significant overall effect, the subscales instead of the total scores were entered in a multivariate regression analysis. The same analyses were performed with the PAI-BOR scores as predictor and CTS2 scores as dependent variable (Path b1). In addition, a multiple regression analysis (and follow-up multivariate regression analysis) was used to test whether childhood maltreatment severity significantly predicted BP features (Path a1), suggesting that a mediation might occur. For matter of completeness, the same analyses were performed to test assumptions for the second mediator (Path a2, Path b2). For significant effects, effect sizes are reported.
To quantify the total, direct, and indirect effect of childhood maltreatment severity on IPV outcomes through BPD features as well as coping strategies, Hayes’s (2013) PROCESS tool for SPSS (Model 6) was used. The PROCESS tool is based on a nonparametric bootstrapping procedure, which calculates regression coefficients of the overall mediation model and generates bias-corrected confidence intervals (CIs) for total, direct, and indirect effects. A bootstrap function based on n = 5,000 samples and a CI of 95% was used. Age and gender were included as covariates. For significant indirect effects, standardized effects are reported. In a separate analysis, it was tested whether results remained significant after controlling for attachment and nationality.
Results
Sample Description
Participants reported a broad range of childhood maltreatment, IPV, and BP features (see Table 1). In total, 284 participants (40.4%) scored higher than 60 on the PAI-BOR, suggesting clinically significant BPD features; this was significantly more frequently the case in female participants (n = 251, 45%) than in male participants (n = 43, 26%; χ2 = 18.96, p < .001). Sixty-one percent of the participants have been seeking psychotherapeutic treatment, while 25% of participants have been receiving psychotropic medication; significantly more women than men reported that they have been seeking psychotherapeutic treatment and received one or more clinical diagnosis (65% vs. 49% and 53% vs. 32%, respectively; see Supplemental Table 2). As shown in Table 1, women reported significantly more BP features, maladaptive coping strategies, anxious attachment, and less perceived social support from friends and family than men. Moreover, women reported significantly higher severity of childhood trauma, particularly a higher frequency of moderate to extreme abuse (emotional abuse: n = 355, 66%; physical abuse: n = 185, 34%; sexual abuse: n = 181, 33%) and neglect (emotional: n = 432, 80%; physical: n = 439, 82%) compared with the male sample: 48% of male reported moderate to extreme emotional abuse, 20% (n = 33) physical abuse, 14% reported (n = 24) sexual abuse, 82% reported (n = 136) emotional neglect, and 84% reported (n = 139) physical neglect.
Table 1.
Distribution of CTQ, PAI-BOR, CTS2 Frequency Scores, CERQ, MSPSS, and AAS-R.
| Variable | Females (n = 537) |
Males (n = 166) |
t tests, t(df), p
U tests, U(df), p |
|---|---|---|---|
| CTQ sum | 57.43 ± 15.76 | 51.46 ± 13.19 | t(702) = 4.86, p < .0001 |
| Emotional abuse | 13.33 ± 6.78 | 9.98 ± 5.38 | t(702) = 6.56, p < .0001 |
| Emotional neglect | 15.87 ± 6.16 | 16.62 ± 6.12 | t(702) = 1.38, p = .170 |
| Physical abuse | 8.07 ± 4.58 | 7.08 ± 4.05 | t(702) = 2.68, p = .008 |
| Physical neglect | 11.89 ± 3.19 | 11.54 ± 3.25 | t(702) = 0.22, p = .280 |
| Sexual abuse | 8.07 ± 5.97 | 6.25 ± 3.49 | t(702) = 5.42, p < .0001 |
| PAI-BOR sum (BPD features) | 59.38 ± 15.59 | 52.43 ± 13.88 | t(702) = 5.48, p < .0001 |
| Affective instability | 15.72 ± 4.62 | 13.55 ± 4.46 | t(702) = 5.35, p < .0001 |
| Identity disturbances | 15.89 ± 4.55 | 14.23 ± 4.41 | t(702) = 4.16, p < .0001 |
| Negative relationships | 15.55 ± 4.55 | 13.50 ± 3.87 | t(702) = 5.58, p < .0001 |
| Self-harm | 12.22 ± 4.64 | 11.16 ± 3.88 | t(702) = 2.93, p = .004 |
| CTS2 (IPV) perpetration | 78.20 ± 55.19 | 72.82 ± 73.90 | U(702) = 1.93, p = .053 |
| Psychological aggression (perpetration) | 40.28 ± 35.36 | 32.54 ± 32.86 | U(292.55) = 2.98, p = .003 |
| Physical assault (perpetration) | 19.49 ± 19.45 | 17.98 ± 25.24 | U(702) = 1.74, p = .082 |
| Sexual coercion (perpetration) | 11.43 ± 10.56 | 14.60 ± 17.93 | U(702) = 2.70, p = .007 |
| Injury (perpetration) | 7.00 ± 5.10 | 7.69 ± 11.50 | U(702) = 0.06, p = .955 |
| CTS2 (IPV) victimization | 90.68 ± 90.66 | 84.88 ± 88.90 | U(702) = 0.54, p = .591 |
| Psychological aggression (victimization) | 40.35 ± 40. 67 | 37.36 ± 38.14 | U(702) = 0.89, p = .374 |
| Physical assault (victimization) | 23.46 ± 31.34 | 23.22 ± 32.65 | U(702) = 1.71, p = .087 |
| Sexual coercion (victimization) | 17.76 ± 22.44 | 15.11 ± 18.06 | U(702) = 0.91, p = .363 |
| Injury (victimization) | 9.14 ± 11.43 | 9.20 ± 13.31 | U(702) = 0.36, p = .824 |
| CERQ (mean) (coping) | 2.69 ± 0.64 | 2.90 ± 0.75 | t(702) = 3.62, p < .0001 |
| MSPSS total score | 15.47 ± 4.16 | 15.76 ± 3.74 | t(702) = 1.79, p = .075 |
| Family Friends |
4.58 ± 1.99 5.19 ± 2.00 |
4.86 ± 1.70 5.52 ± 1.61 |
t(702) = 2.54, p < .0001 t(702) = 0.79, p = .431 |
| Secure attachment (AAS-R) | 4.81 ± 1.10 | 5.11 ± 0.98 | t(702) = 2.85, p = .004 |
| Anxious attachment (AAS-R) | 5.69 ± 1.77 | 4.97 ± 1.74 | t(702) = 4.29, p < .0001 |
Note. Table shows M ± SD of scores and results of t tests or (nonparametrical) Mann–Whitney U tests. CTQ = Childhood Trauma Questionnaire; PAI-BOR = Personality Assessment Inventory–Borderline Features; CTS2 = Conflict Tactics Scale; CERQ = Cognitive Emotion Regulation Questionnaire; MSPSS = Multidimensional Scale of Perceived Social Support; BPD = borderline personality disorder; IPV = intimate partner violence; AAS-R = Adult Attachment Scale–Revised.
Approximately 84% of the participants (n = 588) reported at least one form of IPV perpetration toward an intimate partner (psychological aggression: 84%, physical assault: 39%, sexual coercion: 29%, injury: 11%). Approximately 82% of the participants (n = 575) reported experiencing psychological aggression, 38% experienced physical assault, 42% experienced sexual coercion, and 18% experienced severe injury. In 82.5% of the cases (n = 580), IPV was reciprocal, that is, perpetrated by oneself and experienced by the partner. There were no significant gender differences in self-reported frequency of IPV victimization and IPV perpetration (see Table 1). However, there was a trend concerning overall frequency and type of perpetration: Women reported significantly more psychological aggression, whereas men reported significantly more sexual violence.
