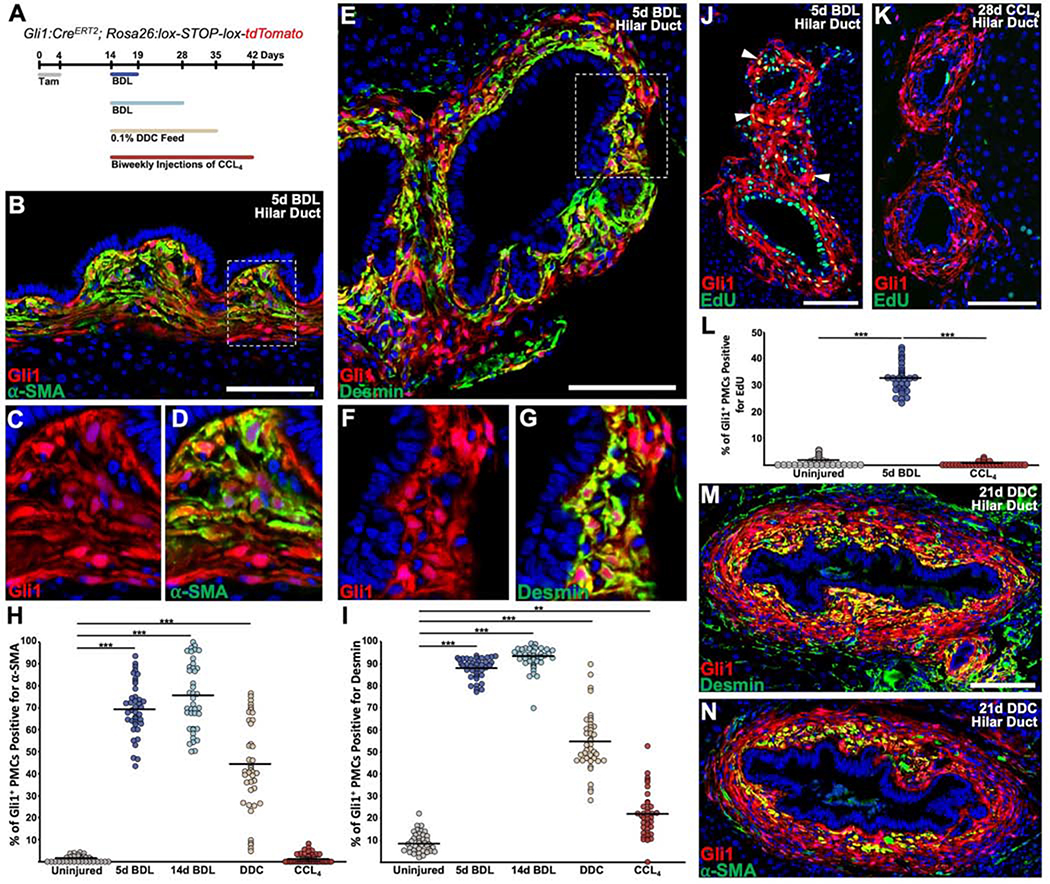
Figure 3. Cholestatic injury causes activation and proliferation of Gli1+ PMCs around hilar ducts.
(A) Experimental scheme. Tamoxifen was administered daily for 4 doses, followed by a 10 day washout. Subsequently, animals underwent the described injuries and were analyzed at the indicated timepoint. (B) α-SMA was strongly induced within Gli1+ PMCs 5 days post BDL, particularly within mesenchymal cells adjacent to cholangiocytes. (C, D) Zoom of dash box in (B), where Gli1+ PMCs are seen to colocalize with α-SMA. (E) Desmin was induced within Gli1+ PMCs 5 days post BDL in a similar pattern to α-SMA. (F, G) Zoom of dash box in (B), where Gli1+ PMCs are seen to colocalize with desmin. (H, I) Quantification of the percentages of Gli1+ PMCs that are positive for α-SMA (H) or desmin (I). (J) Gli1+ PMCs incorporate EdU 5 days post BDL (arrowhead). (K) Gli1+ PMCs do not show EdU incorporation after CCL4. (L) Percentage of Gli1+ EdU+ PMCs 5 days post BDL and 28 days post CCL4. (M, N) After 21 days of 0.1% DDC diet, large ducts have numerous layers of Gli1+ PMCs, with desmin and α-SMA restricted primarily to the innermost layer of mesenchymal cells (n = 4 for all experiments). ***P<0.001; **P<0.05. Scale bars, 100 μm.