Multiple and Multivariate Regression Analyses
Complete results can be found in Supplemental Tables S3 to S6.
Childhood maltreatment and IPV
The multiple regression analyses revealed a significant positive effect of childhood maltreatment on IPV perpetration, t(702) = 5.63, p < .0001, B = 0.84, SE = 0.15, β = .22, as well as victimization, t(702) = 5.16, p < .0001, B = 1.15, SE = 0.22, β = .20, when controlling for age and gender (Path c). Among the five CTQ subscales, Emotional Abuse, Physical Abuse, and Neglect significantly predicted IPV perpetration, while Emotional Abuse and Neglect as well as Physical Neglect were significant predictors for victimization (Table S3).
BP features and IPV
The multiple regression analyses revealed a significant positive effect of BP features on IPV perpetration, t(702) = 10.93, p < .0001, B = 1.52, SE = 0.14, β = .39, and IPV victimization, while controlling for age and gender, t(702) = 7.59, p < .0001, B = 1.62, SE = 0.21, β = .28 (Path b1). “Affective instability,” “negative relationships,” and “self-harm” positively predicted IPV perpetration, while victimization was predicted by “negative relationships” (Table S4).
Childhood maltreatment and BP features
Childhood maltreatment had a significant positive predictive effect on BPD features, t(702) = 10.32, p < .0001, B = 0.371, SE = 0.036, β = .368 (Path a1). All types of abuse and neglect were significant predictors (Table S5).
Coping
Coping significantly predicted IPV perpetration, t(702) = 10.93, p < .0001, B = 1.518, SE = 0.139, β = .391, and victimization, t(702) = 3.33, p = .001, B = 1.19, SE = 0.36, β = .12, controlling for age and gender (Table S6). Moreover, childhood maltreatment significantly predicted coping, F = 20.19, R2 = .17, = .16; t(702) = 7.13, p < .0001, B = 0.09, SE = 0.01, β = .27.
BP features and coping
A multiple regression analysis with coping (CERQ score) as dependent variable and BP features (PAI-BOR) as predictors revealed a positive relationship, t(702) = 21.77, p < .0001, B = 0.39, SE = 0.02, β = .65, while controlling for age and gender.
Mediation Analysis
As the preliminary analyses suggested that a mediation effect may occur for both BP features and coping, the subsequent mediation analysis included both mediator variables (M1: BP features, M2: coping) as well as age and gender as covariates. Results are depicted in Figure 1.
Figure 1.
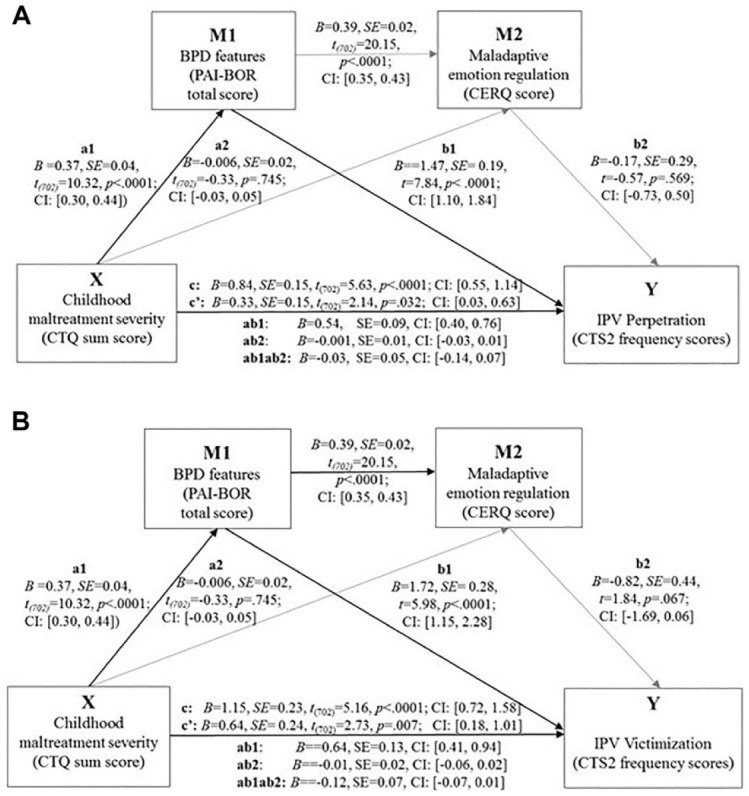
This figure depicts results of the mediation analysis for IPV perpetration (A), and victimization (B).
Note. Significant paths are highlighted in darker color. Path c corresponds to the total effect of childhood maltreatment (X variable) on IPV victimization and perpetration (Y variable) when the effect through the intervening variables is not accounted for. Path c′ corresponds to the direct effect of childhood maltreatment on IPV when effects of the intervening variables are accounted for. Path a1 and Path a2, respectively, refer to the effects of the predictor variable (X variable) on the intervening variables (M1 and M2). Path b1 and b2, respectively, correspond to the effect of each intervening variable on the outcome variable (Y variable). Path a1b1 and Path a2b2, respectively, are the indirect effects of the X variable through the intervening variable on the Y variable. BPD = borderline personality disorder; PAI-BOR = Personality Assessment Inventory–Borderline Feature Scale; CI = confidence interval; CERQ = Cognitive Emotion Regulation Questionnaire; CTQ = Childhood Trauma Questionnaire; IPV = intimate partner violence; CTS2 = Conflict Tactics Scale–Revised.
Perpetration
The overall regression model for IPV perpetration was significant, F(6, 695) = 25.22, p < .0001, R = .40, R2 = .15. With all predictors in the model, childhood maltreatment severity, B = 0.33, SE = 0.16, t(702) = 2.13, p = .033, CI = [0.03, 0.63], and BP features, B = 1.47, SE = 0.19, t(702) = 7.84, p < .0001, CI = [1.10, 1.83], were both significant predictors, while coping, B = 0.16, SE = 0.29, t(702) = 0.57, p = .569, CI = [−0.74, 0.41]; gender, B = 6.21, SE = 5.07, t(702) = 1.23, p = .220, CI = [−0.28, 0.55]; and age, B = 0.14, SE = 0.21, t(702) = 0.67, p = .504, CI = [−0.27, 0.55], had no significant effects. As shown in Figure 1A, the total effect of childhood maltreatment on IPV perpetration was significant (Path c), and so was the direct effect (Path c′), indicating that childhood trauma severity still significantly predicted IPV perpetration, when taking the mediators into account. There was a significant indirect effect of childhood trauma severity via BP features on IPV perpetration (completely standardized effect: B = 0.13, SE = 0.02, CI = [0.10, 0.19]). Path a1 and b2 were significant. There was also a significant link between BPD features and maladaptive coping. However, no significant indirect effects through coping were observed.
Results remained stable after controlling for anxious attachment (B = 8.24, SE = 4.15, t = 1.98, p = .047, CI = [−16.40, −0.10]; indirect effect through BP features: B = 0.17, SE = 0.06, CI = [0.05, 0.29]). Furthermore, results remained stable when controlling for nationality (B = 0.27, SE = 1.72, t = 0.16, p = .874, CI = [−3.67, 3.13]; indirect effect through BP features: B = 0.30, SE = 0.10, CI = [0.15, 0.53]).
Victimization
For IPV victimization, the overall regression model was significant, F(7,695) = 18.35, p < .0001, R = .34, R2 = .12, with both childhood maltreatment severity, B = 0.63, SE = 0.23, t(702) = 2.73, p = .007, CI = [0.18, 1.10], and BP features, B = 1.72, SE = 0.28, t(702) = 5.98, p < .0001, CI = [1.15, 2.28], as well as age, B = 1.51, SE = 0.33, t(702) = 4.67, p < .0001, CI = [0.87, 2.14], being significant predictors. There was a trend for a significant effect of coping, B = −0.82, SE = 0.45, t(702) = 1.83, p = .067, CI = [−1.69, 0.05]. Gender, B = 6.28, SE = 7.76, t(702) = 0.81, p = .418, CI = [−1.69, 0.06], had no significant effect. As shown in Figure 1B, both the total effect and the direct effect of childhood maltreatment severity on victimization were significant. In addition, there was a significant indirect effect of childhood maltreatment through BPD features (B = 0.011, SE = 0.02, CI = [0.07, 0.15]). Path a1 and Path b1 were significant. No significant indirect effects through coping were observed.
Anxious attachment was identified as additional significant predictor (B = 4.62, SE = 2.10, t = 2.19, p = .028, CI = [−8.76, −0.49]) but did not alter results (direct effect: B = 0.56, SE = 0.24, t = 2.31, p = .021, CI = [0.08, 1.03]; indirect effect through BP features: B = 0.16, SE = 0.07, CI = [0.05, 0.32]). Furthermore, results remained stable when controlling for nationality (B = 0.44, SE = 4.33, t = 0.10, p = .919, CI = [−9.01, 8.13]; indirect effect through BP features: B = 0.48, SE = 0.26, CI = [0.29, 1.14]).
Follow-up analysis
As BP features were a significant mediator between childhood maltreatment and IPV, we performed an exploratory follow-up analysis with the four PAI-BOR subscales instead of the total PAI-BOR scale as mediators. Coping was not included as secondary mediator, as no indirect effects through coping had been observed. Table 2 summarizes results for total, direct, indirect effects, and interactions between indirect effects (mediated mediation).
Table 2.
Results of the Follow-Up Mediation Analysis for the BP Features Separately.
| Perpetration | |
| Total effect CM | B = 0.84, SE = 0.15, t(702) = 5.63, p < .001, CI = [0.55, 1.14] |
| Direct effect CM | B = 0.33, SE = 0.15, t(702) = 2.18, p = .030, CI = [0.03, 0. 63] |
| Indirect effects of BP features | |
| AI | B = 0.22, SE = 0.07, CI = [0.09, 0.36] (B = 0.05, SE = 0.01, CI = [0.02, 0.09]) |
| ID | B = −0.04, SE = 0.03, CI = [−0.11, 0.003] |
| NR | B = 0.08, SE = 0.03, CI = [0.03, 0.14] (B = 0.02, SE = 0.01, CI = [0.01, 0.03]) |
| SH | B = 0.04, SE = 0.02, CI = [−0.02, 0.10] |
| Interaction effects (mediated mediation) | |
| AI→ID | B = −0.07, SE = 0.04, CI = [−0.17, 0.00] |
| AI→NR | B = 0.06, SE = 0.04, CI = [0.02, 0.11] (B = 0.01, SE = 0.06, CI = [0.01, 0.03]) |
| AI→SH | B = 0.06, SE = 0.02, CI = [0.03, 0.11] (B = 0.02, SE = 0.01, CI = [0.01, 0.03]) |
| AI→ID→NR | B = 0.06, SE = 0.02, CI = [0.02, 0.11] (B = 0.02, SE = 0.01, CI = [0.05, 0.03]) |
| AI→ID→SH | B = 0.03, SE = 0.01, CI = [0.01, 0.06] (B = 0.01, SE = 0.01, CI = [0.003, 0.2]) |
| AI→SH→NR | B = 0.01, SE = 0.04, CI = [0.002, 0.20] (B = 0.01, SE = 0.01, CI = [0.00,0.01]) |
| ID→NR | B = 0.04, SE = 0.02, CI = [0.01, 0.07] (B = 0.01, SE = 0.01, CI = [0.002,0.02]) |
| ID→SH | B = 0.02, SE = 0.01, CI = [0.01, 0.04] (B = 0.01, SE = 0.002, CI = [0.00,0.01]) |
| ID→NR→SH | B = 0.004, SE = 0.01, CI = [0.01,0.01] (B = 0.01, SE = 0.01, CI = [0.003,0.003]) |
| SH→NR | B = 0.01, SE = 0.01, CI = [0.003,0.02] (B = 0.002, SE = 0.001, CI = [0.01,0.01]) |
| AI→ID→NR→SH | B = 0.01, SE = 0.004, CI = [0.002,0.02] (B = 0.02, SE = 0.01, CI = [0.001,0.004]) |
| Victimization | |
| Total effect CM | B = 1.15, SE = 0.23, t(702) = 5.16, p < .001, CI = [0.71, 1.58] |
| Direct effect CM | B = 0.53, SE = 0.23, t(702) = 2.31, p = .021, CI = [0.08, 0.99] |
| Indirect effects of BP features | |
| AI | B = −0.02, SE = 0.10, CI = [−0.23, 0.16] |
| ID | B = −0.05, SE = 0.05, CI = [−0.16, 0.03] |
| NR | B = 0.22, SE = 0.06, CI = [0.12, 0.36] (B = 0.04, SE = 0.01, CI = [0.02, 0.06]) |
| SH | B = 0.02, SE = 0.02, CI = [−0.005, 0.10] |
| Interaction effects | |
| NR→AI | B = 0.17, SE = 0.07, CI = [−0.23, 0.05] |
| NR→ID | B = 0.10, SE = 0.03, CI = [0.05, 0.19] (B = 0.02, SE = 0.01, CI = [0.01, 0.03]) |
| NR→SH | B = 0.01, SE = 0.005, CI = [−0.001, 0.02] |
| NR→ID→SH | B = 0.002, SE = 0.002, CI = [−0.003, 0.01] |
Note. Table shows results of the mediation analysis with the PAI-BOR subscales (AI, ID, NR, and SH). For significant effects, completely standardized effects are reported in brackets. BP = borderline personality; CM = childhood maltreatment; AI = affective instability; ID = identity disturbance, NR = negative relationships; SH = self-harm.
Perpetration
Among the four subscales, “Affective Instability” and “Negative Relationships” were identified as significant mediators. Moreover, results suggest that the indirect effect of childhood maltreatment through “affective instability” was mediated by the three other BP features (“negative relationships,” “identity,” and “self-harm”; see Table 2).
Victimization
The subscale “Negative Relationship” was the only significant mediator for victimization. This indirect effect was further mediated by “identity” (see Table 2).
Discussion
The aim of this study was to investigate the effect of childhood maltreatment severity on IPV perpetration and victimization, and its indirect effect through BP features and maladaptive coping. There was a significant indirect effect through BP features. No indirect effects through coping and no effect of gender were found.
The positive relationship between childhood maltreatment and IPV is in line with our hypothesis and previous research (Capaldi et al., 2009; Jennings, Richards, Tomsich, & Gover, 2015; Linder & Collins, 2005; McMahon et al., 2015; Stith et al., 2004; Swinford et al., 2000; Whitfield et al., 2003; Widom et al., 2014). A history of childhood maltreatment, especially emotional and physical maltreatment, may increase the likelihood of perpetrating and re-experiencing violence in adult relationships (Bandura, 1973; Widom et al., 2014). In addition, we found strong significant associations between all forms of childhood maltreatment and BP features. Current conceptualizations propose that complex interactions between genetic, neurobiological predispositions, and traumatic experiences underlie the development of BPD (Ball & Links, 2009; Battle et al., 2004; Golier et al., 2003; Herman et al., 1989; Pietrek, Elbert, Weierstall, Müller, & Rockstroh, 2013; Yen et al., 2002; Zanarini, 2000).
In line with our hypothesis and previous research, BP features played a significant role in the relationship between self-reported childhood maltreatment severity and IPV. The presence of BPD features was found to be an important risk factor for IPV (Newhill et al., 2009), also when compared with other personality disorders, such as antisocial personality disorder (Weinstein et al., 2012). BPD symptoms were associated with higher rates of marital violence perpetration (Whisman & Schonbrun, 2009). Moreover, BPD features were associated with more teen dating violence (Hatkevich, Mellick, Reuter, Temple, & Sharp, 2020; Reuter et al., 2014). In line with this previous research, our findings suggest that the presence of BPD features may put individuals at higher risk for perpetrating and experiencing IPV. BPD may also be an important psychological factor underlying the relationship between growing up in an abusive environment and intimate violence in adult intimate relationships.
Follow-up analyses suggest that affective instability and interpersonal disturbances, alone and in interaction with identity disturbance and self-harming impulsivity, were relevant factors for IPV perpetration. Interestingly, interpersonal disturbances (e.g., fear of abandonment, intolerance of being alone, separation concerns), paired with instable self-image, was a significant factor for victimization, suggesting that a different psychological mechanism may be at play here. Survivors of childhood maltreatment, especially those with separation concerns and an instable self-image, may learn to believe that violence is a normal part of close relationships and respond with helplessness when confronted with violence in adult intimate relationships (Walker, 1977). Our results remained stable after controlling for anxious attachment, which suggests that anxious attachment alone does not significantly account for the observed findings (Dutton, 2002).
In contrast to our hypothesis, coping was not identified as a significant psychological factor in the relationship between childhood maltreatment, BPD, and IPV. There was no significant predictive effect of coping for perpetration and only a trend for victimization. In contrast to this, previous research has highlighted the role of stress coping in the cycle of violence, for example, individuals with a history of childhood abuse may have learned to believe that violence is an acceptable strategy for coping with conflicts in close relationships (Bandura, 1973; Cappell & Heiner, 1990; Franklin & Kercher, 2012; Walker, 1977). Moreover, previous research suggests that aggressive and impulsive behavior in BPD is primarily observed under emotional distress and may reflect a lack of adaptive coping strategies (Cackowski et al., 2017; Cackowski et al., 2014; Krause-Utz et al., 2016; Krause-Utz et al., 2013; Scott et al., 2014; Scott et al., 2017). A possible explanation for these inconsistencies is that in the present study coping was measured with the CERQ, which focuses on cognitive coping strategies (Garnefski et al., 2001) and might not capture general difficulties in emotion regulation (Gratz & Roemer, 2004). Although both constructs are related, for example, emotional dysregulation can result from an inability to downregulate negative emotions through cognitive strategies (Ochsner & Gross, 2005), it might very well be that other behavioral aspects, not assessed by the CERQ, mediate the relationship between BP features and IPV. For example, problematic alcohol use was found to play an important role in the relationship between BP features and IPV (Armenti, Snead, & Babcock, 2018; Jackson et al., 2015). Moreover, impulsivity, especially in the context of negative emotions, may play an important role here (Peters et al., 2017). Future studies should include scales on behavioral aspects of coping (e.g., problematic substance use) difficulties in emotion regulation, anger, and impulsivity to further clarify these discrepancies.
Gender did not have a significant effect on IPV perpetration and victimization either. Previous research suggests that women and men are equally likely to perpetrate or to experience IPV, with the most common form of IPV being reciprocal (e.g., Capaldi et al., 2012; Whitaker et al., 2007). Some studies even found somewhat higher rates of IPV perpetration in women than in men (see, for example, Capaldi et al., 2012) while females may also experience a wider range of poor mental health outcomes (Afifi et al., 2009). Consistent with these earlier findings (Capaldi et al., 2012), in the present study, women tended to report higher rates of psychological aggression and physical assault toward their partners, while male participants tended to report more sexual coercion. This again argues for a more gender-balanced view with reciprocal violence being the most prevalent form of IPV. Regarding the role of gender in the link between BPD and IPV, previous research found more impulsive (reactive) aggression in men with BPD (Bradley et al., 2005; Ross & Babcock, 2009; Zlotnick et al., 2002) and more victimization in women with BPD features (Maneta et al., 2013). In contrast, in the present study, gender did not play a significant role in this relationship. Higher age was related to lower self-reported BPD features. Yet, it is important to highlight that interpersonal disturbances usually persist, with increasing age, in BPD (e.g., Soloff & Chiappetta, 2018). Therefore, it is important to involve longitudinal measures and different age groups in future studies on associations between childhood trauma, BPD features, and IPV.
To our knowledge, this is the first study investigating the role of BP features as well as coping in the relationship between childhood maltreatment on IPV perpetration and victimization, in a mixed (clinical and nonclinical) sample of female and male participants. Findings may help to deepen the understanding of psychological mechanisms underlying IPV. Strengths are the relatively large sample of both clinical and nonclinical participants. When interpreting our findings, one must be aware of several limitations. Due to the cross-sectional correlational design, no causal conclusions can be drawn, for example, it remains unclear whether BP features predate and/or follow IPV. As childhood maltreatment and other variables were assessed in a retrospective and subjective manner, we cannot rule out that participants’ responses were biased, for example, due to a lack of awareness, different subjective interpretations of measured concepts, minimizing/denial or social desirability. Individuals with higher levels of BP features may be more likely to remember and report more severe childhood abuse, suffering from more traumatic re-experiencing, associated with more vivid negative memories (Baker, 2009). Almost half of our sample did not complete the survey, which might have caused a selection bias. Although those completing the survey did not differ significantly in other demographic variables, they reported higher education level than participants who did not complete the survey. The unequal distribution (3:1) of females and males in our sample may be representative for clinical samples but nonetheless hinder interpretation of results regarding gender. More research with a stronger gender balance is needed to replicate our findings and to understand whether certain BP features increase the likelihood of IPV. Prospective studies will help gaining more insights into causal relationships between childhood abuse, BP features, coping, and IPV. Future research should investigate IPV in systems and interpersonal contexts, for example, in couples with BPD. It is possible that a confounding variable, such as another form of psychopathology, might explain the present results. Therefore, future research should investigate the possibility that other personality characteristics or symptoms (e.g., posttraumatic stress or depressive symptoms) play a role in the link between BPD and IPV. Besides impulsivity, anger, and antisocial personality features (Peters et al., 2017; Riggs et al., 2000), substance abuse may increase the risk for IPV (Afifi et al., 2009; Riggs et al., 2000). Those who abused alcohol or drugs were not only more likely to have BPD features but also to perpetrate more severe forms of violence toward a partner compared with nondrug users (Jackson et al., 2015).
To conclude, our results suggest a strong association between traumatic childhood experiences and IPV, which may be partly influenced by the presence of BP features, especially affective instability and interpersonal disturbances. This might have strong clinical implications, as childhood maltreatment may not only increase the risk for developing BPD features, but this may also pave the way for a pattern of revictimization and perpetration. BPD is often underdiagnosed or misdiagnosed, especially in men (Grant et al., 2008), which may result in a lack of appropriate treatment interventions. Screening for BPD features may therefore be an important step in IPV prevention. Couple-oriented psychoeducation about reciprocal and dynamic conceptualizations of IPV may be another essential part of working with this risk group. Teaching emotion regulation strategies and social interaction skills is an essential component of evidence-based treatments for BPD, including Dialectical Behavior Therapy (DBT; Linehan, 1993), Mentalization-Based Therapy (Fonagy & Bateman, 2008), Schema Therapy (Arntz & van Genderen, 2009; Young, 1990), and Transference-Focused Psychotherapy (Yeomans, Clarkin, & Kernberg, 2015). Skills training, for example, in the context of DBT, has also been proven to be successful in treating male IPV perpetrators with BPD features (McKeown, 2014). Violence reduction training (group therapy in social problem-solving) led to a decrease of overall levels of negative anger strategies (Gerhart, Holman, Seymour, Dinges, & Ronan, 2015), especially in participants with BP features (Gerhart, Ronan, Russ, & Seymour, 2013). Furthermore, intervention, targeting IPV in individuals with BPD features may focus on increasing self-control during distress by involving mindfulness techniques (Peters et al., 2017), for example, as implemented in DBT (Linehan, 1993). Training in social-emotional processing (e.g., differentiating ambiguous facial expressions, while addressing rejection or separation concerns and fear of abandonment) in individuals with BPD may further help to reduce the number of IPV perpetrators and victims and to break the cycle of abuse and violence.
Supplemental Material
Supplemental material, Supplemental_Tables_2-6 for Childhood Maltreatment, Borderline Personality Features, and Coping as Predictors of Intimate Partner Violence by Annegret Krause-Utz, Lea J. Mertens, Julian B. Renn, Pauline Lucke, Antonia Z. Wöhlke, Charlotte C. van Schie and Joanne Mouthaan in Journal of Interpersonal Violence
Supplemental material, Supplemental_Table_1 for Childhood Maltreatment, Borderline Personality Features, and Coping as Predictors of Intimate Partner Violence by Annegret Krause-Utz, Lea J. Mertens, Julian B. Renn, Pauline Lucke, Antonia Z. Wöhlke, Charlotte C. van Schie and Joanne Mouthaan in Journal of Interpersonal Violence
Acknowledgments
The authors thank all participants of this study for their essential contribution. They also thank Myrto Alampanou, Li-Ling Athime, Leonie J. R. Cloos, Marjon de Vries, Elsemieke Hoevenaren, Katarina Jensen, Winglet W. Law, Mirella Lindström, Nadja Ludwig, Stefanie Kloos, Nina Marinov, Niké Planken, Lavinia Przyborowski, Sarah Rein, Philine Rojczyk, Esther Thebock, and Daniela van der Linden for data collection.
Author Biographies
Annegret Krause-Utz is currently working as assistant professor in clinical psychology at Leiden University. She obtained a medical PhD at the Medical Faculty of Heidelberg University in Germany (2014, supervisor Prof. Christian Schmahl) and a PhD in psychology at Leiden University (2017). She was also trained in behavior therapy and dialectical behavior therapy. She has worked with individuals with borderline personality disorder (BPD) and complex trauma (e.g., childhood abuse and neglect). Understanding the underlying mechanisms of BPD, such as emotion dysregulation and dissociation, is also her main research interest, combining different methods such as self-reports, experimental-tasks, and neuroimaging.
Lea J. Mertens is a research master student in cognitive and clinical neuroscience at Maastricht University, specializing in neuropsychology. She did her Bachelor’s in Psychology at Leiden University, during which she conducted research on borderline personality and intimate partner violence under the supervision of Dr. A. Krause-Utz. Now, her research interests mainly lie in disease and treatment mechanisms of psychiatric disorders, with a particular focus on psychopharmacology and mechanisms of psychotropic drugs. After her internship at Imperial College London with Dr. Robin Carhart-Harris, she hopes to continue researching the psychopharmacological basis of affective disorders in her PhD.
Julian B. Renn graduated with an associate degree in Psychology at Northern Virginia Community College and with an International Bachelor in Psychology at Leiden University. After specializing in forensic and clinical psychology, he is currently working at the department of forensic psychiatry and psychotherapy at Regensburg University (under the supervision of Prof. Dr. Michael Osterheider).
Pauline Lucke obtained her Bachelor of Science in Psychology at Leiden University in 2017. She did her Bachelor’s in Psychology at Leiden University, during which she conducted research on borderline personality and intimate partner violence under the supervision of Dr. A. Krause-Utz. Before that, she finished her training as a social care worker with a focus on biographical work with people with disabilities in Berlin, Germany.
Antonia Z. Wöhlke obtained her Master of Science in Psychology at Leiden University in 2018. For her master thesis, she collected data and wrote her article about borderline personality and intimate partner violence under the supervision of Dr. A. Krause-Utz.
Charlotte C. van Schie is currently doing her PhD on social interactions and identity disturbances in borderline personality disorder, studying affective as well as neural processes using neuroimaging. Particularly, she is interested in the role of social interactions and autobiographical memory in constructing a self and the difficulties that may arise from disturbances in the self. Her PhD is under supervision of Prof. Dr. Bernet Elzinga, Prof. Dr. Serge Rombouts, and Prof. Dr. Willem Heiser at Leiden University. She is interested in using advanced statistical methods to elucidate the nuances in the data. Furthermore, she visited the INRIA lab of Gael Varoquaux and Bertrand Thirion to expand her skills in machine learning techniques as an alternative tool to analyze functional magnetic resonance imaging (fMRI) data.
Joanne Mouthaan (*1979) is currently working as assistant professor in clinical psychology at Leiden University. Main areas of her research are psychological trauma and e-health. Her work focuses on predictors, early intervention and prevention of posttraumatic stress disorder (PTSD), and other trauma-related disorders in hospital patients, uniformed services, and rescue workers. Part of her PhD thesis was a randomized controlled trial into the effectiveness of an online early psychological intervention in preventing PTSD in injury patients. As an assistant professor in the clinical psychology department of Leiden University, she teaches and supervises Bachelor, Master and postdoctoral students and studies the broad effects of trauma(-related stress) in clinical and subclinical populations.
Sufficient English proficiency was defined as ability to understand the main points of clear standard input on familiar matters regularly encountered in work, school, and leisure, as checked before and after the survey.
Authors’ Note: Annegret Krause-Utz and Lea J. Mertens contributed equally for this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
References
- Afifi T. O., MacMillan H., Cox B. J., Asmundson G. J., Stein M. B., Sareen J. (2009). Mental health correlates of intimate partner violence in marital relationships in a nationally representative sample of males and females. Journal of Interpersonal Violence, 24, 1398-1417. doi: 10.1177/0886260508322192 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Archer J. (2000). Sex differences in aggression between heterosexual partners: A meta-analytic review. Psychological Bulletin, 126, 651-680. doi: 10.1037//0033-2909.126.5.651 [DOI] [PubMed] [Google Scholar]
- Armenti N. A., Snead A. L., Babcock J. C. (2018). Exploring the moderating role of problematic substance use in the relations between borderline and antisocial personality features and intimate partner violence. Violence Against Women, 24, 223-240. doi: 10.1177/1077801216687875 [DOI] [PubMed] [Google Scholar]
- Arntz A., van Genderen H. (2009). Schema therapy for borderline personality disorders. Chichester, UK: Wiley-Blackwell. [Google Scholar]
- Baker J. (2009). Adult recall of childhood psychological maltreatment: Definitional strategies and challenges. Children and Youth Services Review, 31, 7703-7714. doi: 10.1016/j.childyouth.2009.03.001 [DOI] [Google Scholar]
- Ball J. S., Links P. S. (2009). Borderline personality disorder and childhood trauma: Evidence for a causal relationship. Current Psychiatry Reports, 11, 63-68. doi: 10.1007/s11920-009-0010-4 [DOI] [PubMed] [Google Scholar]
- Bandura A. (1973). Aggression: A social learning analysis. Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Baron R. M., Kenny D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173-1182. doi: 10.1037/0022-3514 [DOI] [PubMed] [Google Scholar]
- Battle C. L., Shea M. T., Johnson D. M., Yen S., Zlotnick C., Zanarini M. C., . . . Morey L. C. (2004). Childhood maltreatment associated with adult personality disorders: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Personality Disorders, 18, 193-211. doi: 10.1521/pedi.18.2.193.32777 [DOI] [PubMed] [Google Scholar]
- Bernstein D. P., Fink L. (1998). Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Bradley R., Conklin C. Z., Westen D. (2005). The borderline personality diagnosis in adolescents: Gender differences and subtypes. Journal of Child Psychology and Psychiatry, 46, 1006-1019. doi: 10.1111/j.1469-7610.2004.00401.x [DOI] [PubMed] [Google Scholar]
- Cackowski S., Krause-Utz A., Van Eijk J., Klohr K., Daffner S., Sobanski E., Ende G. (2017). Anger and aggression in borderline personality disorder and attention deficit hyperactivity disorder—Does stress matter? Borderline Personality Disorder & Emotion Dysregulation, 4, Article 6. doi: 10.1186/s40479-017-0057-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cackowski S., Reitz A., Ende G., Kleindienst N., Bohus M., Schmahl C., Krause-Utz A. (2014). Impact of stress on different components of impulsivity in borderline personality disorder. Psychological Medicine, 44, 3329-3340. doi: 10.1017/S0033291714000427 [DOI] [PubMed] [Google Scholar]
- Cameranesi M. (2016). Battering typologies, attachment insecurity, and personality disorders: A comprehensive literature review. Aggression and Violent Behavior, 28, 29-46. doi: 10.1016/j.avb.2016.03.005 [DOI] [Google Scholar]
- Capaldi D. M., Knoble N. B., Shortt J. W., Kim H. K. (2012). A systematic review of risk factors for intimate partner violence. Partner Abuse, 3, 231-280. doi: 10.1891/1946-6560.3.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capaldi D. M., Shortt J. W., Kim H. K., Wilson J., Crosby L., Tucci S. (2009). Official incidents of domestic violence: Types, injury, and associations with nonofficial couple aggression. Violence and Victims, 24, 502-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappell C., Heiner R. B. (1990). The intergenerational transmission of family aggression. Journal of Family Violence, 5, 135-152. doi: 10.1007/BF00978516 [DOI] [Google Scholar]
- Clift R. J., Dutton D. G. (2011). The abusive personality in women in dating relationships. Partner Abuse, 2, 166-188. doi: 10.1891/1946-6560.2.2.166 [DOI] [Google Scholar]
- Collins N. L., Read S. J. (1990). Revised Adult Attachment Scale. Los Angeles: Department of Psychology, University of Southern California. [Google Scholar]
- Crowell S. E., Beauchaine T. P., Linehan M. M. (2009). A biosocial developmental model of borderline personality: Elaborating and extending Linehan’s theory. Psychological Bulletin, 135, 495-510. doi: 10.1037/a0015616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries K. M., Mak J. M., Bacchus L. J., Child J. C., Falder G., Petzold M., . . . Watts C. H. (2013). Intimate partner violence and incident depressive symptoms and suicide attempts: A systematic review of longitudinal studies. PLoS Medicine, 10(5), e1001439. doi: 10.1371/journal.pmed.1001439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton D. G. (2002). Personality dynamics of intimate abusiveness. Journal of Psychiatric Practice, 8, 216-228. doi: 10.1097/00131746-200207000-00005 [DOI] [PubMed] [Google Scholar]
- Dutton D. G., Lane R. A., Koren T., Bartholomew K. (2016). Secure base priming diminishes conflict-based anger and anxiety. PLoS ONE, 11(9), e0162374. doi: 10.1371/journal.pone.0162374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutton D. G., Tetreault C., Karakanta C., White K. (2015). Violent offenders: Understanding and assessment. In Pietz C. A., Mattson C. A. (Eds.), Psychological factors in intimate partner violence (pp. 186-215). New York, NY: Oxford University Press. [Google Scholar]
- Dutton D. G., White K. R. (2012). Attachment insecurity and intimate partner violence. Aggression and Violent Behavior, 17, 475-481. doi: 10.1016/j.avb.2012.07.003 [DOI] [Google Scholar]
- Emmelkamp P. M., Kamphuis J. H. (2007). Personality disorders. Hove, UK: Psychology Press. [Google Scholar]
- Fonagy P., Bateman A. (2008). The development of borderline personality disorder—A mentalizing model. Journal of Personality Disorders, 22(1), 4-21. [DOI] [PubMed] [Google Scholar]
- Franklin C. A., Kercher G. A. (2012). The intergenerational transmission of intimate partner violence: Differentiating correlates in a random community sample. Journal of Family Violence, 27, 189-199. doi: 10.1007/s10896-012-9419-3 [DOI] [Google Scholar]
- Garnefski N., Kraaij V. (2006). Cognitive Emotion Regulation Questionnaire—Development of a short 18-item version (CERQ-short). Personality and Individual Differences, 41, 1045-1053. doi: 10.1016/j.paid.2006.04.010 [DOI] [Google Scholar]
- Garnefski N., Kraaij V., Spinhoven P. (2001). Negative life events, cognitive emotion regulation and emotional problems. Personality & Individual Differences, 30, 1311-1327. doi: 10.1016/S0191-8869(00)00113-6 [DOI] [Google Scholar]
- Gerhart J. I., Holman K., Seymour B., Dinges B., Ronan G. F. (2015). Group process as a mechanism of change in the group treatment of anger and aggression. International Journal of Group Psychotherapy, 65, 180-208. doi: 10.1521/ijgp.2015.65.2.180 [DOI] [PubMed] [Google Scholar]
- Gerhart J. I., Ronan G. F., Russ E., Seymour B. (2013). The moderating effects of cluster B personality traits on violence reduction training: A mixed-model analysis. Journal of Interpersonal Violence, 28, 45-61. doi: 10.1177/0886260512448849 [DOI] [PubMed] [Google Scholar]
- Gilbert R., Widom C. S., Browne K., Fergusson D., Webb E., Janson S. (2009). Burden and consequences of child maltreatment in high-income countries. The Lancet, 373(9657), 68-81. doi: 10.1016/S0140-6736(08)61706-7 [DOI] [PubMed] [Google Scholar]
- Golier J. A., Yehuda R., Bierer L. M., Mitropoulou V., New A. S., Schmeidler J., . . . Siever L. J. (2003). The relationship of borderline personality disorder to posttraumatic stress disorder and traumatic events. American Journal of Psychiatry, 160, 2018-2024. doi: 10.1176/appi.ajp.160.11.2018 [DOI] [PubMed] [Google Scholar]
- González R. A., Igoumenou A., Kallis C., Coid J. W. (2016). Borderline personality disorder and violence in the UK population: Categorical and dimensional trait assessment. BMC Psychiatry, 16, Article 180. doi: 10.1186/s12888-016-0885-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham J. M., Unterschute M. S. (2015). A reliability generalization meta-analysis of self-report measures of adult attachment. Journal of Personality Assessment, 97, 31-41. doi: 10.1080/00223891.2014.927768 [DOI] [PubMed] [Google Scholar]
- Grant B. F., Chou S. P., Goldstein R. B., Huang B., Stinson F. S., Saha T. D., . . . Ruan W. J. (2008). Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 69, 533-545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz K., Roemer L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26, 41-54. [Google Scholar]
- Hatkevich C., Mellick W., Reuter T., Temple J. R., Sharp C. (2020). Dating violence victimization, nonsuicidal self-injury, and the moderating effect of borderline personality disorder features in adolescent inpatients. Journal of Interpersonal Violence, 35(15-16), 3124-3147. [DOI] [PubMed] [Google Scholar]
- Hayes A. F. (2013). Introduction to mediation, moderation, and conditional process analysis—A regression-based approach. New York, NY: Guilford Press. [Google Scholar]
- Herman J. L., Perry J. C., van der Kolk B. A. (1989). Childhood trauma in borderline personality disorder. American Journal of Psychiatry, 146, 490-495. doi: 10.1176/ajp.146.4.490 [DOI] [PubMed] [Google Scholar]
- Hines D. (2008). Borderline personality traits and intimate partner aggression: An international multisite, cross-gender analysis. Psychology of Women Quarterly, 32, 290-302. doi: 10.1111/j.1471-6402.2008.00437.x [DOI] [Google Scholar]
- Hughes F. M., Stuart G. L., Gordon K. C., Moore T. M. (2007). Predicting the use of aggressive conflict tactics in a sample of women arrested for domestic violence. Journal of Social and Personal Relationships, 2, 155-176. doi: 10.1177/0265407507075406 [DOI] [Google Scholar]
- Jackson K. M., Trull T. J. (2001). The factor structure of the Personality Assessment Inventory-Borderline Features (PAI-BOR) Scale in a nonclinical sample. Journal of Personality Disorders, 15, 536-545. doi: 10.1521/pedi.15.6.536.19187 [DOI] [PubMed] [Google Scholar]
- Jackson M. A., Sippel L. M., Mota N., Whalen D., Schumacher J. A. (2015). Borderline personality disorder and related constructs as risk factors for intimate partner violence perpetration. Aggression and Violent Behavior, 24, 95-106. doi: 10.1016/j.avb.2015.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings W. G., Richards T. N., Tomsich E., Gover A. R. (2015). Investigating the role of child sexual abuse in intimate partner violence victimization and perpetration in young adulthood from a propensity score matching approach. Journal of Child Sexual Abuse, 24, 659-681. doi: 10.1080/10538712.2015.1057665 [DOI] [PubMed] [Google Scholar]
- Johnson W. L., Giordano P. C., Manning W. D., Longmore M. A. (2015). The age-IPV curve: Changes in the perpetration of intimate partner violence during adolescence and young adulthood. Journal of Youth and Adolescence, 44, 708-726. doi: 10.1007/s10964-014-0158-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H. K., Laurent H. K., Capaldi D. M., Feingold A. (2008). Men’s aggression toward women: A 10-year panel study. Journal of Marriage and the Family, 70, 1169-1187. doi: 10.1111/j.1741-3737.2008.00558.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause-Utz A., Cackowski S., Daffner S., Sobanski E., Plichta M. M., Bohus M., . . . Schmahl C. (2016). Delay discounting and response disinhibition under acute experimental stress in women with borderline personality disorder and adult attention deficit hyperactivity disorder. Psychological Medicine, 46, 3137-3149. doi: 10.1017/S0033291716001677 [DOI] [PubMed] [Google Scholar]
- Krause-Utz A., Niedtfeld I., Knauber J., Schmahl C. (2017). Neurobiology in borderline personality disorder. In Stanley B., New A. (Eds.), Primer on borderline personality disorder (pp. 83-111). New York, NY: Oxford University Press. [Google Scholar]
- Krause-Utz A., Sobanski E., Alm B., Valerius G., Kleindienst N. B. M., Schmahl C. (2013). Impulsivity in relation to stress in patients with borderline personality disorder with and without co-occurring attention-deficit/hyperactivity disorder: An exploratory study. Journal of Nervous and Mental Disease, 201, 116-123. doi: 10.1097/NMD.0b013e31827f6462 [DOI] [PubMed] [Google Scholar]
- Lawson D. M., Brossart D. F. (2013). Interpersonal problems and personality features as mediators between attachment and intimate partner violence. Violence and Victims, 28, 414-428. doi: 10.1891/0886-6708.VV-D-12-00031 [DOI] [PubMed] [Google Scholar]
- Lazarus R. S., Folkman S. (1984). Stress, appraisal, and coping. New York, NY: Springer. [Google Scholar]
- Lieb K., Zanarini M. C., Schmahl C., Linehan M. M., Bohus M. (2004). Borderline personality disorder. The Lancet, 364, 453-461. doi: 10.1016/s0140-6736(04)16770-6 [DOI] [PubMed] [Google Scholar]
- Linder J. R., Collins W. A. (2005). Parent and peer predictors of physical aggression and conflict management in romantic relationships in early adulthood. Journal of Family Psychology, 19, 252-262. [DOI] [PubMed] [Google Scholar]
- Linehan M. (1993). Diagnosis and Treatment of Mental Disorders. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press. [Google Scholar]
- Maneta E. K., Cohen S., Schulz M. S., Waldinger R. J. (2013). Two to tango: A dyadic analysis of links between borderline personality traits and intimate partner violence. Journal of Personality Disorders, 27, 233-243. doi: 10.1521/pedi.2013.27.2.233 [DOI] [PubMed] [Google Scholar]
- Martin R., Dahlen E. (2005). Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences, 39, 1249-1260. [Google Scholar]
- Mauricio A. M. (2007). Borderline and antisocial personality scores as mediators between attachment and intimate partner violence. Violence and Victims, 22, 139-157. doi: 10.1891/088667007780477339 [DOI] [PubMed] [Google Scholar]
- McKeown A. (2014). Attachment, personality and female perpetrators of intimate partner violence. Journal of Forensic Psychiatry & Psychology, 25, 556-573. doi: 10.1080/14789949.2014.943792 [DOI] [Google Scholar]
- McMahon K., Hoertel N., Wall M. M., Okuda M., Limosin F., Blanco C. (2015). Childhood maltreatment and risk of intimate partner violence: A national study. Journal of Psychiatric Research, 69, 42-49. doi: 10.1016/j.jpsychires.2015.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore K. E., Gobin R. L., McCauley H. L., Kao C. W., Anthony S. M., Kubiak S., . . . Johnson J. E. (2018). The relation of borderline personality disorder to aggression, victimization, and institutional misconduct among prisoners. Comprehensive Psychiatry, 84, 15-21. doi: 10.1016/j.comppsych.2018.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey L. C. (1991). Personality Assessment Inventory. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Newhill C. E., Eack S. M., Mulvey E. P. (2009). Violent behavior in borderline personality. Journal of Personality Disorders, 23, 541-554. doi: 10.1521/pedi.2009.23.6.541 [DOI] [PubMed] [Google Scholar]
- Ochsner K. N., Gross J. J. (2005). The cognitive control of emotion. Trends in Cognitive Science, 9, 242-249. doi: 10.1016/j.tics.2005.03.010 [DOI] [PubMed] [Google Scholar]
- Peterman A., Bleck J., Palermo T. (2015). Age and intimate partner violence: An analysis of global trends among women experiencing victimization in 30 developing countries. Journal of Adolescent Health, 57, 624-630. doi: 10.1016/j.jadohealth.2015.08.008 [DOI] [PubMed] [Google Scholar]
- Peters J. R., Derefinko K. J., Lynam D. R. (2017). Negative urgency accounts for the association between borderline personality features and intimate partner violence in young men. Journal of Personality Disorders, 31, 16-25. doi: 10.1521/pedi_2016_30_234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrek C., Elbert T., Weierstall R., Müller O., Rockstroh B. (2013). Childhood adversities in relation to psychiatric disorders. Psychiatry Research, 206, 103-110. doi: 10.1016/j.psychres.2012.11.003 [DOI] [PubMed] [Google Scholar]
- Reuter T. R., Sharp C., Temple J. R., Babcock J. C. (2014). The relation between borderline personality disorder features and teen dating violence. Psychology of Violence, 5, 163-173. doi: 10.1037/a0037891 [DOI] [Google Scholar]
- Riggs D. S., Caulfield M. B., Street A. E. (2000). Risk for domestic violence: Factors associated with perpetration and victimization. Journal of Clinical Psychology, 56, 1289-1316. doi: [DOI] [PubMed] [Google Scholar]
- Ross J. M., Babcock J. C. (2009). Proactive and reactive violence among intimate partner violent men diagnosed with antisocial and borderline personality disorder. Journal of Family Violence, 24, 607-617. doi: 10.1007/s10896-009-9259-y [DOI] [Google Scholar]
- Sansone R. A., Sansone L. A. (2010). Measuring self-harm behavior with the Self-Harm Inventory. Psychiatry, 7(4), 16-20. [PMC free article] [PubMed] [Google Scholar]
- Scott L. N., Stepp S. D., Pilkonis P. A. (2014). Prospective associations between features of borderline personality disorder, emotion dysregulation, and aggression. Personality Disorders: Theory, Research, and Treatment, 5, 278-288. doi: 10.1037/per0000070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott L. N., Wright A. G., Beeney J. E., Lazarus S. A., Pilkonis P. A., Stepp S. D. (2017). Borderline personality disorder symptoms and aggression: A within-person process model. Journal of Abnormal Psychology, 126, 429-440. doi: 10.1037/abn0000272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soloff P. H., Chiappetta L. (2018). Time, age, and predictors of psychosocial outcome in borderline personality disorder. Journal of Personality Disorders, 4, 1-16. doi: 10.1521/pedi_2018_32_386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiglmayr C. E., Grathwol T., Linehan M. M., Ihorst G., Fahrenberg J., Bohus M. (2005). Aversive tension in patients with borderline personality disorder: A computer-based controlled field study. Acta Psychiatrica Scandinavica, 111, 372-379. doi: 10.1111/j.1600-0447.2004.00466.x [DOI] [PubMed] [Google Scholar]
- Stith S. M., Rosen K. H., Middleton K. A., Busch A. L., Lundeberg K., Carlton R. P. (2000). The intergenerational transmission of spouse abuse: A meta-analysis. Journal of Marriage and the Family, 62, 640-654. [Google Scholar]
- Stith S. M., Smith D. B., Penn C. E., Ward D. B., Tritt D. (2004). Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggression and Violent Behavior, 10, 65-98. doi: 10.1016/j.avb.2003.09.001 [DOI] [Google Scholar]
- Straus M. A. (2004). Scoring the CTS2 and CTSPC. Family Research Laboratory, University of New Hampshire. Retrieved from http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.295.2407&rep=rep1&type=pdf [Google Scholar]
- Straus M. A., Hamby S. L., Boney-McCoy S., Sugarman D. B. (1996). The revised Conflict Tactics Scales (CTS2): Development an preliminary psychometric data. Journal of Family Issues, 17, 283-316. doi: 10.1177/019251396017003001 [DOI] [Google Scholar]
- Swinford S. P., DeMaris A., Cernkovich S. A., Giordano P. C. (2000). Harsh physical discipline in childhood and violence in later romantic involvements: The mediating role of problem behaviors. Journal of Marriage and the Family, 62, 508-519. [Google Scholar]
- Walker L. E. (1977). Battered women and learned helplessness. Victimology, 2, 525-534. [Google Scholar]
- Weinstein Y., Gleason M. E. J., Oltmanns T. F. (2012). Borderline but not antisocial personality disorder symptoms are related to self-reported partner aggression in late middle-age. Journal of Abnormal Psychology, 121, 692-698. doi: 10.1037/a0028994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman M. A., Schonbrun Y. C. (2009). Social consequences of borderline personality disorder symptoms in a population-based survey: Marital distress, marital violence, and marital disruption. Journal of Personality Disorders, 23, 410-415. [DOI] [PubMed] [Google Scholar]
- Whitaker D. J., Haileyesus T., Swahn M., Saltzman L. S. (2007). Differences in frequency of violence and reported injury between relationships with reciprocal and nonreciprocal intimate partner violence. American Journal of Public Health, 97, 941-947. doi: 10.2105/ajph.2005.079020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitfield C. L., Anda R. F., Dube S. R., Felitti V. J. (2003). Violent childhood experiences and the risk of intimate partner violence in adults: Assessment in a large health maintenance organization. Journal of Interpersonal Violence, 18, 166-185. [Google Scholar]
- Widom C. S., Czaja S., Dutton M. A. (2014). Child abuse and neglect and intimate partner violence victimization and perpetration: A prospective investigation. Child Abuse & Neglect, 38, 650-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willie T. C., Powell A., Callands T., Sipsma H., Peasant C., Magriples U., . . . Kershaw T. (2019). Investigating intimate partner violence victimization and reproductive coercion victimization among young pregnant and parenting couples: A longitudinal study. Psychology of Violence, 9(3), 278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen S., Shea M. T., Battle C. L., Johnson D. M., Zlotnick C., Dolan-Sewell R., . . . McGlashan T. H. (2002). Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant, and obsessive-compulsive personality disorders: Findings from the collaborative longitudinal personality disorders study. The Journal of Nervous and Mental Disease, 190, 510-518. doi: 10.1097/01.NMD.0000026620.66764.78 [DOI] [PubMed] [Google Scholar]
- Yeomans F. E., Clarkin J. F., Kernberg O. F. (2015). Transference-focused psychotherapy for borderline personality disorder: A clinical guide (1st ed.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Young J. E. (1990). Cognitive therapy for personality disorders: A schema-focused approach. Sarasota, FL: Professional Resource Exchange. [Google Scholar]
- Zanarini M. C. (2000). Childhood experiences associated with the development of borderline personality disorder. The Psychiatric Clinics of North America, 23, 89-101. doi: 10.1016/S0193-953X(05)70145-3 [DOI] [PubMed] [Google Scholar]
- Zimet G. D., Powell S. S., Farley G. K., Werkman S., Berkoff K. A. (1990). Psychometric characteristics of the multidimensional scale of perceived social support. Journal of Personality Assessment, 55, 610-617. [DOI] [PubMed] [Google Scholar]
- Zlotnick C., Rothschild L., Zimmerman M. (2002). The role of gender in the clinical presentation of patients with borderline personality disorder. Journal of Personality Disorders, 16, 277-282. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_Tables_2-6 for Childhood Maltreatment, Borderline Personality Features, and Coping as Predictors of Intimate Partner Violence by Annegret Krause-Utz, Lea J. Mertens, Julian B. Renn, Pauline Lucke, Antonia Z. Wöhlke, Charlotte C. van Schie and Joanne Mouthaan in Journal of Interpersonal Violence
Supplemental material, Supplemental_Table_1 for Childhood Maltreatment, Borderline Personality Features, and Coping as Predictors of Intimate Partner Violence by Annegret Krause-Utz, Lea J. Mertens, Julian B. Renn, Pauline Lucke, Antonia Z. Wöhlke, Charlotte C. van Schie and Joanne Mouthaan in Journal of Interpersonal Violence


